Back to Journals » Journal of Inflammation Research » Volume 18
White Blood Cell Count Is Associated with Hyperuricemia in Patients with Type 2 Diabetes Mellitus
Authors Peng YF, Yin H, Hu L, Fang L, Jia DR, Li L
Received 23 October 2024
Accepted for publication 6 February 2025
Published 17 March 2025 Volume 2025:18 Pages 3993—3999
DOI https://doi.org/10.2147/JIR.S501890
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
You-Fan Peng,1,2,* Han Yin,3,* Lin Hu,3 Li Fang,4 Dian-Rong Jia,5 Ling Li3,6
1Department of Respiratory and Critical Care Medicine, Affiliated Hospital of Youjiang Medical University for Nationalities, Baise, People’s Republic of China; 2Life Science and Clinical Medicine Research Center, Affiliated Hospital of Youjiang Medical University for Nationalities, Baise, People’s Republic of China; 3Department of Endocrinology, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, People’s Republic of China; 4Department of Endocrinology, Nanjing Gaochun Hospital of Traditional Chinese Medicine, Nanjing, People’s Republic of China; 5Department of Endocrinology, Taizhou Jiangyan Hospital of Traditional Chinese Medicine, Taizhou, People’s Republic of China; 6Pancreatic Research Institute, Southeast University, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ling Li, Department of Endocrinology, Zhongda Hospital, School of Medicine, Southeast University, No. 87 Dingjiaqiao, Nanjing, Jiangsu, 210009, People’s Republic of China, Email [email protected] Dian-Rong Jia, Department of Endocrinology, Taizhou Jiangyan Hospital of Traditional Chinese Medicine, No. 699 Jiangyan Avenue, Taizhou, Jiangsu, 225500, People’s Republic of China, Email [email protected]
Background: Hyperuricemia is highly prevalent among patients with type 2 diabetes mellitus (T2DM). Inflammation is associated with the process of hyperuricemia. However, it is unclear whether white blood cell (WBC) count, a convenient inflammatory marker, is associated with hyperuricemia in patients with T2DM. Thus, we aimed to explore the possible association between WBC count and hyperuricemia in patients with T2DM.
Methods: A total of 1768 patients with T2DM were retrospectively included. Cumulative data were analyzed in patients with T2DM.
Results: WBC count was significantly elevated in T2DM patients with hyperuricemia compared with those without hyperuricemia (6.80 [5.60, 8.02] vs 6.20 [5.27, 7.24] 109/L, p< 0.001). There was a significant positive correlation between WBC count and serum UA levels in patients with T2DM (r=0.165, 95% CI: [0.118, 0.211], p< 0.001). Multivariable logistic regression analysis revealed an independent association between WBC count and hyperuricemia in patients with T2DM (OR=1.185, 95% CI: [1.077, 1.303], p< 0.001).
Conclusion: Elevated WBC count, even within the normal range, is associated with hyperuricemia in patients with T2DM, suggesting that chronic inflammation, as indicated by a higher WBC count, may be related to the development of hyperuricemia in patients with T2DM and urate-lowering therapy may be helpful to ameliorate chronic inflammatory damage in T2DM patients with hyperuricemia.
Keywords: type 2 diabetes mellitus, hyperuricemia, white blood cell, inflammation
Introduction
Type 2 diabetes mellitus (T2DM) is a disease characterized by impaired insulin secretion or a failure of tissues to respond to insulin.1 The prevalence of T2DM maintains an increased trend globally, and the escalating burden of T2DM has become a significant concern within the healthcare domain.2 The chronic complications of T2DM mainly include macrovascular and microvascular manifestations, such as cardiovascular disease, retinopathy, nephropathy, and neuropathy, which seriously affect patient’s quality of life.3,4 Hyperuricemia, a purine metabolic disorder, has emerged as a significant public health burden.5 Accumulating evidences have reported that the prevalence of hyperuricemia is high among patients with T2DM.6–8 It has been suggested that inflammation is associated with in the process of hyperuricemia.9
White blood cell (WBC) count is a convenient marker for assessing inflammation.10 The variations in WBC subtypes have been associated with multiple diseases, including coronary heart disease, ischemic stroke, and cancer.11–13 Convincing evidence has demonstrated that WBC count is positively correlated with uric acid (UA) in patients with preeclampsia.14 It has been found that WBC count is positively associated with elevated serum UA levels in females who live in high-altitude regions.15 There has been a positive correlation between WBC count and serum UA levels in adolescents with hyperuricemia.16 In addition, an increased WBC count has been proposed as an important biological marker of hyperuricemia in an adult population.17 Even more importantly, an elevated WBC count has been reported to be associated with hyperuricemia independently of conventional risk factors for chronic kidney disease,18 though the mechanism of inflammation is a crucial factor in kidney injury.19 However, to our knowledge, the association between WBC count and hyperuricemia still remains unknown in patients with T2DM. Hence, the aim of this study was to examine the possible association between WBC count and hyperuricemia in patients with T2DM.
