Back to Journals » Infection and Drug Resistance » Volume 18
β-Lactam/β-Lactamase Inhibitor Combinations Non-Susceptible ESBL-Producing Enterobacteriaceae Bloodstream Infections: An Underestimated Clinical Entity
Authors Zhang Y, Ni S, Hu H , Zhang S, Feng H, Ni L, Chen H, Yang Q , Yu M, Qu T
Received 8 January 2025
Accepted for publication 7 May 2025
Published 27 May 2025 Volume 2025:18 Pages 2687—2701
DOI https://doi.org/10.2147/IDR.S514373
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandip Patil
Yan Zhang,1,* Shuangling Ni,2,* Hangbin Hu,3,* Sheng Zhang,4 Haiting Feng,4 Lingmei Ni,4 Hongchao Chen,5 Qing Yang,5 Meihong Yu,1 Tingting Qu1,4
1State Key Laboratory for Diagnosis and Treatment of Infectious Disease, National Clinical Research Center for Infectious Diseases, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Department of Infectious Disease, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, 310003, People’s Republic of China; 2Infectious Disease Department, Lishui People’s Hospital, Lishui, 323000, People’s Republic of China; 3Department of Nutrition, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, 310003, People’s Republic of China; 4Infection Control Department, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, 310003, People’s Republic of China; 5Department of Laboratory Medicine, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, 310003, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tingting Qu, The First Affiliated Hospital, College of Medicine, Zhejiang University, 79# Qingchun East Road, Hangzhou, 310001, People’s Republic of China, Email [email protected] Meihong Yu, The First Affiliated Hospital, College of Medicine, Zhejiang University, 79# Qingchun East Road, Hangzhou, 310001, People’s Republic of China, Email [email protected]
Background: To describe the clinical and molecular characteristics of β-lactam/β-lactamase inhibitor combinations (BLBLIs) non-susceptible ESBL–producing Enterobacteriaceae (BnESBL-E) bloodstream infections (BSIs).
Methods: A cohort study was performed with ESBL-E-BSI cases from 2017 to 2019 in East China. Clinical characteristics, risk factors, and all-course mortality were evaluated. Whole-genome sequencing and antibiotic susceptibility testing were performed.
Results: Among the 187 patients with ESBL-E-BSI, 39.57% (74/187) had BnESBL-E-BSI. Nosocomial infections constituted 63.51% of BnESBL-E-BSIs, and 39.19% of cases originated from intra-abdominal sources. Risk factors for BnESBL-E-BSI included BLBLIs exposure within the preceding 3 months, ICU admission within the last 3 months, and the duration of hospital stay prior to BSI. Notably, a urinary source of bacteremia emerged as a protective factor against BnESBL-E-BSI(OR, 0.177; 95% CI, 0.049– 0.647; p=0.009). BnESBL-E-BSIs were associated with a higher 28-day mortality compared to BLBLIs-susceptible cases (31.08%vs.16.81%; p=0.031). Multivariate analysis identified the Pitt bacteremia score, CRP level, and hospitalization within the preceding 3 months as risk factors for BnESBL-E-BSI-related mortality, while receipt of carbapenems within 72 hours of symptom onset improved survival(OR, 0.128; 95% CI, 0.018– 0.912; p = 0.04). BnESBL-E isolates demonstrated no clonal transmission and remained highly susceptible to amikacin, carbapenems and tigecycline. Coexistence of multiple ESBL types was frequently observed, occurring in 40.6% of BnESBL-Ec and 72.7% of BnESBL-Kp isolates.
Conclusion: Given the high prevalence and mortality of BnESBL-E-BSI, carbapenems may be preferable treatment option for non-urinary ESBL-E-BSIs. BnESBL-E represents an underestimated clinical threat, warranting timely identification of risk factors and the consideration of appropriate empirical therapy.
Keywords: extended spectrum β-lactamase, β-lactam/β-lactamase inhibitors combinations, bloodstream infections, Enterobacteriaceae
Background
Extended-spectrum β-lactamase–producing Enterobacteriaceae (ESBL-E) have emerged as significant etiological agents of both community-acquired and nosocomial bloodstream infections (BSIs) worldwide.1,2 Among these, Escherichia coli (Ec) and Klebsiella pneumoniae (Kp) are the most prevalent pathogens. A study conducted in China in 2016 revealed that 16.5% of Kp and 55.5% of Ec isolates from community-onset BSIs were ESBL producers, with even higher proportions observed in nosocomial-onset BSIs.3,4 BSIs caused by ESBL-E (ESBL-E-BSIs) are associated with high morbidity and mortality, with rates reaching up to 20% and even 43.9% within 30 days in patients with sepsis.5,6 ESBLs are enzymes that confer resistance to a wide spectrum of β-lactam antibiotics and are frequently co-expressed with additional resistance mechanisms, thereby contributing to multidrug resistance.7 The majority of ESBLs belong to Ambler class A, with TEM (temoniera β-lactamase), SHV (sulfhydryl reagent variable β-lactamase), and CTX-M (cefotaxime-M β-lactamase) being the predominant types.1,7
β-lactam/β-lactamase inhibitor combinations (BLBLIs) and carbapenems are the most commonly used agents for managing infections caused by ESBL producers.8,9 In the last decades, BLBLIs have emerged as an alternative to carbapenems used in ESBL-E infections.10 BLBLIs, such as piperacillin/tazobactam (TZP) and cefoperazone/sulbactam (CSL) are often employed as empirical therapy in hospitalized patients. However, the increased clinical application of BLBLIs has driven bacterial evolution, leading to the emergence and proliferation of ESBL-E strains that exhibit resistance to these combinations. A decline in TZP susceptibility among Ec and Kp has been observed over time.11 Although numerous clinical studies have focused on ESBL-E-BSIs,6,12,13 there is a paucity of systematic clinical research specifically addressing BLBLIs non-susceptible ESBL-E (BnESBL-E) BSIs. Infections caused by BnESBL-E pose a significant clinical challenge, as empirical treatment with BLBLIs may prove ineffective, resulting in therapeutic delays and increased mortality rates.14 Thus, the early identification of patients at risk for BnESBL-E infections is crucial to enable prompt initiation of appropriate antimicrobial therapy.
