Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Association Between Weight-Adjusted Waist Index and Periodontitis: A Cross-Sectional Study and Mediation Analysis
Authors Yang H, Lu Y , Zhao L, He Y, He Y, Chen D
Received 2 September 2024
Accepted for publication 25 October 2024
Published 11 November 2024 Volume 2024:17 Pages 4235—4246
DOI https://doi.org/10.2147/DMSO.S491413
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Hao Yang,1 Yayun Lu,2 Lina Zhao,3 Yufeng He,1 Yuecheng He,4 Dong Chen5,6
1Department of Stomatology, Health Examination Center of Shanghai Health and Medical Center, Huadong Sanatorium, Wuxi, People’s Republic of China; 2Nursing Department, Health Examination Center of Shanghai Health and Medical Center, Huadong Sanatorium, Wuxi, People’s Republic of China; 3Department of Stomatology, The Affiliated Hospital of Inner Mongolia Medical University, Inner Mongolia Medical University, Hohhot, People’s Republic of China; 4Department of Oral and Maxillofacial Implantology, Shanghai Ninth People’s Hospital, Shanghai, People’s Republic of China; 5Department of Endodontics, Shanghai Stomatological Hospital & School of Stomatology, Fudan University, Shanghai, People’s Republic of China; 6Shanghai Key Laboratory of Craniomaxillofacial Development and Diseases, Fudan University, Shanghai, People’s Republic of China
Correspondence: Dong Chen, Department of Endodontics, Shanghai Stomatological Hospital & School of Stomatology, Fudan University, 356 East Beijing Road, Shanghai, 200001, People’s Republic of China, Email [email protected] Yufeng He, Department of Stomatology, Health Examination Center of Shanghai Health and Medical Center, Huadong Sanatorium, Wuxi, 214065, People’s Republic of China, Email [email protected]
Aim: The research examined the correlation between the weight-adjusted waist index (WWI) and periodontal disease, as well as the intermediary influence of triglyceride glucose (TyG) index-related indicators, utilizing a health examination dataset.
Methods: This cross-sectional study included 39,522 subjects from health check-up database of Shanghai Health and Medical Center. The WWI was determined by applying a formula that includes dividing the waist circumference (WC) by the body weight’s square root. Periodontitis diagnosis followed the Centers for Disease Control and Prevention and American Academy of Periodontology (CDC/AAP) classification. The correlation between the WWI and periodontitis was investigated through multivariate logistic regression and smoothing curve fitting. Subgroup analysis and interaction tests were also performed to verify the stability of the results. A mediation analysis was conducted to quantify the direct and indirect influences mediated by the TyG-related indicators [TyG, TyG -body mass index (TyG-BMI), TyG -waist-to-height ratio (TyG-WHtR), and TyG-waist circumference (TyG-WC)].
Results: Multivariable logistic regression analysis revealed the positive association of WWI and periodontitis (OR=1.37, 95% CI: 1.30– 1.43). Compared to those in the lowest quartile of WWI, participants in the highest quartile exhibited a 82% higher likelihood of periodontitis (OR=1.82, 95% CI: 1.69– 1.96). Subgroup analysis and interaction tests revealed that this positive correlation was consistent in gender, BMI, WC, smoking, drinking, hypertension, and dyslipidemia (P for interaction > 0.05), with some variations noted by age and diabetes status (P for interaction< 0.05). Mediation analysis showed that the proportions mediated by TyG, TyG-BMI, TyG-WC, and TyG-WHtR on the association of WWI and periodontitis risk were 13.13%, 6.30%, 16.46% and 19.79%, respectively.
Conclusion: A higher WWI in Chinese adults was linked to an increased likelihood of periodontitis, and this correlation could be partially explained by elevated levels of TyG index-related indicators.
