Back to Journals » Advances in Medical Education and Practice » Volume 16
Assessing Knowledge of Radiation Protection and Safety Among Undergraduate and Intern Radiologic Technologists: A Pre- and Post-Educational Course Survey
Authors Alamoudi D , Ahmed ME, Alhalwani AY , Alnakhli AT, Qahaf RM, Bazuhayr LF, Yamani BH
Received 7 February 2025
Accepted for publication 9 May 2025
Published 3 July 2025 Volume 2025:16 Pages 1151—1158
DOI https://doi.org/10.2147/AMEP.S521381
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sateesh B Arja
Dalal Alamoudi,1,2 Mohamed Eldigire Ahmed,1,2 Amani Y Alhalwani,1,2 Alhassan Talal Alnakhli,3 Raghad Mohammed Qahaf,3 Lama Fahad Bazuhayr,3 Byadr Hassan Yamani3
1Department of Basic Sciences, College of Science and Health Professions, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia; 2Research Office, King Abdullah International Medical Research Center, Jeddah, Saudi Arabia; 3Department of Radiological Sciences, College of Applied Medical Sciences, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
Correspondence: Dalal Alamoudi, Email [email protected]
Introduction: Radiation protection aims to reduce unnecessary exposure to ionizing radiation, protecting patients and healthcare workers. Although diagnostic imaging techniques contribute minimally to overall exposure, risks still exist. Radiologic technologists perform X-ray procedures in diverse settings, collaborating with medical teams to ensure quality patient care. The Radiological Sciences program delivers comprehensive education and clinical training in anatomy, radiation safety, patient positioning, and imaging techniques. This study assesses the effectiveness of educational interventions in enhancing students’ understanding of principles of radiation physics, protection, and safety guidelines, preparing them for responsible clinical and research practices.
Methods: A cross-sectional, in-person survey was conducted among undergraduate and intern students in the Radiological Sciences Department at King Saud bin Abdulaziz University for Health Sciences (KSAU-HS) in Jeddah. The Healthcare Professional Knowledge of Radiation Protection (HPKRP) scale was distributed via Google Forms. Data were analyzed using SPSS (v.29). Differences in HPKRP components between students’ stages were examined using an unpaired samples t-test and ANOVA.
Results: Undergraduate students in their third and fourth years, as well as interns who completed post-educational courses, scored significantly higher than second-year students without prior coursework in medical radiation imaging. Participants with post-educational courses and training in ionizing radiation demonstrated the highest knowledge levels in radiation physics, biology, and principles of radiation use (mean: 9.2 ± 0.8), followed by radiation protection (mean: 8.9 ± 1.2). Knowledge of safe ionizing radiation use guidelines scored slightly lower (mean: 8.5 ± 1.6).
Conclusion: Structured radiation education significantly enhances students’ knowledge of radiation physics, protection, and safety guidelines. Significant improvements were observed between the second and third academic stages, as well as among interns, with stable retention in later stages. Early integration and continuous education for promoting a strong culture of radiation safety and responsible practice across clinical and research environments.
Keywords: ionizing radiation, radiation protection knowledge, healthcare professional knowledge of radiation protection, HPKRP, radiologic technologists, educational courses
Introduction
Ionizing radiation in the medical field is an essential tool for diagnosing and treating a range of medical conditions. Various diagnostic imaging modalities, including computed tomography, mammography, and nuclear imaging, are minor contributors to the cumulative dose exposures received by healthcare personnel. Nevertheless, any exposure to radiation presents potential risks for both patients and healthcare workers.1,2 Therefore, radiation protection is a vital practice designed to minimize unnecessary exposure to ionizing radiation, thereby reducing its harmful effects on both healthcare providers and patients.3 The principles of radiation protection are based on three fundamental principles: justification, optimization, and dose limitation. The risks associated with ionizing radiation in the radiology department can be avoided by following the As Low As Reasonably Achievable (ALARA) principle, mandated by federal regulations. This principle emphasizes the necessity of implementing all possible measures to minimize radiation exposure, including shielding, increasing distance from the radiation source, and reducing the duration of exposure.4
Over the past decade, several studies involving groups of physicians, radiologists, and radiographers have highlighted a concerning deficiency in their understanding of radiation protection. Many of these professionals underestimated the radiation doses associated with various imaging methods, and in some instances, they were unable to accurately differentiate between ionizing and non-ionizing radiation imaging techniques.5–10 Radiographers, commonly referred to as radiologic technologists, diagnostic radiographers, or medical radiation technologists, are healthcare professionals who use medical imaging equipment to perform X-ray examinations in various settings, including hospitals, physician’s offices, clinics, medical imaging centers, surgical centers, and mobile imaging agencies. They collaborate with other medical professionals to ensure high-quality outcomes and enhance the patient experience.11 The key responsibilities of radiologic technologists include accurately positioning patients and producing quality diagnostic images. They work closely with radiologists—physicians who interpret these medical images for diagnostic purposes. The technologist performs proper imaging procedures to ensure accurate interpretation.12,13