This study aims to investigate the clinical characteristics, risk factors, and outcomes associated with BnESBL-E-BSIs in a tertiary hospital in East China from 2017 to 2019. Additionally, we seek to characterize the genomic alterations within the BnESBL-E population and their corresponding phenotypic and pathogenic traits. Our findings aim to enhance the understanding of BnESBL-E-BSIs and provide guidance for clinical management.
Method
Study Population
A retrospective cohort study was conducted on cases of ESBL-E-BSIs at a 5000-bed tertiary teaching hospital in East China from January 2017 to December 2019. Cases of ESBL-E-BSIs were retrieved from the conventional microbiology laboratory database. Patients with a blood culture positive for ESBL-Ec or ESBL-Kp, clinical manifestations of infection, and a complete clinical data set were included. Initially, 192 patients were identified; however, 5 cases of polymicrobial BSI were excluded, resulting in a final cohort of 187 patients. For patients with two or more positive blood cultures, only the first episode was selected. The study flowchart is shown in Figure 1. Epidemiological and clinical data were collected using a standardized case record form. The study was conducted in accordance with the Declaration of Helsinki. This retrospective study received approval from the Institutional Review Board of the First Affiliated Hospital of Zhejiang University in China, under the research ethics approval code IIT20231028A. The requirement for informed consent was waived due to the retrospective nature of the study, and it did not include any protected patient information.
Bacterial Identification, Antimicrobial Susceptibility Testing and ESBL Production Detection
The automated VITEK 2 COMPACT system was used for bacterial identification. Antimicrobial susceptibility testing was performed by broth dilution method and Kirby-Bauer method according to Clinical and Laboratory Standards Institute (CLSI) guidelines. The minimum inhibitory concentrations (MICs) of TZP and CSL were determined according to CLSI guidelines. And ESBL production was determined by double-disk potentiation assay using amoxicillin-clavulanic acid, cefotaxime, ceftazidime, or cefepime, according to CLSI guidelines. Ec ATCC 25922 and Kp ATCC 700603 were employed as quality-control strains.
CLSI 2023 criteria were used to interpret the results according to the interpretation standards for TZP (≤8/4 mg/L=sensitive, ≥32/4 mg/L=resistant). The FDA criteria for cefoperazone were used to interpret the results for CSL (≤16/8 mg/L=sensitive, ≥64/32 mg/L=resistant).
Whole Genome Sequencing and Bioinformatics Analysis
The genomic DNA extraction kit (Qiagen, USA) was used to extract genomic DNA. The genome library was sequenced on the Illumina Hi Seq™ 2000 sequencing platform. In silico analyses were performed on the CLC Genomic Workbench (version 8.0). Genome annotation was performed via the RAST server (http://rast.nmpdr.org/). Sequence type (ST) and resistance genes were detected using MLST 2.0 and ResFinder 4.1 on the CGE server with default settings (https://cge.cbs.dtu.dk/services/). Virulence genes were determined online in the Institute Pasteur database (https://bigsdb.pasteur.fr/).
Variables and Definitions
The duration of stay before BSI was defined as the time from hospital admission to the collection of the first positive blood culture. Nosocomial bacteremia was identified by the isolation of ESBL-E from blood samples collected more than 48 hours after admission. Co-infection in other parts was defined as the simultaneous presence of infectious lesions in areas other than the primary lesion. The source of bacteremia was determined according to the Centers for Disease Control’s definitions of nosocomial infections (1988). The Pitt Bacteremia Score (PBS) was utilized, incorporating variables such as temperature, hypotension, mechanical ventilation, cardiac arrest, and mental status, as outlined in reference.15 The PBS is widely acknowledged as an objective indicator of acute illness severity in patients with severe infections, including BSI.15 Our research employed the PBS to evaluate infection severity. At BSI diagnosis, laboratory examinations and PBS were taken. The clinical outcome was 28-day all-cause mortality. Appropriate therapy was defined as the administration of effective drugs, as determined by the in vitro susceptibility testing, during the infection episode.16
Patients infected with ESBL-E sensitive to TZP and CSL were classified as having BLBLIs sensitive ESBL-E (BsESBL-E) infections. Patients infected with ESBL-E intermediate or resistant to TZP or CSL were classified as having BnESBL-E infections.
Statistical Analysis
Continuous variables were expressed as medians (interquartile ranges) or means ± standard deviations and assessed using Student’s t-test (for normally distributed variables) or Mann–Whitney-U test (for non-normally distributed variables). Categorical variables were expressed as percentages of the group and analyzed by the χ2 test or the two-tailed Fisher exact test appropriately. Two-tailed tests were used to determine statistical significance. Multivariate analysis was performed by logistic regression, and incorporating variables with a p-value≤0.1 from the univariate analysis through a stepwise approach. Kaplan–Meier analysis was utilized to estimate the survival distribution function, and Kaplan–Meier survival curves were generated for patients with BsnESBL-E and BsESBL-E infections. In all analyses, a p-value<0.05 was considered significant. All statistical analyses were performed using SPSS version 23.0 (IBM Corporation, Armonk, NY, USA).