Keywords: weight-adjusted waist index, periodontitis, triglyceride glucose index, mediating effect
Introduction
Periodontitis, characterized by chronic inflammation of the gums and the structures that support the teeth, can result in the loss of teeth among adults. This condition is quite common, affecting approximately 42% of the adult population in the United States and an estimated 11.2% of individuals worldwide in its more severe forms.1,2 The prevalence of periodontitis in China is estimated to be around 30%, which is a significant health concern.3 Beyond oral health implications, periodontitis has been linked to other systemic health concerns, such as metabolic syndrome and diabetes, where the inflammatory processes from periodontal disease can worsen these conditions.4,5 Studies have explored the interplay between obesity and periodontitis, suggesting that excess body weight may contribute to the severity of gum inflammation by increasing inflammatory markers and impairing insulin sensitivity.6,7
The assessment of obesity has advanced with the introduction of the weight-adjusted waist index (WWI), which provides a more detailed evaluation of central obesity compared to traditional measures like body mass index (BMI) and waist circumference (WC).8 Central obesity, characterized by excess visceral fat, is particularly concerning due to its strong link to metabolic issues and insulin resistance (IR).9,10 Iinsulin resistance, where the body’s cells fail to respond adequately to insulin, impairing glucose uptake and metabolism. The adipose tissue in the abdominal region, when excessive, also acts as an endocrine organ, secreting pro-inflammatory cytokines such as TNF-α and IL-6, which contribute to a state of chronic low-grade inflammation.11–13 This inflammation further exacerbates insulin resistance and is implicated in the development of metabolic syndrome, type 2 diabetes, and cardiovascular diseases.14–16 Abdominal obesity causes a chronic low-grade inflammatory state. This inflammation can worsen periodontal disease by increasing the production of pro-inflammatory cytokines and changing the immune response to periodontal pathogens.17 Prior research has established a distinct connection between central obesity and periodontal health, noting a synergistic increase in serum interleukin-1β particularly in those presenting with both conditions.18,19 Numerous investigations have pointed to a positive correlation between obesity and periodontitis, with reported odds ratios ranging from 1.1 to 4.5 for related inflammation or periodontal tissue breakdown.20 A study has shown a significant positive correlation between WWI and periodontitis, indicating that higher levels of central obesity, as measured by WWI, are associated with an increased risk of periodontitis.3
The WWI accounts for WC in relation to body weight, providing a more nuanced measure of central obesity and metabolic dysfunction, underscoring the significance of waist circumference as a more informative indicator than BMI or WC alone for assessing muscle and fat distribution, this index and offers a robust measure of fat and muscle levels, which is not as influenced by factors such as height and overall weight as BMI is, and it’s not solely dependent on waist size like WC.21 Numerous studies had demonstrated a direct link between WWI and the risk of developing hypertension, diabetes, alterations in bone mineral density, as well as both all-cause and cardiovascular mortality.22–26 The WWI could signify shifts in the composition of adipose and muscular tissues associated with aging, pertinent across the entire demographic spectrum, potentially offering a more precise gauge for forecasting the likelihood of chronic health conditions.27
The Triglyceride Glucose (TyG) index is a useful tool for estimating insulin sensitivity and has been found to be correlated with the risk of periodontitis.28 Combining TyG with obesity indices, such as TyG-WHtR, TyG-WC, and TyG-BMI, shows promise in better reflecting the risk of metabolic syndrome, diabetes, and potentially periodontitis than TyG alone.29–31 Despite the evidence linking obesity, insulin resistance, and periodontitis, the role of TyG index-related indicators in the association between central obesity and periodontitis is not well studied. This gap in knowledge is important to address, as understanding the mechanisms linking central obesity to periodontitis could help in developing more targeted interventions and preventive strategies.
In this cross-sectional study, we seek to examine the correlation and potential mediating mechanisms. Our findings present fresh insights into the influence of central obesity, as evaluated by WWI, on the prevalence of periodontitis and underscore the significance of TyG-related indicators in mediating this connection.
Methods
Study Population and Design
This research encompassed individuals aged 18 years and above who had undergone routine health assessments at the health examination center of Shanghai Health and Medical Center. Utilizing a random cluster sampling method to ensure a representative sample, the study initially identified several clusters, which were then randomly selected. From these chosen clusters, all eligible individuals were included in the study. To begin with, the study sample comprised 52,114 adults for this cross-sectional analysis. Exclusion criteria for participants were based on the following conditions: (1) incomplete medical information; (2) weight and waist circumference not available; (3) oral health examination not available; (4) pregnant participants. After excluding these individuals, a total of 39,522 participants were included in the study (Figure 1), consisting of 15,993 females and 23,529 males with average age of 47±12 years. In accordance with the ethical standards of the Declaration of Helsinki, this cross-sectional study received approval from the ethics committee of Health Examination Center of Shanghai Health and Medical Center (Wuxi, China). All participants provided written informed consent before study participation.
 |
Figure 1 Flowchart of study participants. |
Sample Size Estimation
To ensure our analysis was adequately powered, we conducted a power analysis using PASS 2021 software. With a 30% prevalence of periodontitis, the analysis revealed that we needed a sample size of 1329 participants to detect a significant effect at the 0.05 significance level with 80% power. Accounting for an estimated 10% non-response rate, we increased the sample size to 1462. Ultimately, our study enrolled 39,522 participants, exceeding our target sample size. This large sample size provides sufficient statistical power to identify significant associations within the data.
Assessment of Covariates
A standard questionnaire was employed to gather basic demographic data, including participants’ age, sex, and habits related to tobacco and alcohol consumption. For the purposes of this study, smoking was categorized based on a habit of smoking three or more cigarettes daily over the course of a year, and alcohol use was identified by regular intake, defined as three or more drinking occasions weekly, sustained for at least twelve months. Following a 12-hour overnight fast, fasting venous blood samples were obtained from all subjects enrolled in the study. Blood samples were collected by certified phlebotomists who are trained in venipuncture techniques and adhere to standard operating procedures to ensure sample integrity. Levels of fasting plasma glucose (FPG), triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), neutrophils (NE), and lymphocytes (LY) were measured using an automatic hematology analyzer. Strict quality control procedures were adhered to in the laboratory.