Radiologic Technology holds a distinct position within the medical sciences. Students in this field are trained in various imaging modalities that utilize ionizing radiation—such as radiography, computed tomography (CT), radiotherapy, and nuclear medicine—as well as non-ionizing radiation techniques, including magnetic resonance imaging (MRI) and ultrasonography.14 The primary objective of this program is to establish a strong educational foundation, enabling students to gain hands-on experience and become proficient in using advanced imaging technologies in medical radiography.15 Proper instruction in radiologic technology is essential not only for students but also for technologists and radiologists.16 While the educational structure and objectives of Radiologic Technology programs show considerable consistency across universities, a comparative analysis of curricula from different countries found no significant differences in core content and structure.15 In general, Radiologic Technology programs offer a rigorous curriculum that integrates both theoretical knowledge and practical expertise to ensure accurate disease diagnosis.17 The program is typically delivered as a full-time course, combining academic study and hospital internship.15 In most universities, the early stages of the program focus on general education and foundational specialized courses, including anatomy, physiology, pathology, patient care, radiation physics, examination procedures, equipment protocols, quality management, radiologic imaging, radiation protection, and radiobiology.15 At the later phase of the program, students further develop knowledge in sophisticated imaging technologies, covering modalities such as CT, ultrasound, MRI, diagnostic imaging, nuclear medicine, and interventional radiology. Each modality is presented with a review of the relevant physics, fundamental principles, imaging techniques, and applications in clinical practice. Additionally, most programs include training in research methods and offer students opportunities for extensive hospital internships. In certain institutions, such as the one mentioned by Gholami M [15], students are also required to conduct research and to defend a thesis or research article as part of the requirements for graduation. While this level of research engagement reflects a model of best practice approach to cultivating critical thinking and evidence-based practice, it is not a universal requirement across all Radiologic Technology programs, particularly in countries such as the United States. Graduates of the program are well-prepared to engage with multidisciplinary healthcare teams and contribute to community health promotion through their expertise in medical imaging and radiation safety.15
This study evaluates students’ knowledge and awareness of radiation protection and safety following educational interventions. The Healthcare Professional Knowledge of Radiation Protection (HPKRP) scale will be utilized among undergraduate students and interns in the Radiological Science Department at King Saud bin Abdulaziz University for Health Sciences (KSAU-HS) in Jeddah, Saudi Arabia. This is essential to ensure that future radiologic technology professionals are adequately equipped with the necessary knowledge to promote safety in clinical and research settings.
Methodology
Study Design
A prospective cross-sectional questionnaire was conducted to assess radiation knowledge and identify specific deficiencies among undergraduate and intern students enrolled in the Radiological Science Department at KSAU-HS in Jeddah. A total of 80 students participated in the survey. The questionnaires were distributed from October 1, 2024, to November 30, 2024. This study included all undergraduate and intern students to evaluate their knowledge of radiation protection and safety using the validated Healthcare Professional Knowledge of Radiation Protection (HPKRP) scale.18 Notably, the HPKRP scale was previously validated by Hirvonen et al using Cronbach’s alpha coefficients.19
Questionnaire Details
A validated, self-administered questionnaire was divided into two main sections. The first section consisted of demographic questions, including gender, age group, academic stage, educational level, prior training in ionizing medical facilities, and information about medical radiation courses. The second section comprised the Healthcare Professional Knowledge of Radiation Protection (HPKRP) scale, which assesses medical radiation knowledge through a total of 33 items across three main domains:
1. Radiation Physics and Principles of Radiation Use (12 items).
2. Radiation Protection (13 items).
3. Guidelines for Safe Ionizing Radiation Use (8 items).
The HPKRP scale, developed by T. Schroderus-Salo et al18 was employed to assess the radiation knowledge of undergraduate students in the second stage (pre-educational courses) and the third and fourth stages, as well as interns (post-educational courses), in the Radiological Sciences department at KSAU-HS, Jeddah, Saudi Arabia.