Results
Clinical Characteristics of 187 Patients Infected with ESBL-E-BSI
A total of 187 cases of ESBL-E-BSI were included in the study, consisting of 74 cases (39.57%) from the BnESBL-E group and 113 cases (60.43%) from the BsESBL-E group. The proportion of BnESBL-E-BSI within the ESBL-BSI cohort ranged from 35.23% to 47.29% between 2017 and 2019, demonstrating an increasing trend over the years (Appendix 1). Among the 187 patients, 140 (74.87%) were infected with ESBL-Ec, while 47 (25.13%) were infected with ESBL-Kp. Notably, BnESBL-Kp accounted for 70.21% (33/47) of the ESBL-Kp cases, whereas BnESBL-Ec constituted 29.28% (41/140) of the ESBL-Ec cases.
The epidemiological and clinical characteristics of these 187 patients are detailed in Table 1. The median age was 60.83 years, with 44.39% of the patients aged over 65. Males comprised 64.71% of the cohort. The most prevalent underlying comorbidities were cardiovascular disease (86%), solid malignancies (80%), and pancreaticobiliary disease (58%). Additionally, 107 patients (57.22%) had been hospitalized within the preceding 3 months, and 18 (9.63%) had been admitted to the intensive care unit (ICU) during the same timeframe. Notably, 101 patients (54.01%) had prior antibiotic/antimicrobial exposure within the last 3 months. In 39.04% of cases, the infections were nosocomial. The primary source of bacteremia was intra-abdominal infection (29.41%), followed by urinary tract infection (13.90%) and respiratory tract infection (7.49%). The overall 28-day mortality rate was 22.46%.
 |
Table 1 Clinical Characteristics of 187 ESBL-E BSI Patients in This Study |
Risk Factors for Development of BnESBL-E-BSI
Table 1 compared the epidemiological and clinical characteristics between the BnESBL-E group and the BsESBL-E group. Both groups had similar distributions in terms of age, gender, history of abdominal surgery, and prior invasive procedures or device use. However, cardiovascular and urinary system diseases were significantly more prevalent in the BsESBL-E group (p=0.037 and p=0.019, respectively). In contrast, the BnESBL-E group was more likely to have prior BLBLIs exposure within the last 3 months (p=0.002) and prior ICU admission within the last 3 months (p=0.004). In the BnESBL-E group, more patients were nosocomial (p<0.001), with longer duration of stay before the onset of BSI (p<0.001). Within the BnESBL-E group, 55.41% (41/74) of cases were caused by ESBL-Ec, while 44.59% (33/74) were caused by ESBL-Kp, In contrast, the BsESBL-E group had proportions of 87.61% (99/113) for ESBL-Ec and 12.39% (14/113) for ESBL-Kp, respectively.(p<0.01) Furthermore, intra-abdominal infection (39.19%) was the most common source of bacteremia in the BnESBL-E group, followed by pulmonary (9.46%) and urinary tract infections (4.05%), while in the BsESBL-E group, intra-abdominal and urinary tract infections were equally prevalent as the primary sources of bacteremia (23.89% each), with pulmonary infection accounting for 7.96%. In addition, the BnESBL-E group exhibited higher PBS and elevated white blood cell (WBC) levels (p = 0.026 and p = 0.006, respectively). Notably, the 28-days all-cause mortality was significantly higher in the BnESBL-E group compared to the BsESBL-E group (p =0.031). The 28-day survival curves, stratified by the susceptibility of ESBL-E to BLBLIs, demonstrated a significant difference, as detailed in Appendix 2.
Multivariate analysis identified prior BLBLIs exposure within the last 3 months (OR, 2.340; 95% CI, 1.117–4.904; p = 0.024), ICU admission within the last 3 months (OR, 3.167; 95% CI, 1.009–9.937; p = 0.048), and prolonged duration of stay before BSI (OR, 1.035; 95% CI, 1.008–1.062; p = 0.01) as independent risk factors for BnESBL-E-BSI (Table 1). According to the ROC curve analysis, a duration of stay before BSI of ≥3 days predicted BnESBL-E-BSI with a sensitivity of 71.62% and a specificity of 54.87%. In contrast, a urinary source of bacteremia emerged as a protective factor against BnESBL-E-BSI(OR, 0.177; 95% CI, 0.049–0.647; p=0.009). (Table 1)
Among the 74 patients with BnESBL-E-BSI, 47 individuals (63.51%) had infections caused by ESBL-E non-susceptible to either TZP or CSL, classified as BnESBL-E group 1, while 27 individuals (36.49%) were infected with ESBL-E non-susceptible to both agents, categorized as BnESBL-E group 2. Multivariate analysis revealed that age was the only risk factor for infections with ESBL-E non-susceptible to both TZP and CSL. In comparison, community-acquired infections were more likely to involve ESBL-E non-susceptible to either TZP or CSL. (Appendix 3)
Mortality Predictor Analysis for 28-Day Mortality in ESBL-E-BSI Patients
Among the 187 patients with ESBL-E-BSI, 145 (77.54%) survived, while 42 (22.46%) succumbed to the infection. Mortality rates were comparable between patients infected with ESBL-Kp and those with ESBL-Ec (23.40% vs 22.14%, p=0.84). Detailed factors potentially influencing 28-day mortality are provided in Appendix 4.