Furthermore, we gathered pertinent health data, inquiring about participants’ medical histories regarding hypertension or diabetes, and their medication regimens. Diabetes was identified through fasting blood glucose (FBG) levels of 7.0 mmol/L or higher, the use of insulin or hypoglycemic medications, or by self-reported diagnosis.32 Hypertension was diagnosed if systolic blood pressure (SBP) was 140 mmHg or higher, or diastolic blood pressure (DBP) was 90 mmHg or higher, coupled with the ongoing use of antihypertensive drugs.33 Dyslipidemia was characterized by total cholesterol (TC) levels of 5.2 mmol/L or more, low-density lipoprotein cholesterol (LDL-C) levels exceeding 3.4 mmol/L, high-density lipoprotein cholesterol (HDL-C) levels below 1.0 mmol/L, or triglycerides (TG) exceeding 1.7 mmol/L.34
The physical examination involved the measurements of blood pressure and anthropometric indices including height, weight, and waist circumference (WC). BMI was computed by the ratio of body mass in kilograms to the square of height in meters. The waist-to-height ratio (WHtR) was defined as the WC divided by standing height. After a rest period of at least five minutes, arterial pressure measurements, both systolic and diastolic, were taken on the right arm utilizing a sphygmomanometer, and the mean value of two such measurements was determined. WWI is an anthropometric metric based on WC and body weight, utilized for central obesity assessment. Each participant’s WWI was calculated utilizing the formula which involves the division of WC by the square root of the body weight, rounding the resulting value to two decimal places (WWI = WC/body weight1/2, where WC is in cm and body weight is in kg). An elevated WWI suggests a more pronounced level of obesity.8
Furthermore, the TyG index was determined using the formula: TyG = ln [fasting triglycerides (mg/dL) × fasting glucose (mg/dL) / 2].28 The TyG-BMI was derived by the product of the TyG index and BMI. Similarly, TyG-WC was obtained by multiplying the TyG index by WC, and TyG-WHtR was the result of the TyG index multiplied by the WHtR.35
Ascertainment of Periodontitis
Assessments for periodontitis was conducted by experienced dentists with a minimum of five years of clinical practice in periodontology. All examiners were calibrated to ensure consistent application of diagnostic criteria according to the American Academy of Periodontology guidelines for every study participant. The oral health status was evaluated by examining specific teeth: the maxillary right first molar, maxillary left central incisor, maxillary left first premolar, mandibular left first molar, mandibular right central incisor, and mandibular right first premolar. In cases where these teeth were absent, an alternative tooth was selected following the guidelines suggested by Fleiss et al.36 Various periodontal measurements, including probing depth (PD), clinical attachment level (CAL), and bleeding on probing (BOP), were recorded at six sites around each tooth using a standardized periodontal probe. The presence of periodontitis was determined based on the clinical criteria established by the joint efforts of the Centers for Disease Control and Prevention and the American Academy of Periodontology for epidemiological monitoring (CDC/AAP), Severe periodontitis was characterized by the presence of at least two non-adjacent interproximal sites with a clinical attachment level (CAL) of 6 mm or more, along with at least one interproximal site exhibiting a probing pocket depth (PPD) of 5 mm or greater. Moderate periodontitis was identified by either at least two non-adjacent interproximal sites with a PPD of 5 mm or more or at least two non-adjacent interproximal sites with a CAL of 4 mm or more.37 Moderate or severe periodontitis was indicative of periodontitis diagnosis, with cases of no or mild periodontitis serving as the comparative reference group.
Statistical Analysis
Data analyses were carried out utilizing SPSS version 23.0 and R software version 4.1. The Kolmogorov–Smirnov test was applied to determine the normality of the data distributions. Variables with a normal distribution were expressed as the mean (±standard deviation), those with a skewed distribution as the median [with interquartile range], and categorical variables were depicted as frequencies (and proportions). For comparing continuous variables between groups, either the one-way ANOVA or the Kruskal–Wallis H-test was utilized, whereas categorical variables were assessed using the chi-square test. A multivariable logistic regression analysis was conducted to investigate the relationship between WWI and the risk of periodontitis, with three different models accounting for potential confounders. Model 1 incorporated adjustments for sex and age, Model 2 further adjusted for smoking, drinking, and BMI, and Model 3 included additional adjustments for diabetes, hypertension, dyslipidemia, and NLR. We also employed restricted cubic splines with four knots positioned at the 5th, 35th, 65th, and 95th percentiles of the WWI distribution to model the potential non-linear relationship between WWI and periodontitis risk, stratified by gender. Additional subgroup analyses and interaction tests were performed to evaluate the stability of the association between WWI and periodontitis across different subgroups defined by gender, age, BMI, WC, smoking, drinking, hypertension, diabetes, and dyslipidemia. For subgroup analysis, participants were classified using the following criteria: age categories: 18–44 years (Young), 45–65 years (Middle-aged), over 65 years (Elderly); BMI Classifications: Below 24 kg/m2 (lean/normal subject), 24 kg/m2 and above (overweight/obese subject); Waist Circumference thresholds: men ≥90 cm, women ≥85 cm. Mediation analysis was conducted to explore the direct and indirect effects of WWI on periodontitis through TyG-related indices, using the “mediation” R package. A significance level of 0.05 was used for statistical tests.