Statistical Analysis
Data collected were organized on an Excel sheet and analyzed using SPSS statistical software (v.29). Categorical variables were presented in frequencies and percentages, while the quantitative HPKRP Scale variables were summarized in means and standard deviations. The differences in HPKRP components between students’ stages were examined using unpaired samples t-test and ANOVA test. A P-value of 0.05 or less was considered significant. Participants assessed their radiation knowledge based on specified items using a 10-point Likert scale, ranging from 1 (indicating no knowledge) to 10 (indicating full knowledge), with 5 representing moderate knowledge. This scale was designed to gather detailed information regarding participants’ self-reported understanding of various aspects of radiation and its application. The “Low” category included scores ranging from 1.00 to 4.99, while the “High” category included scores ranging from 5.00 to 10.00.19,20 The findings were analyzed and presented as odds ratios (OR) with 95% confidence intervals (CI), and statistical significance was determined with a p-value of < 0.05.
Ethical Considerations
The study was approved by the institutional review board at King Abdullah International Medical Research Center, Jeddah, Saudi Arabia (NRJ24/018/8). This study was prospective; it was conducted with participants’ informed consent.
Results
The demographic analysis of the study sample provided valuable insights into the distribution of participants based on gender, age, academic stage, and exposure to ionizing radiation education and training. From the demographic information of 80 undergraduate students and interns from the Radiological Sciences department, 46.3% were female, while 53.7% were male. The demographic data revealed that most participants were in the 18–20 age group, comprising 48.8% of the sample, followed by the 21–23 age group, which accounted for 51.2%. Regarding the academic stage, 45% of participants were in their second year, 15% in their third year, 18.7% in their fourth year, and 21.3% were interns. Regarding ionizing radiation education, 62.5% of participants received lectures, 5% attended tutorials/workshops, and 32.5% experienced both methods. 38.7% had not received training in ionizing medical facilities from second-year undergraduate students, while the remaining 61.3% had undergone such training. Most participants (95%) agreed on the importance of providing radiation protection courses for students in health professions, as shown in Table 1.
 |
Table 1 Summary of Demographic Information of Participating Undergraduate Students and Interns |
Table 2 illustrates the items and sub-categories of competency within the HPKRP scale, comparing the mean and standard deviation for the three main components of radiation knowledge between pre- and post-educational courses. Among the undergraduate students in their third and fourth years, as well as the interns surveyed, the highest mean score was observed in their understanding of radiation physics, biology, and principles of radiation use 9.2 ± 0.8. This was followed by their knowledge of radiation protection 8.9 ± 1.2, while the lowest mean score was recorded in their knowledge of the guidelines for safe ionizing radiation use 8.5 ± 1.6. In contrast, second-year undergraduate students surveyed before the educational course demonstrated lower scores across all three components: understanding of radiation physics, biology, and principles of radiation use 3.5 ± 1.5, knowledge of radiation protection 3.5 ± 1.6, and knowledge of guidelines for safe ionizing radiation use 3.5 ± 1.5.
 |
Table 2 Main Factors and Competency Items in the Healthcare Professional Knowledge of Radiation Protection (HPKRP) Scale: Comparison of Pre- and Post-Educational Course Results |
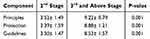 |
Table 3 Comparison of Participants’ Responses on the HPKRP Components Between the Second Stage and Third and Above Stages Students |
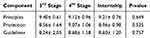 |
Table 4 Comparison of Participants’ Responses on the HPKRP Components Among Post-Course Students Across the Third Stage, Fourth Stage, and Internship |
Table 3 presents a comparison of participants’ responses across student stages, specifically second-stage students and those in the third stage and above, across three components: radiation physics, biology, and principles of radiation use (Principles); radiation protection (Protection); and guidelines for the safe use of ionizing radiation (Guidelines). The data revealed that there were significant differences between these stages for all components. For the Principles component, second-stage students reported a mean score of 3.52 ± 1.49, while third-stage and above students demonstrated a much higher mean score of 9.22 ± 0.79 (p = 0.001). Similarly, for the Protection component, second-stage students had a mean score of 3.39 ± 1.59, whereas third-stage and above students scored 8.88 ± 1.21 (p = 0.001). Finally, for the Guidelines component, second-stage students reported a mean score of 3.50 ± 1.47, while third-stage and above students scored 8.53 ± 1.57 (p = 0.001).