Methods
Patients
A total of 1768 T2DM patients who visited the National Metabolic Management Center, Zhongda Hospital, Southeast University were retrospectively included from January 2021 to March 2023. The diagnosis of T2DM was determined according to the American Diabetes Association criteria.20 Hyperuricemia was defined as serum UA levels >420 µmol/L in males and >360 µmol/L in females.21 To minimize potential factors that affected WBC count, T2DM patients with a WBC count outside the normal range were excluded from the study. Moreover, T2DM patients with missing data for the included variables were also excluded from the analysis. The study was approved by the Ethics Committee of Zhongda Hospital, Southeast University, and was conducted in compliance with the Declaration of Helsinki. Due to the retrospective nature of this study, the requirement for informed consent of patients was waived by the Ethics Committee of Zhongda Hospital, Southeast University. The data of patients were maintained with confidentiality.
Data Extraction
We extracted the following data: (a) sex, age, height, and weight; (b) medical history; (c) the results of laboratory examinations including WBC count, fasting blood glucose (FBG), hemoglobin A1c (HbA1c), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), creatinine (Cr), and UA. The laboratory examinations were carried out after overnight fasting. Body mass index (BMI) was calculated as weight in kilogram divided by the square of height in meter.
Statistical Analysis
Continuous variables are expressed as median and interquartile range due to non-normally distribution, and categorical variables are expressed as frequency and percentage. Chi-square test was employed to compare the differences in categorical variables, and Mann–Whitney U-test was used to compare the differences in continuous variables. Spearman correlation analysis was used to assess the correlation between the two continuous variables. Univariable logistic regression analysis was used to examine which variables were associated with hyperuricemia in patients with T2DM. Multivariable logistic regression analysis was performed to determine the independent factors associated with hyperuricemia in patients with T2DM. A p value of 0.05 was considered to indicate statistical significance. The data were analyzed by SPSS version 29.0 (IBM, Corporation, Armonk, NY, USA).
Results
The Characteristics of T2DM Patients With Hyperuricemia and Those Without Hyperuricemia
The characteristics were compared between T2DM patients with hyperuricemia and those without hyperuricemia (Table 1). WBC count was significantly higher in T2DM patients with hyperuricemia than in those without hyperuricemia (6.80 [5.60, 8.02] vs 6.20 [5.27, 7.24] 109/L, p<0.001). Moreover, there were significant differences with respect to age (p=0.002), BMI (p<0.001), hypertension history (p<0.001), TG (p<0.001), HDL-C (p<0.001), and Cr (p<0.001) between the groups. No significant differences were observed in gender (p=0.287), coronary heart disease history (p=0.105), FBG (p=0.144), HbA1c (p=0.208), TC (p=0.661), and LDL-C (p=0.120) between the groups.
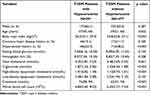 |
Table 1 The Characteristics of T2DM Patients with Hyperuricemia and Those without Hyperuricemia |
The Correlation Between WBC Count and Serum UA Levels in Patients With T2DM
The correlation analysis between WBC count and continuous variables was conducted in patients with T2DM (Table 2). WBC count was significantly positively correlated with serum UA levels in patients with T2DM (r=0.165, 95% CI: [0.118, 0.211], p<0.001) (Figure 1). WBC count was also found to be significantly positively correlated with BMI (r=0.141, 95% CI: [0.094, 0.188], p<0.001), FBG (r=0.093, 95% CI: [0.045, 0.140], p<0.001), HbA1c (r=0.095, 95% CI: [0.047, 0.142], p<0.001), TG (r=0.156, 95% CI: [0.109, 0.203], p<0.001), and Cr (r=0.081, 95% CI: [0.033, 0.128], p<0.001), and significantly negatively correlated with age (r=−0.083, 95% CI: [−0.130,-0.035], p<0.001) and HDL-C (r=−0.164, 95% CI: [−0.210,-0.117], p<0.001) except for TC (r=0.011, 95% CI: [−0.037, 0.059], p=0.648) and LDL-C (r=0.003, 95% CI: [−0.045, 0.051], p=0.899) in patients with T2DM.