Results
Baseline Characteristics of Study Populations
Table 1 outlines the clinical characteristics of 39,522 participants, with columns displaying stratified groups based on WWI quartiles. The average (SD) value of WWI for all participants was 9.92 (0.57) cm/kg 1/2, ranging from 7.49 to 12.65 cm/kg 1/2. All participants were divided into quartiles based on WWI values, namely 7.49–9.52 (1st quartile, n=9798), 9.52–9.91 (2nd quartile, n=10,016), 9.91–10.3 (3rd quartile, n=9778), and 10.3–12.65 (4th quartile, n=9930). Among all participants, 13,159 subjects (33.3%) were diagnosed as periodontitis, and it increased with the higher WWI quartiles (P for trend<0.001). Notable variations were observed across WWI quartiles with respect to age, sex, smoking, drinking, WC, BMI, WHtR, SBP, DBP, FPG, hypertension, diabetes, dyslipidemia, TG, TC, HDL-C, LDL-C, WBC and NLR (all P values<0.001). Besides, when contrasted with participants in the lowest quartile of WWI, those in the highest quartile were predominantly older adults, males, and more frequently engaged in smoking and drinking habits. They also exhibited a higher prevalence of comorbidities such as diabetes, hypertension, and dyslipidemia. Concurrently, an elevated WWI was typically associated with increased markers of WC, BMI, WHtR, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting plasma glucose (FPG), triglycerides (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), white blood cell count (WBC), and neutrophil-to-lymphocyte ratio (NLR), whereas the levels of high-density lipoprotein cholesterol (HDL-C) were found to be reduced. (P for trend<0.001).
 |
Table 1 Baseline Characteristics of All Participants |
Association Between WWI and Periodontitis by Gender
Table 2 summarizes the findings from the multivariate logistic regression analyses using three distinct models. A significant positive association was confirmed between WWI and the likelihood of periodontitis, which was consistently significant in all model iterations. After accounting for all potential confounding factors, a uniform increment in WWI by one unit was associated with a 37% higher likelihood of periodontitis (OR=1.37, 95% CI: 1.30–1.43). When stratified by gender, the odds ratios (95% CI) for the WWI-periodontitis link were 1.39 (1.31–1.48) for males and 1.31 (1.21–1.41) for females. This correlation was similarly stable when WWI was categorized into quartiles, with those in the highest quartile showing a markedly increased risk of periodontitis (OR=1.82, 95% CI: 1.69–1.96) compared to those in the lowest. This trend was evident in both males (OR=1.69, 95% CI: 1.55–1.84) and females (OR=1.47, 95% CI: 1.30–1.66). Additionally, we utilized a restricted cubic spline model to validate the potential non-linearity in the relationship between WWI and periodontitis, and the results indicated a non-linear positive correlation between WWI and periodontitis among all participants or stratified by gender (all P for non-linear<0.05) (Figure 2). Furthermore, increasing value of WWI significantly increased the periodontitis when WWI was above 9.89 for all subjects, 10.07 for male and 9.69 for female, but showed a significant protective effect below this value.
 |
Table 2 Multivariable Regression Analysis of Association Between WWI and Periodontitis Risk |
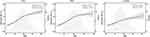 |
Figure 2 Dose-relationship between WWI and periodontitis by gender. |
Subgroup Analysis
We performed a stratified analysis to evaluate the consistency of our results, categorized by gender, age, BMI, WC, smoking habits, alcohol consumption, hypertension, diabetes, and dyslipidemia, with adjustments for potential confounding variables. The specific outcomes of these subgroups are depicted in Figure 3. The correlation between WWI and periodontitis proved to be robust across a variety of subgroups. Moreover, our data indicated that the association between WWI and periodontitis was consistent irrespective of gender (male/female), BMI (below 24 kg/m² / 24 kg/m² or above), WC [for males (below 90 cm) and females (below 85 cm) / for males (90 cm or above) and females (85 cm or above)], smoking (yes/no), alcohol use (yes/no), hypertension (yes/no), and dyslipidemia (yes/no) (all P for interactions>0.05). However, a notable interaction was identified concerning age and diabetes status (all P-values for interaction were 0.001), implying that the influence of WWI on periodontitis might differ with respect to age group and diabetes status, with a more pronounced impact in younger, non-diabetic individuals.
 |
Figure 3 Subgroup analysis. |
Mediation Analysis Through TyG-Related Indicators
Figure 4 presents that mediating effect of TyG-related parameters on the association between WWI and periodontitis risk. This study revealed a significant indirect effect of WWI and periodontitis risk (all P value<0.001). The proportions mediated by TyG, TyG-BMI, TyG-WC, and TyG-WHtR on the association of WWI and periodontitis risk were 13.13%, 6.30%, 16.46% and 19.79%, respectively. Additionally, the results also show a significantly direct and indirect coefficients between WWI and periodontitis through TyG, TyG-BMI, TyG-WC and TyG-WHtR (all P value<0.001).