Table 4 presents a comparison of the participants’ responses across three stages—the third stage, the fourth stage, and the internship—on three components: Principles, Protection, and Guidelines. Although there were some fluctuations in mean scores across the different stages, the data revealed no significant differences between these stages for any of the components. For the Principles component, third-stage students reported a mean score of 9.40 ± 0.61, fourth-stage students had a mean score of 9.12 ± 0.96, and the internship scored 9.21 ± 0.76 with a p-value of 0.649. For the Protection component, third-stage students reported a mean score of 8.56 ± 1.64, fourth-stage students scored 9.07 ± 1.06, and interns reported a mean score of 8.96 ± 0.98, with a p-value of 0.535. Finally, for the Guidelines component, third-stage students had a mean score of 8.24 ± 2.05, fourth-stage students scored 8.68 ± 1.58, and the internship reported 8.60 ± 1.20 with a p-value of 0.757.
Discussion
This study highlighted significant discrepancies in radiation knowledge among undergraduate students at different academic stages in the Radiological Sciences department, particularly between early-year students and those in their third year, fourth year, and interns. Using the HPKRP scale, the study assessed three main components: Radiation Physics, Biology, and Principles of Radiation Use (Principles); Radiation Protection (Protection); and Guidelines for Safe Ionizing Radiation Use (Guidelines). The observed increase in competency across all three components supports the integration of educational radiation courses early in the curriculum, followed by continuous reinforcement through advanced training and hands-on experiences. A substantial improvement in radiation knowledge was evident among students who completed educational courses, as indicated by the significant differences in mean scores across all three assessed components—Principles, Protection, and Guidelines. The strong statistical significance suggests that these differences are unlikely to be due to chance, underscoring the effectiveness of educational interventions in enhancing students’ understanding of radiation safety. The principles component demonstrated the greatest increase in mean scores from second-stage students to those in the third stage and beyond. This finding highlights the significant impact of education on students’ comprehension of fundamental radiation concepts. Conversely, previous studies,19,20 along with a recent study by Alamoudi et al (under press), reported that nurses scored lowest in the ‘Principles’ component of radiation knowledge. These lower scores may reflect gaps in formal radiation safety education during their academic training, particularly if such content was not adequately emphasized in the curriculum. The Guidelines component showed a relatively lower mean score, suggesting that while students gain theoretical and practical knowledge in radiation safety, there may still be gaps in their understanding of formal regulatory guidelines and compliance standards. This highlights the need for additional emphasis on institutional and international guidelines within the curriculum to ensure students develop a comprehensive understanding of best practices in radiation use. Overall, these findings emphasize the critical role of structured education in improving radiation knowledge and safety awareness among students. Additionally, as the differences in scores from the third stage to the internship were not statistically significant, this implies that students’ knowledge of Principles, Protection, and Guidelines remains relatively stable at these advanced stages. To the best of our knowledge, these results are incomparable with previous studies, as this scale has not been previously applied to undergraduate students in the radiological sciences department.
Limitations and Future Work
This study was conducted at a single institution, KSAU-HS, which may limit the generalizability of the findings to a broader population. However, despite the relatively small sample size, the study provides valuable insights into radiation knowledge among undergraduate students enrolled in the Radiological Sciences program. The findings highlight the need for future programs focused on radiation education, particularly through implementing targeted courses and practical training for undergraduate students in health professions who will work with or be exposed to radiation. Early integration principles of radiation protection and safety into academic curricula is essential to ensure students acquire a strong theoretical and practical foundation before entering clinical practice. Furthermore, enhancing awareness across various healthcare disciplines can contribute to the development of a more comprehensive safety culture within clinical environments.
Based on these findings, we recommend integrating a formal radiation safety module into undergraduate curricula across Saudi universities. Future research should consider multi-institutional studies with larger and more diverse samples to improve generalizability. Longitudinal studies may also provide deeper insights into long-term knowledge retention and the effectiveness of curriculum-based interventions on professional practice.
Conclusion
This study highlights the significant impact of structured radiation education on undergraduate students in their third and fourth years, as well as interns, in enhancing their knowledge and awareness about radiation physics, protection, and safety guidelines. The stability of knowledge retention in later stages suggests that structured coursework and practical exposure effectively prepare students for radiation safety in clinical and research settings. This is particularly crucial for nurses and other healthcare professionals exposed to radiation, as it helps minimize risks and strengthen safety protocols. Enhancing radiation protection training enables healthcare institutions to foster a culture of safety, ensuring the effective and safe use of medical radiation while reducing risks to healthcare professionals and patients.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgment
We express our gratitude and sincere thanks to all the students who took the time to answer the survey and participate in the research.