Multivariate analysis revealed the PBS (OR, 1.297; 95% CI, 1.091–1.543; p=0.003) as the only risk factor for ESBL-E-BSI related mortality, while the administration of appropriate therapy within 72 hours after symptom onset was identified as a significant protective factor(OR, 0.317; 95% CI, 0.107–0.940; p=0.038).
Mortality Predictor Analysis for 28-Day Mortality in BnESBL-E-BSI Patients
Among the 74 patients with BnESBL-E-BSI, the 28-day mortality rate was found to be 31.08% (23/74). Notably, there was no significant difference in mortality between patients infected with BnESBL-Kp and those with BnESBL-Ec (30.30% vs 31.71%, p=1.00). Univariate analysis indicated that non-survivors exhibited distinct characteristics compared to survivors, including hospitalization within the preceding 3 months, higher PBS, elevated WBC counts, increased CRP levels, and reduced serum albumin levels. (p<0.05)
In terms of treatment, carbapenems and BLBLIs were the most commonly used drugs, with 63.51% (47/74) of patients receiving carbapenem monotherapy, and 21.62% (16/74) receiving BLBLIs monotherapy within 72 hours of symptom onset. Univariate analysis revealed that initiating carbapenem treatment within 72 hours of symptom onset was significantly associated with reduced mortality. However, the administration of BLBLIs within 72 hours of symptom onset did not improve outcomes (Table 2).
 |
Table 2 Mortality Predictor Analysis for 30-Day Mortality in BnESBL-E BSI Patients |
Multivariate analysis identified several independent predictors of BnESBL-E-BSI-related mortality: a higher PBS (OR, 1.605; 95% CI, 1.149–2.240; p=0.005), elevated CRP levels (OR, 1.025; 95% CI, 1.007–1.044; p=0.007), and hospitalization within the last 3 months (OR, 136.765; 95% CI, 4.533–4126.777; p=0.005). Conversely, receipt of carbapenems within 72 hours of symptom onset was significantly associated with improved survival (OR, 0.·128; 95% CI, 0.018–0.912; p=0.04). (Table 2)
Antimicrobial Susceptibility Testing of Isolates
The results of antimicrobial susceptibility testing on 187 ESBL-producing isolates are summarized in Table 3. Among these, 113 isolates were categorized as BsESBL-E, consisting of 14 BsESBL-Kp and 99 BsESBL-Ec. The remaining 74 isolates were classified as BnESBL-E, which included 30 isolates non-susceptible to CSL (6 ESBL-Kp, 24 ESBL-Ec), 17 isolates non-susceptible to TZP (14 ESBL-Kp, 3 ESBL-Ec), and 27 isolates non-susceptible to both TZP and CSL (13 ESBL-Kp, 14 ESBL-Ec). The MICs for TZP and CSL of all 187 ESBL-E isolates are presented in Appendix 5. Overall, BnESBL-E isolates demonstrated a nonsusceptibility rate of 59.46% to TZP and 77.03% to CSL.
 |
Table 3 Antimicrobial Susceptibilities of 187 ESBL-E Isolates |
Comparative analysis showed that BnESBL-E isolates had higher nonsusceptibility rates than BsESBL-E isolates. Both BnESBL-Ec and BnESBL-Kp displayed high level of nonsusceptibility to gentamicin, ciprofloxacin, levofloxacin, cefuroxime, ceftazidime, cefepime and aztreonam. BnESBL-Ec isolates exhibited significantly higher nonsusceptibility to gentamicin, cefoxitin and cefepime compared to BsESBL-Ec (56.67% vs 27.89%, p=0.001; 48.78% vs 22.45%, p=0.004; 80.95% vs 51.04%, p=0.001). Similarly, BnESBL-Kp isolates showed higher nonsusceptibility to ceftazidime and cefepime than BsESBL-Kp isolates (87.10% vs 62.5%, p=0.002; 87.10% vs 42.86%, p=0.004; 100.00% vs 57.14%, p=0.012, respectively). It is worth noting that both BnESBL-E and BsESBL-E showed high susceptibility to amikacin (90.54% vs 97.35%), ertapenem (100% vs 100%), imipenem (100% vs 100%), meropenem (MEM, 100% vs 100%) and tigecycline (97.1% vs 100%). (Table 3)
Genetic Relatedness, Antibiotic Resistance Genes, and Virulence Genes of Isolates
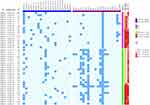
Among the 74 BnESBL-E isolates, 43 has been conserved previously, with their genomic characteristics illustrated in Figure 2. In this study, the 17 Kp strains and 26 Ec strains exhibited diverse ST types.