 |
Figure 4 Mediation analyses of the association between WWI and periodontitis through TyG-related indicators. ***, P value<0.001. |
Discussion
In this comprehensive cross-sectional analysis involving 39,522 participants, a positive correlation was observed between the weight-adjusted waist index (WWI) and the incidence of periodontitis. This finding points to a probable connection between WWI and an increased risk of periodontitis. Upon closer inspection, after categorizing the data based on factors such as gender, BMI, WC, smoking habits, alcohol consumption, hypertension, and dyslipidemia, the association between WWI and periodontitis remained strong. This suggests a consistent positive connection across these subgroups, with the impact of different age ranges and diabetes status being particularly significant. Besides, the mediation analysis further revealed that the TyG index and its related obesity measures—TyG-BMI, TyG-WC, and TyG-WHtR—partially mediated this relationship, accounting for 13.13%, 6.30%, 16.46%, and 19.79% of the effect, respectively.
A thorough analysis of a large participant pool has recognized the WWI as a more precise predictor of cardiometabolic outcomes and mortality compared to traditional metrics like BMI, WC, and Waist-to-Height ratio.8 Consequently, in this analysis, we adopted WWI as an innovative metric for gauging central obesity and its influence on body fat distribution, aiming to delve into its association with periodontitis. Our results underscored a substantial positive correlation between WWI and the incidence of periodontitis. These insights underscore the importance of stringent WWI monitoring as part of obesity management, potentially serving as an additional tactic for bolstering periodontal wellness.
The correlation between WWI and periodontitis was identified as substantial across a spectrum of age cohorts, with a more pronounced effect in younger subjects. Overall, the association between obesity and periodontitis onset appears to be more intense among the younger and middle-aged demographics relative to the elderly. This variance might stem from several elements. It’s possible that older adults, having already experienced some tooth loss, may retain healthier dentition. Furthermore, the natural aging process, which includes increased oxidative stress and reduced physical activity, could contribute to a rise in adiposity.38,39 This insight implies that weight gain among the elderly who are obese might be an outcome of senescence, whereas in younger cohorts, obesity might originate from earlier life stages. Lastly, the lifestyle discrepancies between younger and older groups, with the former potentially engaging more frequently in unhealthy eating patterns, such as excessive sugar and fat consumption, could intensify the connection between obesity and periodontal health issues.40 Additionally, the link between WWI and periodontitis is believed to be more significant in individuals without diabetes compared to those with diabetes. This difference can be attributed to various physiological and metabolic factors that affect how adiposity interacts with periodontal health. Non-diabetic individuals typically have better insulin sensitivity than diabetic patients. In diabetic patients, the presence of high blood glucose and advanced glycation end products may already be causing inflammation, potentially masking the additional inflammatory effects of obesity. Adipose tissue releases different adipokines, like leptin and adiponectin, which help regulate the immune system and inflammation.14 Non-diabetic individuals with abdominal obesity may have an imbalanced release of these adipokines, contributing to periodontal inflammation. On the other hand, diabetic patients may have an altered adipokine profile due to their condition, affecting their susceptibility to periodontitis differently. Furthermore, non-diabetic individuals with abdominal obesity may engage in unhealthy behaviors, like poor diet and lack of physical activity, that independently raise the risk of periodontitis.41,42 In diabetic patients, the focus on managing blood glucose levels may overshadow the importance of oral health, leading to differences in how periodontal disease presents.
The underlying biological mechanism connecting central obesity WWI to periodontitis remains incompletely understood. Abdominal obesity is increasingly recognized as a critical factor in the development of periodontitis, a chronic inflammatory disease affecting the supporting structures of teeth. The pathophysiological mechanisms linking these two conditions are multifaceted, involving insulin resistance, chronic inflammation, and adipose tissue dysfunction. Insulin resistance, a key mediator in the relationship between abdominal obesity and periodontitis, triggers a cascade of inflammatory responses that impair the immune system’s ability to combat periodontal pathogens.43 This dysregulation exacerbates periodontal inflammation and bone loss, establishing a direct link between central adiposity and the progression of periodontal disease,44,45 and our results also showed that insulin resistance indicators including TyG index and its related indices significantly mediated the association between WWI and periodontitis. The TyG index has emerged as a significant marker for insulin resistance and is increasingly being recognized for its potential in predicting various metabolic disorders and cardiovascular diseases.29,30 Recent study have highlighted its clinical utility in assessing the risk of conditions like periodontitis, which is particularly relevant given the link between metabolic health and oral diseases.28 The TyG index offers a simple and accessible measure that could be integrated into routine health assessments to identify individuals at higher risk of metabolic complications, including periodontal issues. Insulin resistance fosters an inflammatory milieu characterized by increased production of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). These cytokines can exacerbate periodontal inflammation and impair the host’s immune response to periodontal pathogens, thereby promoting periodontal tissue destruction.46 Moreover, adipose tissue in obese individuals secretes various adipokines, including leptin, which can modulate immune cell function and contribute to the progression of periodontitis.47 Elevated levels of leptin have been associated with increased bone resorption and alveolar bone loss, a hallmark of periodontal disease.48 Additionally, the infiltration of immune cells into adipose tissue can lead to the release of reactive oxygen species, further exacerbating oxidative stress and tissue damage in periodontal tissues.49 The relationship between abdominal obesity and periodontitis is further complicated by the systemic effects of obesity, such as endothelial dysfunction and increased oxidative stress, which can impair the blood supply to periodontal tissues and reduce their resistance to infection.50,51 These mechanisms collectively contribute to the increased susceptibility to periodontitis observed in individuals with abdominal obesity.