 |
Table 2 The Correlation Between WBC Count and Continuous Variables in Patients with T2DM |
 |
Figure 1 The correlation between WBC count and UA in patients with T2DM. Abbreviation: WBC, white blood cell; UA, uric acid; T2DM, type 2 diabetes mellitus; CI, confidence interval. |
The Independent Association Between WBC Count and Hyperuricemia in Patients With T2DM
The univariable and multivariable logistic regression analyses were conducted in patients with T2DM (Table 3). Univariable logistic regression analysis found that WBC ount (OR=1.279, 95% CI: [1.170, 1.399], p<0.001), age (OR=0.978, 95% CI: [0.968, 0.989], p<0.001), BMI (OR=1.118, 95% CI: [1.084, 1.154], p<0.001), hypertension history (OR=1.903, 95% CI: [1.467, 2.469], p<0.001), TG (OR=1.098, 95% CI: [1.053, 1.146], p<0.001), HDL-C (OR=0.252, 95% CI: [0.159, 0.398], p<0.001), and Cr (OR=1.011, 95% CI: [1.007, 1.015], p<0.001) were significantly associated with hyperuricemia in patients with T2DM. After adjustment for gender, age, BMI, coronary heart disease history, hypertension history, FBG, HbA1c, TC, TG, HDL-C, LDL-C, and Cr, multivariable logistic regression analysis revealed that WBC count was independently associated with hyperuricemia in patients with T2DM (OR=1.185, 95% CI: [1.077, 1.303], p<0.001), and that gender (OR=0.535, 95% CI: [0.394, 0.727], p<0.001), age (OR=0.973, 95% CI: [0.960, 0.986], p<0.001), BMI (OR=1.054, 95% CI: [1.017, 1.092], p=0.004), hypertension history (OR=1.761, 95% CI: [1.300, 2.386], p<0.001), TG (OR=1.138, 95% CI: [1.054, 1.228], p<0.001), HDL-C (OR=0.414, 95% CI: [0.239, 0.717], p=0.002), LDL-C (OR=1.427, 95% CI: [1.044, 1.949], p=0.026), and Cr (OR=1.012, 95% CI: [1.008, 1.017], p<0.001) were also as factors independently associated with hyperuricemia in patients with T2DM.
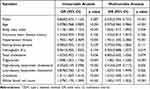 |
Table 3 Univariable and Multivariable Logistic Regression Analyses of Factors Associated with Hyperuricemia in Patients with T2DM |
Discussion
WBC count is a component of complete blood count. Our study revealed that elevated WBC count, although still within the normal range, was independently associated with hyperuricemia in patients with T2DM. WBC count, even within the normal range, is widely acknowledged to be an indicator of inflammation.10 Thus, inflammatory mechanism may mediate the association between elevated WBC count and hyperuricemia in patients with T2DM. Ruggiero C et al22 suggested a significant positive association between UA and inflammatory markers such as tumor necrosis factor-α, interleukin-6, and interleukin-18 in community-dwelling older persons. High-sensitivity C-reactive protein levels have been reported to be positively associated with the prevalence of hyperuricemia.23 It has been confirmed that urate-lowering therapy improves systemic inflammation by reducing UA in asymptomatic hyperuricemia.24 Thus, these literatures suggest that UA may activate the inflammatory response through different mechanisms. Indeed, UA triggers the inflammatory response by affecting immune cells in a hyperuricemic environment.9 UA can promote the inflammation by several intracellular signaling pathways, including ERK/p38 MAPK, AMPK, and PI3K,25 and may also induce renal inflammation by NF-κB signaling activation.26 Additional, hyperuricemia establishes a pro-inflammatory microenvironment through multiple signaling pathways, including NLRP3 inflammasome activation, JAK2/STAT3 cascade, and ROS/NRLP3/NF-κB axis.27–29 Notably, elevated levels of UA promote the formation of monosodium urate (MSU) crystals in circulation.30 Thus, the inflammatory effects of UA also depend on its precipitation into MSU crystals in the development of gout.31 Mechanistically, MSU crystals induce the production of active interleukin-1β and interleukin-18 by activating NALP3 inflammasome.32 Furthermore, MSU crystals directly stimulate tumor necrosis factor-α synthesis,33 and activateboth classical and alternative complement pathways to amplify inflammatory response.34,35 Emerging evidence indicates that MSU crystal deposits induce inflammatory response through innate immune cellular recognition for naked MSU crystals via specific Toll-like receptors.36 Thus, these molecular mechanisms collectively underscore that the formation of MSU crystals is an important factor for the inflammatory response in T2DM patients with hyperuricemia.