Of the 17 BnESBL-Kp strains, the blaCTX-M gene was the most prevalent ESBL gene (14 strains, 82.35%), followed by blaTEM (13 strains, 76.47%) and blaSHV (10 strains, 58.82%). Of the 13 strains harboring blaTEM, 12 (92.31%) contained the blaTEM-1 variant. A significant proportion (82.35%) of these BnESBL-Kp strains (14/17) harbored multiple ESBL genes. Specifically, 35.29% (6/17) possessed blaCTX-M+blaTEM+blaSHV, 29.41% (5/17) possessed blaCTX-M+blaTEM, 11.76% (2/17) possessed blaSHV+blaCTX-M and 5.88% (1/17) possessed blaSHV+blaTEM. Only 17.65% (3/17) carried a single ESBL gene. Additionally, co-existence of ESBLs with other beta-lactamases was observed within the same isolate. (Figure 3)
Among the 26 BnESBL-Ec strains, blaCTX-M was the predominant ESBL genotype (24, 92.31%), followed by blaTEM (16, 61.54%). The blaSHV gene was absent in all BnESBL-Ec strains. The blaCTX-M-14 variant emerged as the most common type, found in 14 isolates (53.85%). Of the 16 strains harboring blaTEM, 12 (75%) contained the blaTEM-1 variant. Half of the BnESBL-Ec strains (13/26) carried multiple ESBL genes, including 18.75% (3/16) possessed a combination of two blaCTX-M genes and blaTEM, while 62.5% (10/16) carried blaCTX-M+blaTEM. The remaining 50% of BnESBL-Ec strains (13/26) carried a single ESBL gene, with 10 strains containing blaCTX-M and 3 strains harboring blaTEM. Additionally, two BnESBL-Ec strains harbored AmpC in addition to ESBL genes. (Figure 3)
The analysis of virulence genes revealed that the 17 BnESBL-Kp strains exhibited a low carriage rate of such genes. Notably, no hypervirulence-associated genes, such as rmpA/rmpA2, iucA, iroB and peg-344, were detected. In contrast, a significant proportion of the 26 BnESBL-Ec strains carried virulence factors, including the adhesin-related virulence gene fimH (23/26, 88.5%), the effective iron uptake gene fyuA (16/26, 61.5%), kpsM (15/26, 57.7%), iutA (14/26, 53.8%), and iroD (5/26, 19.2%). (Figure 3)
Discussion
BLBLIs have been widely used to treat ESBL-producing bacterial infections. However, the prevalence and clinical prognosis of infections caused by ESBL-producing bacteria that are non-susceptible to BLBLIs remain insufficiently explored. Our study provides a comprehensive clinical and microbiological characterization of a cohort with BnESBL-E-BSIs. This detailed analysis enhances the current understanding of the clinical diagnosis and empirical antibiotic treatment of these challenging infections.
We report a striking prevalence of BnESBL-E-BSI, constituting 39.57% of ESBL-E-BSIs in a tertiary care center in China, highlighting an urgent need for improved surveillance and early detection strategies. The 28-day mortality rate associated with BnESBL-E-BSI was significantly higher than that of BsESBL-E-BSI, at 31.08% versus 16.81%, respectively. Moreover, the highest mortality rate was observed in cases that were non-susceptible to both TZP and CSL (33.33%). These findings underscore the adverse impact of BnESBL-E bacteremia on patient outcomes, including severe clinical presentations, extended hospitalization, and increased mortality, thereby emphasizing its underestimated clinical significance.
Given the high prevalence and elevated mortality rate associated with BnESBL-E-BSI, it is crucial to identify risk factors that can guide appropriate empirical therapies. Our analysis identified prior BLBLIs exposure within three months as a significant risk factor for developing BnESBL-E-BSI. Antibiotic exposure, can foster the development of drug resistance. Previous studies have similarly underscored the role of oxyimino-beta-lactams in increasing the risk of ESBL-E-related BSIs.14,17 Specifically, prior exposure to BLBLIs has been linked to an increased risk of BSI caused by TZP non-susceptible but ceftriaxone-susceptible isolates.18 The association between BLBLIs exposure and the risk of BnESBL-E-BSI may be attributed to the selection of BnESBL-Ec and Kp as dominant isolates, promoting the emergence of endogenous infections, and triggering the generation of these pathogens in clinical settings.18,19 For instance, BLBLIs exposure in vivo could induce IS26-mediated duplication of blaCTX-M-65, leading to higher cephalosporin resistance in Ec.19 Additionally, ICU admission within the last three months and prolonged hospital stays prior to BSI were also identified as risk factors, which are consistent with established risk factors for multidrug-resistant infections.20–23
Our analysis also underscores the differential sources of BnESBL-E-BSI compared to BsESBL-E-BSI. In our study, intra-abdominal infections emerged as the primary source of BnESBL-E-BSI, whereas BsESBL-E cases exhibited comparable frequencies of intra-abdominal and urinary tract sources. Interestingly, a urinary source of bacteremia was identified as a protective factor against BnESBL-E-BSI. This observation may be due to the lower likelihood of BLBLIs exposure in community-acquired urogenital bacteremia, where BsESBL-E isolates accounted for up to 90% of cases, compared to only 10% for BnESBL-E. This finding aligns with the Infectious Diseases Society of America’s (IDSA) recommendation for carbapenem therapy in ESBL-E infections originating outside the urinary tract.24 Furthermore, the rapid and accurate identification of the infection source (eg, urinary source) can facilitate the timely initiation of appropriate antibiotic therapy and improve clinical outcomes.
In our study, the ST types of the 17 BnESBL-Kp strains and 26 BnESBL-Ec were widely distributed, indicating a highly diverse genotype distribution among these strains, and ruling out clonal epidemic transmission. Moreover, our study did not detect hypervirulent clones of Ec and Kp commonly associated with bloodstream infections, such as serotypes K1 and K2 of Kp and ST131 of Ec. Given the low prevalence of virulence genes in BnESBL-E isolates, we speculate that the acquisition of drug resistance may impose an adaptive cost on these bacteria.