Nevertheless, the study acknowledges several inherent limitations. Initially, the cross-sectional nature of the research precludes us from asserting a direct causal link between WWI and the incidence of periodontitis. Moreover, the generalizability of our results is constrained to the Chinese demographic, and their applicability to other ethnic or geographic groups remains uncertain. Additionally, the focus was solely on the detection of periodontitis, with no assessment of its severity, which limits our ability to assess whether the association with WWI varies with the condition’s intensity. Finally, the research did not account for a comprehensive range of potential confounding variables, including dietary habits—such as the intake of dietary fiber or high levels of carbohydrates—or physical activity levels, which could influence the correlation between WWI and periodontal health. Subsequent research should adopt a longitudinal approach, encompass diverse populations, and account for extra variables such as dietary intake and physical activity levels.
Conclusion
This study demonstrates that a high WWI is associated with an increased risk of periodontitis, with this relationship differing among various age groups and diabetes statuses. The TyG index-related obesity indicators may partially account for this association. However, further validation through additional prospective studies is necessary.
Data Sharing Statement
The datasets that were employed and/or analyzed in the current study are accessible from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
We confirm that this research adhered to the principles outlined in the Declaration of Helsinki. Ethical approval was granted by the Health Examination Center’s ethics committee at the Shanghai Health and Medical Center (approval number: SHMC-2024-12). Prior to their participation, all participants provided their informed consent.
Acknowledgments
Our gratitude is extended to all personnel who participated in this research for their diligent work in performing the data collection process. Hao Yang, and Yayun Lu should be considered the co-first authors of this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the “Research on health management strategy and application of elderly population” (NO.GWVI-11.1-28).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA, Genco RJ. Periodontitis in US adults: national health and nutrition examination survey 2009-2014. J AM DENT ASSOC. 2018;149:576–588. doi:10.1016/j.adaj.2018.04.023
2. Takedachi M, Shimabukuro Y, Sawada K, et al. Evaluation of periodontitis-related tooth loss according to the new 2018 classification of periodontitis. Sci Rep. 2022;12:11893. doi:10.1038/s41598-022-15462-6
3. Xu L, Liu Y, Zhao C, Wang J, Zhou H. Association between weight-adjusted waist index and periodontitis: a population-based study. PLoS One. 2024;19:e305010.
4. Pirih FQ, Monajemzadeh S, Singh N, et al. Association between metabolic syndrome and periodontitis: the role of lipids, inflammatory cytokines, altered host response, and the microbiome. PERIODONTOL 2000. 2021;87:50–75. doi:10.1111/prd.12379
5. D’Aiuto F, Gkranias N, Bhowruth D, et al. Systemic effects of periodontitis treatment in patients with type 2 diabetes: a 12 month, single-centre, investigator-masked, randomised trial. Lancet Diabetes Endocrinol. 2018;6:954–965. doi:10.1016/S2213-8587(18)30038-X
6. Pamuk F, Kantarci A. Inflammation as a link between periodontal disease and obesity. PERIODONTOL 2000. 2022;90:186–196. doi:10.1111/prd.12457
7. Jepsen S, Suvan J, Deschner J. The association of periodontal diseases with metabolic syndrome and obesity. PERIODONTOL 2000. 2020;83:125–153. doi:10.1111/prd.12326
8. Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. 2018;8:16753. doi:10.1038/s41598-018-35073-4
9. Semmler G, Balcar L, Wernly S, et al. Insulin resistance and central obesity determine hepatic steatosis and explain cardiovascular risk in steatotic liver disease. Front Endocrinol. 2023;14:1244405. doi:10.3389/fendo.2023.1244405
10. Jha BK, Sherpa ML, Dahal BK, Singh JK. Prevalence of metabolic syndrome and its components in adults with central obesity at Janakpur Zone, Nepal. J Nepal Health Res Counc. 2021;18:681–685. doi:10.33314/jnhrc.v18i4.2890