Established epidemiological evidence has confirmed that female gender, high BMI, and reduced estimated glomerular filtration rate are associated with hyperuricemia in patients with T2DM.37 Our results identified that female gender, high BMI, and high Cr were independently associated with hyperuricemia in patients with T2DM. Hyperuricemia has been shown to be associated with an increased risk for incident hypertension.38 Our study observed an independent association between hypertension history and hyperuricemia in patients with T2DM. Moreover, the current investigation aslo found that younger age, high TG, high LDL-C, and low HDL-C were independently associated with hyperuricemia in our study cohort.
The study has several limitations. First, the cross-sectional design inherently precludes causal inference between WBC count and hyperuricemia in patients with T2DM. Second, the association between other inflammatory markers, such as C-reactive protein, and hyperuricemia was not estimated in patients with T2DM. Third, longitudinal changes in the WBC count following urate-lowering therapy remain unknown due to the absence of interventional follow-up in T2DM patients with hyperuricemia. Fourth, residual confounders from unmeasured variables including dietary patterns, pharmacological exposures, and selection bias may infuence the observed results.
In conclusion, the study demonstrates an association between elevated WBC count, even within physiologically normal limits, and hyperuricemia in patients with T2DM. The findings suggest that chronic inflammation, reflected by increased WBC count, likely contributes to the development of hyperuricemia in patients with T2DM. Importantly, the observations support that urate-lowering therapy may offer benefits in alleviating chronic inflammatory damage in T2DM patients with hyperuricemia.
Data Sharing Statement
Data are available upon reasonable request from the corresponding author.
Ethics Approval
The study was approved by the Ethics Committee of Zhongda Hospital, Southeast University, and was conducted in compliance with the Declaration of Helsinki. Due to the retrospective nature of this study, the requirement for informed consent of patients was waived by the Ethics Committee of Zhongda Hospital, Southeast University.The data of patients were maintained with confidentiality.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mizukami H, Kudoh K. Diversity of pathophysiology in type 2 diabetes shown by islet pathology. J Diabetes Investig. 2022;13(1):6–13. doi:10.1111/jdi.13679
2. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107–111. doi:10.2991/jegh.k.191028.001
3. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. doi:10.1038/nrendo.2017.151
4. Jing X, Chen J, Dong Y, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. 2018;16(1):189. doi:10.1186/s12955-018-1021-9
5. Nutmakul T. A review on benefits of quercetin in hyperuricemia and gouty arthritis. Saudi Pharm J. 2022;30(7):918–926. doi:10.1016/j.jsps.2022.04.013
6. Alemayehu E, Fiseha T, Bambo GM, et al. Prevalence of hyperuricemia among type 2 diabetes mellitus patients in Africa: a systematic review and meta-analysis. BMC Endocr Disord. 2023;23(1):153. doi:10.1186/s12902-023-01408-0
7. Abujbara M, Al Hourani HM, Al-Raoush RI, Khader YS, Ajlouni K. Prevalence of hyperuricemia and associated factors among type 2 diabetic patients in Jordan. Int J Gen Med. 2022;15:6611–6619. doi:10.2147/IJGM.S376857
8. Arersa KK, Wondimnew T, Welde M, Husen TM. Prevalence and determinants of hyperuricemia in type 2 diabetes mellitus patients attending Jimma Medical Center, Southwestern Ethiopia, 2019. Diabetes Metab Syndr Obes. 2020;13:2059–2067. doi:10.2147/DMSO.S252825
9. Li D, Yuan S, Deng Y, et al. The dysregulation of immune cells induced by uric acid: mechanisms of inflammation associated with hyperuricemia and its complications. Front Immunol. 2023;14:1282890.