Nowadays, CTX-M-type enzymes are the most common ESBL type.25 In our study, blaCTX-M was predominant in BnESBL-Kp (82.35%) and BnESBL-Ec (92.31%), with blaCTX-M-14 being predominant in BnESBL-Ec, consistent with other reports.26 Following this, blaTEM was present in 76.47% of BnESBL-Kp and 61.54% of BnESBL-Ec, with blaTEM-1 being the most prevalent variant. A prior study has shown that blaTEM is the most frequently identified β-lactamase gene detected in TZP-intermediate or resistant Ec isolates, with the majority producing TEM-1, which aligns with our findings.27 The hyperproduction of TEM-1 is a well-documented mechanism contributing to resistance against BLBLIs.28,29 Furthermore, TEM enzymes are involved in the acquired resistance to TZP, potentially facilitating the progression from low-level to high-level resistance to BLBLIs.30 The high proportion of blaTEM observed in our study could potentially contribute to resistance against BLBLIs. However, this study did not evaluate the expression levels of blaTEM genes.
An important finding of the study was the coexistence of different ESBLs and other beta-lactamase genes within the same isolate. Specifically, 82.35% of BnESBL-Kp and 50% of BnESBL-Ec harbored at least 2 ESBL genes. Previous studies have documented the coexistence of different ESBLs in ESBL-Kp and ESBL-Ec, which correlates with higher antibiotic resistance.26,31,32 For example, ESBL-Kp and ESBL-Ec harboring blaCTX-M, blaTEM, and blaSHV have been reported to exhibit increased resistance to trimethoprim-sulfamethoxazole, gentamicin, ciprofloxacin, and meropenem.32 This may be due to the frequent co-harboring of other antimicrobial resistance genes on the same conjugative plasmids carrying ESBL genes.32–34 In addition, the presence of additional ESBLs or AmpC may create a “complex background” that renders BLBLIs ineffective.35 Thus, the co-expression of different β-lactamases within a single BnESBL-E is prevalent and may represent one of the mechanisms underlying BLBLIs resistance, warranting further investigation.
Currently, carbapenems are the preferred treatment for BSI caused by ESBL-E. In our study, carbapenems and BLBLIs were the most frequently utilized antimicrobial agents for treating BnESBL-E-BSI. Our findings indicated that patients receiving carbapenem monotherapy exhibited a reduced 28-day mortality rate compared to those receiving BLBLIs monotherapy. Additionally, multivariate analysis demonstrated that the early administration of carbapenems within 72 hours of symptom onset was associated with an improved prognosis in BnESBL-E-BSI, whereas BLBLIs were not. Therefore, carbapenems represent a more suitable therapeutic option than BLILIs for the management of BnESBL-E-BSI. A pivotal randomized clinical trial has demonstrated that TZP treatment is associated with higher mortality rates in ESBL-E-BSI cases compared to treatment with meropenem, thereby not supporting the use of TZP in this context.36 Nevertheless, this study did not include data from China, and available data from this region were limited. Our research contributes data from the Chinese population, and the results are consistent with those of the aforementioned large-scale international clinical study.36 Moreover, there are instances in clinical practice where non-standard use occurs, with physicians choosing BLBLIs to treat patients with ESBL-E infections originating outside the urinary tract when drug susceptibility tests indicate sensitivity to BLBLIs. Our research advocates for the use of carbapenems in cases of ESBL-E-BSI, irrespective of the pathogen’s susceptibility to BLBLIs. This study provides recommendations for the clinical management of ESBL bacterial infections within the Chinese population and holds clinical significance. This research reinforces the recommendation of carbapenems as the first-line therapy for ESBL-E-BSI. Furthermore, the BnESBL-E isolates demonstrated susceptibility to amikacin and tigecycline, in addition to carbapenems, which may be considered alternatives for the treatment of BnESBL-E-BSIs. The administration of timely and appropriate antibiotic therapy has been consistently associated with improved outcomes. Therefore, prompt treatment with carbapenems is recommended for managing BnESBL-E-BSIs.
Our study has certain limitations. Firstly, the sample size was relatively small, and serial imaging to monitor disease progression was not feasible. Secondly, the mechanisms underlying BLBLIs resistance in ESBL-E, including beta-lactamase expression and porin efflux pump activity, were not evaluated in this study and warrant further investigation. Consequently, future research is necessary to enhance our understanding of this subset of patients and the resistance mechanisms associated with this unique phenotype.
Conclusion
In conclusion, BnESBL-E-BSI are associated with considerable mortality rates and are becoming increasingly prevalent. Independent risk factors for the development of BnESBL-E-BSI include exposure to BLBLIs within the preceding 3 months, recent ICU admission, and prolonged hospital stay prior to the onset of BSI. Additionally, a higher PBS, elevated CRP levels, and hospitalization within the last 3 months were identified as predictors of BnESBL-E-BSI-related mortality. Importantly, administration of carbapenems within the first 72 hours significantly improved patient survival outcomes. BnESBL-E isolates demonstrated high levels of antibiotic resistance, with frequent co-occurrence of multiple ESBL enzymes within a single strain. These findings underscore the critical need for early detection of BnESBL-E infections and emphasize the importance of continuous surveillance of antibiotic resistance patterns and the molecular characteristics of ESBL-producing Enterobacteriaceae.
Abbreviations
ESBL, Extended-spectrum β-lactamase; ESBL-E, Extended-spectrum β-lactamase–producing Enterobacteriaceae; BSIs, bloodstream infections; Ec, Escherichia; Kp, Klebsiella pneumoniae; ESBL-E-BSIs, BSIs caused by ESBL-E; TEM, temoniera β-lactamase; SHV, sulfhydryl reagent variable β-lactamase; CTX-M, cefotaxime-M β-lactamase; BLBLIs, β-lactam/β-lactamase inhibitor combinations; TZP, piperacillin/tazobactam; CSL, cefoperazone/sulbactam; BnESBL-E, BLBLIs non-susceptible ESBL-E; CLSI, Clinical and Laboratory Standards Institute; MICs, minimum inhibitory concentrations; PBS, Pitt Bacteremia Score; BsESBL-E, BLBLIs sensitive ESBL-E; ICU, intensive care unit; WBC, white blood cell.