11. Shirvanizadeh F, Eidi A, Hafezi M, Eftekhari-Yazdi P. Abdominal obesity may play a significant role in inflammation exacerbation in polycystic ovary syndrome patients. JBRA Assist Reprod. 2023;27:682–688. doi:10.5935/1518-0557.20230065
12. Zhao D, Cui H, Shao Z, Cao L. Abdominal obesity, chronic inflammation and the risk of non-alcoholic fatty liver disease. ANN HEPATOL. 2023;28:100726. doi:10.1016/j.aohep.2022.100726
13. Bray GA, Kim KK, Wilding J. Obesity: a chronic relapsing progressive disease process. A position statement of the world obesity federation. OBES REV. 2017;18:715–723. doi:10.1111/obr.12551
14. Huang X, Wang Q, Liu T, et al. Body fat indices as effective predictors of insulin resistance in obese/non-obese polycystic ovary syndrome women in the Southwest of China. ENDOCRINE. 2019;65:81–85. doi:10.1007/s12020-019-01912-1
15. Oh JY, Sung YA, Lee HJ. The visceral adiposity index as a predictor of insulin resistance in young women with polycystic ovary syndrome. Obesity. 2013;21:1690–1694. doi:10.1002/oby.20096
16. Ye Z, Hu T, Wang J, et al. Systemic immune-inflammation index as a potential biomarker of cardiovascular diseases: a systematic review and meta-analysis. Front Cardiovasc Med. 2022;9:933913. doi:10.3389/fcvm.2022.933913
17. Lalla E. Periodontal infections and diabetes mellitus: when will the puzzle be complete? J CLIN PERIODONTOL. 2007;34:913–916. doi:10.1111/j.1600-051X.2007.01140.x
18. Munoz-Torres FJ, Jimenez MC, Rivas-Tumanyan S, Joshipura KJ. Associations between measures of central adiposity and periodontitis among older adults. Oral Epidemiol. 2014;42:170–177. doi:10.1111/cdoe.12069
19. Satpathy A, Ravindra S, Thakur S, Kulkarni S, Porwal A, Panda S. Serum interleukin-1beta in subjects with abdominal obesity and periodontitis. OBES RES CLIN PRACT. 2015;9:513–521. doi:10.1016/j.orcp.2015.01.005
20. Khan S, Barrington G, Bettiol S, Barnett T, Crocombe L. Is overweight/obesity a risk factor for periodontitis in young adults and adolescents?: a systematic review. OBES REV. 2018;19:852–883. doi:10.1111/obr.12668
21. Ding C, Shi Y, Li J, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: a prospective cohort study. Nutr, Metab Cardiovasc Dis. 2022;32:1210–1217. doi:10.1016/j.numecd.2022.01.033
22. Huang X, Huang Y, Zhou H, Huang Z. Relationship between weight-adjusted-waist index and blood pressure as well as incident hypertension among middle-aged and elderly Chinese: a longitudinal study. Nutr, Metab Cardiovasc Dis. 2024;34(9):2095–2106. doi:10.1016/j.numecd.2024.06.006
23. Yu S, Wang B, Guo X, Li G, Yang H, Sun Y. Weight-adjusted-waist index predicts newly diagnosed diabetes in Chinese rural adults. J CLIN MED. 2023;13:12. doi:10.3390/jcm13010012
24. Cao T, Xie R, Wang J, et al. Association of weight-adjusted waist index with all-cause mortality among non-Asian individuals: a national population-based cohort study. NUTR J. 2024;23:62. doi:10.1186/s12937-024-00947-z
25. Han Y, Shi J, Gao P, Zhang L, Niu X, Fu N. The weight-adjusted-waist index predicts all-cause and cardiovascular mortality in general US adults. Clinics. 2023;78:100248. doi:10.1016/j.clinsp.2023.100248
26. Zhang Y, Wu H, Li C, et al. Associations between weight-adjusted waist index and bone mineral density: results of a nationwide survey. BMC ENDOCR DISORD. 2023;23:162. doi:10.1186/s12902-023-01418-y
27. Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH. Associations between weight-adjusted waist index and abdominal fat and muscle mass: multi-ethnic study of atherosclerosis. DIABETES METAB J. 2022;46:747–755. doi:10.4093/dmj.2021.0294
28. Lee YC, Lee JW, Kwon YJ. Comparison of the triglyceride glucose (TyG) index, triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio, and metabolic score for insulin resistance (METS-IR) associated with periodontitis in Korean adults. THER ADV CHRONIC DIS. 2022;13:374171247. doi:10.1177/20406223221122671
29. Raimi TH, Dele-Ojo BF, Dada SA, et al. Triglyceride-glucose index and related parameters predicted metabolic syndrome in Nigerians. Metab Syndr Relat Disord. 2021;19:76–82. doi:10.1089/met.2020.0092
30. Li X, Sun M, Yang Y, et al. Predictive effect of triglyceride glucose-related parameters, obesity indices, and lipid ratios for diabetes in a Chinese population: a prospective cohort study. Front Endocrinol. 2022;13:862919. doi:10.3389/fendo.2022.862919