Funding
The authors report no funding associated with the work featured in this article.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Lakhwani OP, Dalal V, Jindal M, Nagala A. Radiation protection and standardization. J Clin Orthop Trauma. 2019;10(4):738–743. doi:10.1016/j.jcot.2018.08.010
2. Mitchell EL, Furey P. Prevention of radiation injury from medical imaging. J Vasc Surg. 2011;53(1):22S–27S. doi:10.1016/j.jvs.2010.05.139
3. Tsapaki V, Balter S, Cousins C, et al. The International Atomic Energy Agency action plan on radiation protection of patients and staff in interventional procedures: achieving change in practice. Physica Medica. 2018;52:56–64. doi:10.1016/j.ejmp.2018.06.634
4. National Council on Radiation Protection and Measurements. Medical x-ray and gamma-ray protection for energies up to 10 MeV: equipment design and use. Bethesda, MD: National Council on Radiation Protection and Measurements. 1968;(Report 33).
5. Zhou G, Wong D, Nguyen L, Mendelson R. Student and intern awareness of ionising radiation exposure from common diagnostic imaging procedures. J Med Imaging Radiat Oncol. 2010;54(1):17–23. doi:10.1111/j.1754-9485.2010.02132.x
6. Lee RKL, Chu WCW, Graham CA, Rainer TH, Ahuja AT. Knowledge of radiation exposure in common radiological investigations: a comparison between radiologists and non-radiologists. Emerg Med J. 2012;29(4):306–308. doi:10.1136/emermed-2011-200481
7. Günalp M, Gülünay B, Polat O, et al. Ionising radiation awareness among resident doctors, interns, and radiographers in a university hospital emergency department. Radiol Med. 2014;119(6):440–447. doi:10.1007/s11547-013-0374-8
8. Faggioni L, Paolicchi F, Bastiani L, Guido D, Caramella D. Awareness of radiation protection and dose levels of imaging procedures among medical students, radiography students, and radiology residents at an academic hospital: results of a comprehensive survey. Eur J Radiol. 2017;86:135–142. doi:10.1016/j.ejrad.2016.10.033
9. Abuhadi N. A study of student awareness of radiation protection skills at Jazan University. King Khalid Univ J Health Sci. 2019;4(1):6. doi:10.4103/1658-743X.292033
10. Jha PK, Thidwar R, Yadav P. Assessment of knowledge and awareness about basics of radiation and safety measures among allied health science professionals including radiographers and students of radiology and imaging technology: university based study. Int J Res Rev. 2022;9(7):244–248. doi:10.52403/ijrr.20220728
11. Adler AM, Crr. Introduction to Radiologic and Imaging Sciences and Patient Care - E-Book: Introduction to Radiologic and Imaging Sciences and Patient Care - E-Book. Elsevier Health Sciences; 2015.
12. Mazal JR, Steelman CB. Technologists role in global health radiology. Radiology in Global Health. 2014;75–84. doi:10.1007/978-1-4614-0604-4_9
13. Patti JA, Berlin JW, Blumberg AL, et al. ACR white paper: the value added that radiologists provide to the health care enterprise. J Ame College Radiol. 2008;5(10):1041–1053. doi:10.1016/j.jacr.2008.06.003
14. Mm GN. Evaluating motivation and interest in choosing career or higher education study among radiology students in Tabriz University of Medical Sciences. Educ Dev Jundishapur. 2014;2014:1.
15. Gholami M. Evaluating the curriculum for BS of radiologic technology in Iran: an international comparative study. Entomol Appl Sci Lett. 2018;5(3–2018):48–59.
16. Jacob J, Paul L, Hedges W, et al. Undergraduate radiology teaching in a UK medical school: a systematic evaluation of current practice. Clin Radiol. 2016;71(5):476–483. doi:10.1016/j.crad.2015.11.021
17. Akimoto T, Caruana CJ, Shimosegawa M. A qualitative comparative survey of First Cycle radiography programmes in Europe and Japan. Radiography. 2009;15(4):333–340. doi:10.1016/j.radi.2009.04.002
18. Schroderus-Salo T, Hirvonen L, Henner A, et al. Development and validation of a psychometric scale for assessing healthcare professionals’ knowledge in radiation protection. Radiography. 2019;25(2):136–142. doi:10.1016/j.radi.2018.12.010
19. Hirvonen L, Schroderus-Salo T, Henner A, et al. Nurses’ knowledge of radiation protection: a cross-sectional study. Radiography. 2019;25(4):e108–e112. doi:10.1016/j.radi.2019.04.011
20. Rahimi AM, Nurdin I, Ismail S, Khalil A. Malaysian nurses’ knowledge of radiation protection: a cross-sectional study. Radiol Res Pract. 2021;2021:1–8. doi:10.1155/2021/5566654
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