Data Sharing Statement
The data in this study can be accessed by sending a request to the corresponding author.
Ethical Approval
This study received approval from the Institutional Review Board of the First Affiliated Hospital of Zhejiang University in China, under the research ethics approval code IIT20231028A.
Acknowledgment
Yan Zhang, Shuangling Ni and Hangbin Hu should be considered co-first authors.
Funding
This work was funded by the National Key Research and Development Program of China (2021YFC2301800), and Zhejiang Provincial Medical and Health Technology Plan Project (2023KY103).
Disclosure
The authors declare no conflict of interest.
References
1. Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005;18(4):657–686. doi:10.1128/CMR.18.4.657-686.2005
2. Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8(3):159–166. doi:10.1016/S1473-3099(08)70041-0
3. Quan J, Zhao D, Liu L, et al. High prevalence of ESBL-producing Escherichia coli and Klebsiella pneumoniae in community-onset bloodstream infections in China. J Antimicrob Chemother. 2017;72(1):273–280. doi:10.1093/jac/dkw372
4. Timsit JF, Ruppé E, Barbier F, Tabah A, Bassetti M. Bloodstream infections in critically ill patients: an expert statement. Intensive Care Med. 2020;46(2):266–284. doi:10.1007/s00134-020-05950-6
5. Palacios-Baena ZR, Gutiérrez-Gutiérrez B, Calbo E, et al. Empiric therapy with carbapenem-sparing regimens for bloodstream infections due to extended-spectrum β-lactamase-producing Enterobacteriaceae: results from the INCREMENT cohort. Clin Infect Dis. 2017;65(10):1615–1623. doi:10.1093/cid/cix606
6. Russo A, Falcone M, Gutiérrez-Gutiérrez B, et al. Predictors of outcome in patients with severe sepsis or septic shock due to extended-spectrum β-lactamase-producing Enterobacteriaceae. Int J Antimicrob Agents. 2018;52(5):577–585. doi:10.1016/j.ijantimicag.2018.06.018
7. Peirano G, Pitout JDD. Extended-spectrum β-lactamase-producing Enterobacteriaceae: update on molecular epidemiology and treatment options. Drugs. 2019;79(14):1529–1541. doi:10.1007/s40265-019-01180-3
8. Giannella M, Pascale R, Ferraro G, et al. Risk factors for treatment failure in patients receiving β-lactam/β-lactamase inhibitor combinations for Enterobacteriaceae bloodstream infection: a retrospective, single-centre, cohort study. Int J Antimicrob Agents. 2019;53(5):574–581. doi:10.1016/j.ijantimicag.2019.01.005
9. Tamma PD, Han JH, Rock C, et al. Carbapenem therapy is associated with improved survival compared with piperacillin-tazobactam for patients with extended-spectrum β-lactamase bacteremia. Clin Infect Dis. 2015;60(9):1319–1325. doi:10.1093/cid/civ003
10. Tamma PD, Rodriguez-Bano J. The use of noncarbapenem β-lactams for the treatment of extended-spectrum β-lactamase infections. Clin Infect Dis. 2017;64(7):972–980. doi:10.1093/cid/cix034
11. Lowe CF, McGeer A, Muller MP, Katz K. Decreased susceptibility to noncarbapenem antimicrobials in extended-spectrum-β-lactamase-producing Escherichia coli and Klebsiella pneumoniae isolates in Toronto, Canada. Antimicrob Agents Chemother. 2012;56(7):3977–3980. doi:10.1128/AAC.00260-12
12. Qureshi ZA, Paterson DL, Pakstis DL, et al. Risk factors and outcome of extended-spectrum β-lactamase-producing Enterobacter cloacae bloodstream infections. Int J Antimicrob Agents. 2011;37(1):26–32. doi:10.1016/j.ijantimicag.2010.09.009
13. Xiao T, Yang K, Zhou Y, et al. Risk factors and outcomes in non-transplant patients with extended-spectrum beta-lactamase-producing Escherichia coli bacteremia: a retrospective study from 2013 to 2016. Antimicrob Resist Infect Control. 2019;8(1):144. doi:10.1186/s13756-019-0599-y
14. Pilmis B, Zahar JR. Ventilator-associated pneumonia related to ESBL-producing gram negative bacilli. Ann Transl Med. 2018;6(21):424. doi:10.21037/atm.2018.09.34
15. Paterson DL, Ko WC, Von Gottberg A, et al. International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum beta-lactamase production in nosocomial infections. Ann Intern Med. 2004;140(1):26–32. doi:10.7326/0003-4819-140-1-200401060-00008
16. Shi Q, Huang C, Xiao T, Wu Z, Xiao Y. A retrospective analysis of Pseudomonas aeruginosa bloodstream infections: prevalence, risk factors, and outcome in carbapenem-susceptible and -non-susceptible infections. Antimicrob Resist Infect Control. 2019;8(1):68. doi:10.1186/s13756-019-0520-8
17. Rodríguez-Baño J, Navarro MD, Retamar P, Picón E, Pascual Á. β-Lactam/β-lactam inhibitor combinations for the treatment of bacteremia due to extended-spectrum β-lactamase-producing Escherichia coli: a post hoc analysis of prospective cohorts. Clin Infect Dis. 2012;54(2):167–174. doi:10.1093/cid/cir790