31. Yan S, Wang D, Jia Y. Comparison of insulin resistance-associated parameters in US adults: a cross-sectional study. Hormones. 2023;22:331–341. doi:10.1007/s42000-023-00448-4
32. Wang L, Peng W, Zhao Z, et al. Prevalence and treatment of diabetes in China, 2013-2018. JAMA. 2021;326:2498–2506. doi:10.1001/jama.2021.22208
33. Wang JG, Zhang W, Li Y, Liu L. Hypertension in China: epidemiology and treatment initiatives. NAT REV CARDIOL. 2023;20:531–545. doi:10.1038/s41569-022-00829-z
34. Lu Y, Zhang H, Lu J, et al. Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China. JAMA Network Open. 2021;4:e2127573. doi:10.1001/jamanetworkopen.2021.27573
35. Dang K, Wang X, Hu J, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003-2018. CARDIOVASC DIABETOL. 2024;23:8. doi:10.1186/s12933-023-02115-9
36. Fleiss JL, Park MH, Chilton NW, Alman JE, Feldman RS, Chauncey HH. Representativeness of the ”Ramfjord teeth” for epidemiologic studies of gingivitis and periodontitis. Oral Epidemiol. 1987;15:221–224. doi:10.1111/j.1600-0528.1987.tb00525.x
37. Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J PERIODONTOL. 2015;86:611–622. doi:10.1902/jop.2015.140520
38. Fukagawa NK, Bandini LG, Young JB. Effect of age on body composition and resting metabolic rate. Am J Physiol. 1990;259:E233–E238. doi:10.1152/ajpendo.1990.259.2.E233
39. Tessari P. Changes in protein, carbohydrate, and fat metabolism with aging: possible role of insulin. NUTR REV. 2000;58:11–19. doi:10.1111/j.1753-4887.2000.tb01819.x
40. Cavadini C, Siega-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. ARCH DIS CHILD. 2000;83:18–24. doi:10.1136/adc.83.1.18
41. Al-Mashhadi AL, Poulsen CB, von Wachenfeldt K, et al. Diet-induced abdominal obesity, metabolic changes, and atherosclerosis in hypercholesterolemic minipigs. J DIABETES RES. 2018;2018:6823193. doi:10.1155/2018/6823193
42. Summer SS, Jenkins T, Inge T, Deka R, Khoury JC. Association of diet quality, physical activity, and abdominal obesity with metabolic syndrome z-score in black and white adolescents in the US. Nutr, Metab Cardiovasc Dis. 2022;32:346–354. doi:10.1016/j.numecd.2021.10.021
43. Ladeira L, Nascimento GG, Leite F, et al. Obesity, insulin resistance, caries, and periodontitis: syndemic framework. NUTRIENTS. 2023;16:15. doi:10.3390/nu16010015
44. Andriankaja OM, Munoz-Torres FJ, Vivaldi-Oliver J, et al. Insulin resistance predicts the risk of gingival/periodontal inflammation. J PERIODONTOL. 2018;89:549–557. doi:10.1002/JPER.17-0384
45. Nishimura F, Murayama Y. Periodontal inflammation and insulin resistance--lessons from obesity. J DENT RES. 2001;80:1690–1694. doi:10.1177/00220345010800080201
46. Tancharoen S, Matsuyama T, Abeyama K, et al. The role of water channel aquaporin 3 in the mechanism of TNF-alpha-mediated proinflammatory events: implication in periodontal inflammation. J CELL PHYSIOL. 2008;217:338–349. doi:10.1002/jcp.21506
47. Bastard JP, Dridi-Brahimi I, Vatier C, Fellahi S, Feve B. Biological markers of adipose tissue: adipokines. Ann Endocrinol. 2024;85:171–172. doi:10.1016/j.ando.2024.04.002
48. Motyl KJ, McCabe LR. Leptin treatment prevents type I diabetic marrow adiposity but not bone loss in mice. J CELL PHYSIOL. 2009;218:376–384. doi:10.1002/jcp.21608
49. Wang L, Kuang Z, Zhang D, Gao Y, Ying M, Wang T. Reactive oxygen species in immune cells: a new antitumor target. BIOMED PHARMACOTHER. 2021;133:110978. doi:10.1016/j.biopha.2020.110978
50. Zhao P, Xu A, Leung WK. Obesity, bone loss, and periodontitis: the interlink. Biomolecules. 2022;13:12. doi:10.3390/biom13010012
51. Arboleda S, Vargas M, Losada S, Pinto A. Review of obesity and periodontitis: an epidemiological view. Br Dent J. 2019;227:235–239. doi:10.1038/s41415-019-0611-1
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Relationship Between Four Non-Insulin-Based Indexes of Insulin Resistance and Serum Uric Acid in Patients with Type 2 Diabetes: A Cross-Sectional Study
Han R, Zhang Y, Jiang X
Diabetes, Metabolic Syndrome and Obesity 2022, 15:1461-1471
Published Date: 9 May 2022
Correlations Between TyG-Related Indices and Bone Health: A Cross-Sectional Study of Osteoporosis in a Rural Chinese Population
Jia F, Lu Y, Wen H, Tu J, Ning X, Wang J, Li P
Diabetes, Metabolic Syndrome and Obesity 2025, 18:1445-1458
Published Date: 7 May 2025