10. Chmielewski PP, Strzelec B. Elevated leukocyte count as a harbinger of systemic inflammation, disease progression, and poor prognosis: a review. Folia Morphol. 2018;77(2):171–178. doi:10.5603/FM.a2017.0101
11. Wang Y, Zhuang Y, Lin C, Hong H, Chen F, Ke J. The neutrophil-to-lymphocyte ratio is associated with coronary heart disease risk in adults: a population-based study. PLoS One. 2024;19(2):e0296838. doi:10.1371/journal.pone.0296838
12. Mao S, Hu Y, Zheng X, et al. Correlation analysis of neutrophil/albumin ratio and leukocyte count/albumin ratio with ischemic stroke severity. Cardiol Cardiovasc Med. 2023;7(1):32–38. doi:10.26502/fccm.92920305
13. Song M, Graubard BI, Loftfield E, Rabkin CS, Engels EA. White blood cell count, neutrophil-to-lymphocyte ratio, and incident cancer in the UK biobank. Cancer Epidemiol Biomarkers Prev. 2024;33(6):821–829. doi:10.1158/1055-9965.EPI-23-1145
14. Li BJ, Zhu TT, Hu XY, He CM. Uric acid as a mediator in the correlation between white blood cells and preeclampsia severity: a retrospective cohort study. Sci Rep. 2023;13(1):20161. doi:10.1038/s41598-023-47625-4
15. Cui D, Huang R, Yongzong D, et al. Gender-specific association between blood cell parameters and hyperuricemia in high-altitude areas. Front Public Health. 2024;12:1336674. doi:10.3389/fpubh.2024.1336674
16. Stelmach MJ, Szczerbinski L, Wasilewska N, Protas P, Wasilewska A. Hematological parameters in adolescents with hyperuricemia. Indian Pediatr. 2014;51(12):1003–1005. doi:10.1007/s13312-014-0547-0
17. Su P, Hong L, Zhao Y, Sun H, Li L. The association between hyperuricemia and hematological indicators in a Chinese adult population. Medicine. 2016;95(7):e2822. doi:10.1097/MD.0000000000002822
18. Liu J, Shen P, Ma X, et al. White blood cell count and the incidence of hyperuricemia: insights from a community-based study. Front Med. 2019;13(6):741–746. doi:10.1007/s11684-017-0579-7
19. Karağaç MS, Yeşilkent EN, Kizir D, et al. Esculetin improves inflammation of the kidney via gene expression against doxorubicin-induced nephrotoxicity in rats: in vivo and in silico studies. Food Biosci. 2024;62:105159. doi:10.1016/j.fbio.2024.105159
20. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of Medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl1):S14–S31. doi:10.2337/dc20-S002
21. Bardin T, Richette P. Definition of hyperuricemia and gouty conditions. Curr Opin Rheumatol. 2014;26(2):186–191. doi:10.1097/BOR.0000000000000028
22. Ruggiero C, Cherubini A, Ble A, et al. Uric acid and inflammatory markers. Eur Heart J. 2006;27(10):1174–1181. doi:10.1093/eurheartj/ehi879
23. Yang T, Ding X, Wang YL, et al. Association between high-sensitivity C-reactive protein and hyperuricemia. Rheumatol Int. 2016;36(4):561–566. doi:10.1007/s00296-016-3429-z
24. Takir M, Kostek O, Ozkok A, et al. Lowering uric acid with allopurinol improves insulin resistance and systemic inflammation in asymptomatic hyperuricemia. J Investig Med. 2015;63(8):924–929. doi:10.1097/JIM.0000000000000242
25. Kimura Y, Tsukui D, Kono H. Uric acid in inflammation and the pathogenesis of atherosclerosis. Int J mol Sci. 2021;22(22):12394. doi:10.3390/ijms222212394
26. Zhou Y, Fang L, Jiang L, et al. Uric acid induces renal inflammation via activating tubular NF-κB signaling pathway. PLoS One. 2012;7(6):e39738. doi:10.1371/journal.pone.0039738
27. Tan J, Wan L, Chen X, et al. Conjugated linoleic acid ameliorates high fructose-induced hyperuricemia and renal inflammation in rats via NLRP3 inflammasome and TLR4 signaling pathway. mol Nutr Food Res. 2019;63(12):e1801402. doi:10.1002/mnfr.201801402