18. Baker TM, Rogers W, Chavda KD, et al. Epidemiology of bloodstream infections caused by Escherichia coli and Klebsiella pneumoniae that are piperacillin-tazobactam-non-susceptible but ceftriaxone-susceptible. Open Forum Infect Dis. 2018;5(12):ofy300. doi:10.1093/ofid/ofy300
19. Wang Y, He J, Sun L, et al. IS26 mediated bla(CTX-M-65) amplification in Escherichia coli increase the antibiotic resistance to cephalosporin in vivo. J Glob Antimicrob Resist. 2023;35:202–209. doi:10.1016/j.jgar.2023.09.018
20. Mosqueda-Gómez JL, Montaño-Loza A, Rolón AL, et al. Molecular epidemiology and risk factors of bloodstream infections caused by extended-spectrum beta-lactamase-producing Klebsiella pneumoniae A case-control study. Int J Infect Dis. 2008;12(6):653–659. doi:10.1016/j.ijid.2008.03.008
21. Fernández J, Prado V, Trebicka J, et al. Multidrug-resistant bacterial infections in patients with decompensated cirrhosis and with acute-on-chronic liver failure in Europe. J Hepatol. 2019;70(3):398–411. doi:10.1016/j.jhep.2018.10.027
22. Boscolo A, Sella N, Pettenuzzo T, et al. Multidrug-resistant and extended-spectrum β-lactamase gram-negative bacteria in bilateral lung transplant recipients: incidence, risk factors, and in-hospital mortality. Chest. 2022;162(6):1255–1264. doi:10.1016/j.chest.2022.06.046
23. Kandemir O, Akbay E, Sahin E, Milcan A, Gen R. Risk factors for infection of the diabetic foot with multi-antibiotic resistant microorganisms. J Infect. 2007;54(5):439–445. doi:10.1016/j.jinf.2006.08.013
24. Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious diseases society of America 2023 guidance on the treatment of antimicrobial resistant gram-negative infections. Clin Infect Dis. 2023:ciae403.
25. Castanheira M, Simner PJ, Bradford PA. Extended-spectrum β-lactamases: an update on their characteristics, epidemiology and detection. JAC Antimicrob Resist. 2021;3(3):dlab092. doi:10.1093/jacamr/dlab092
26. Lin CF, Hsu SK, Chen CH, Huang JR, Lo HH. Genotypic detection and molecular epidemiology of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a regional hospital in central Taiwan. J Med Microbiol. 2010;59(Pt 6):665–671. doi:10.1099/jmm.0.015818-0
27. Rodríguez-Villodres Á, Gutiérrez Linares A, Gálvez-Benitez L, Pachón J, Lepe JA, Smani Y. Semirapid detection of piperacillin/tazobactam resistance and extended-spectrum resistance to β-lactams/β-lactamase inhibitors in clinical isolates of Escherichia coli. Microbiol Spectr. 2021;9(2):e0080121. doi:10.1128/Spectrum.00801-21
28. Babic M, Hujer AM, Bonomo RA. What’s new in antibiotic resistance? Focus on beta-lactamases. Drug Resist Updat. 2006;9(3):142–156. doi:10.1016/j.drup.2006.05.005
29. Chaïbi EB, Sirot D, Paul G, Labia R. Inhibitor-resistant TEM beta-lactamases: phenotypic, genetic and biochemical characteristics. J Antimicrob Chemother. 1999;43(4):447–458. doi:10.1093/jac/43.4.447
30. Rodríguez-Villodres Á, Gil-Marqués ML, Álvarez-Marín R, et al. Extended-spectrum resistance to β-lactams/β-lactamase inhibitors (ESRI) evolved from low-level resistant Escherichia coli. J Antimicrob Chemother. 2020;75(1):77–85. doi:10.1093/jac/dkz393
31. Pokhrel RH, Thapa B, Kafle R, Shah PK, Tribuddharat C. Co-existence of beta-lactamases in clinical isolates of Escherichia coli from Kathmandu, Nepal. BMC Res Notes. 2014;7(1):694. doi:10.1186/1756-0500-7-694
32. Silago V, Kovacs D, Samson H, et al. Existence of multiple ESBL genes among phenotypically confirmed ESBL producing Klebsiella pneumoniae and Escherichia coli concurrently isolated from clinical, colonization and contamination samples from neonatal units at Bugando medical center, Mwanza, Tanzania. Antibiotics. 2021;10(5). doi:10.3390/antibiotics10050476
33. Paterson DL. Recommendation for treatment of severe infections caused by Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs). Clin Microbiol Infect. 2000;6(9):460–463. doi:10.1046/j.1469-0691.2000.00107.x
34. Seni J, Falgenhauer L, Simeo N, et al. Multiple ESBL-producing Escherichia coli sequence types carrying quinolone and aminoglycoside resistance genes circulating in companion and domestic farm animals in Mwanza, Tanzania, Harbor Commonly Occurring Plasmids. Front Microbiol. 2016;7:142. doi:10.3389/fmicb.2016.00142
35. Perez F, Bonomo RA. Can we really use ß-lactam/ß-lactam inhibitor combinations for the treatment of infections caused by extended-spectrum ß-lactamase-producing bacteria? Clin Infect Dis. 2012;54(2):175–177. doi:10.1093/cid/cir793
36. Harris PNA, Tambyah PA, Lye DC, et al. Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA. 2018;320(10):984–994. doi:10.1001/jama.2018.12163
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.