28. Zhang Y, Wang S, Dai X, et al. Simiao San alleviates hyperuricemia and kidney inflammation by inhibiting NLRP3 inflammasome and JAK2/STAT3 signaling in hyperuricemia mice. J Ethnopharmacol. 2023;312:116530. doi:10.1016/j.jep.2023.116530
29. Riaz M, Al Kury LT, Atzaz N, et al. Carvacrol alleviates hyperuricemia-induced oxidative stress and inflammation by modulating the NLRP3/NF-κB pathwayt. Drug Des Devel Ther. 2022;16:1159–1170. doi:10.2147/DDDT.S343978
30. Pluta RM, Shmerling RH, Burke AE, Livingston EH. JAMA patient page. Gout. JAMA. 2012;308(20):2161. doi:10.1001/jama.2012.4095
31. Ghaemi-Oskouie F, Shi Y. The role of uric acid as an endogenous danger signal in immunity and inflammation. Curr Rheumatol Rep. 2011;13(2):160–166. doi:10.1007/s11926-011-0162-1
32. Martinon F, Pétrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440(7081):237–241. doi:10.1038/nature04516
33. Meng ZH, Hudson AP, Hr S
34. Naff GB, Byers PH. Complement as a mediator of inflammation in acute gouty arthritis. I. Studies on the reaction between human serum complement and sodium urate crystals. J Lab Clin Med. 1973;81(5):747–760.
35. Fields TR, Abramson SB, Weissmann G, Kaplan AP, Ghebrehiwet B. Activation of the alternative pathway of complement by monosodium urate crystals. Clin Immunol Immunopathol. 1983;26(2):249–257. doi:10.1016/0090-1229(83)90143-5
36. Liu-Bryan R, Scott P, Sydlaske A, Rose DM, Terkeltaub R. Innate immunity conferred by Toll-like receptors 2 and 4 and myeloid differentiation factor 88 expression is pivotal to monosodium urate monohydrate crystal-induced inflammation. Arthritis Rheum. 2005;52(9):2936–2946. doi:10.1002/art.21238
37. Abdel KA, Kalluvya SE, Sadiq AM, Ashir A, Masikini PI. Prevalence of hyperuricemia and associated factors among patients with type 2 diabetes mellitus in Northwestern Tanzania: a cross-sectional study. Clin Med Insights Endocrinol Diabetes. 2024;17:11795514241274694. doi:10.1177/11795514241274694
38. Grayson PC, Kim SY, LaValley M, Choi HK. Hyperuricemia and incident hypertension: a systematic review and meta-analysis. Arthritis Care Res. 2011;63(1):102–110. doi:10.1002/acr.20344
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Prevalence of Hyperuricemia and Associated Factors Among Type 2 Diabetic Patients in Jordan
Abujbara M, Al Hourani HM, Al-Raoush RI, Khader YS, Ajlouni K
International Journal of General Medicine 2022, 15:6611-6619
Published Date: 16 August 2022
Association Between Triglyceride-Glucose Index and Serum Uric Acid Levels: A Biochemical Study on Anthropometry in Non-Obese Type 2 Diabetes Mellitus Patients
Luo Y, Hao J, He X, Wang C, Zhao H, Zhang Z, Yang L, Ren L
Diabetes, Metabolic Syndrome and Obesity 2022, 15:3447-3458
Published Date: 3 November 2022
The Mechanism of Sodium-Glucose Cotransporter-2 Inhibitors in Reducing Uric Acid in Type 2 Diabetes Mellitus
Dong M, Chen H, Wen S, Yuan Y, Yang L, Xu D, Zhou L
Diabetes, Metabolic Syndrome and Obesity 2023, 16:437-445
Published Date: 14 February 2023
The Association Between Sarcopenia and Diabetes: From Pathophysiology Mechanism to Therapeutic Strategy
Chen H, Huang X, Dong M, Wen S, Zhou L, Yuan X
Diabetes, Metabolic Syndrome and Obesity 2023, 16:1541-1554
Published Date: 30 May 2023
Uric Acid Metabolic Disorders in Pituitary-Target Gland Axis
Li R, Wu B, Han M, Li M, Yang X, Zhang J, Zhang Y, Liu Y
Diabetes, Metabolic Syndrome and Obesity 2024, 17:661-673
Published Date: 7 February 2024

