Back to Journals » Vascular Health and Risk Management » Volume 20
Association of Lactate with Risk of Cardiovascular Diseases: A Two-Sample Mendelian Randomization Study
Authors Chang X, Zheng W, Zhao Y, Niku W, Deng B, Liu P, Wang Y
Received 6 September 2024
Accepted for publication 1 December 2024
Published 6 December 2024 Volume 2024:20 Pages 541—551
DOI https://doi.org/10.2147/VHRM.S488424
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Xindi Chang,* Wang Zheng,* Yingli Zhao, Wangkang Niku, Bing Deng, Ping Liu, Yiru Wang
Department of Cardiology, Longhua Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yiru Wang, Email [email protected]
Purpose: Studies consistently show abnormally high levels of lactate acid in cardiovascular disease patients, suggested that targeting lactate production may serve as potential strategies for the treatment in the future. However, observational results may be subject to residual confounding and bias.
Methods: This study used the dataset from GWAS database to examine confounding in epidemiologic associations between lactate and cardiovascular diseases. A genome-wide genetic association study using Mendelian randomization (MR) was performed from December 02, 2023 to January 15, 2024 to reduce confounding and enhance causal inference. Primary analysis was conducted using inverse-variance-weighted MR. All studies included patients predominantly of European ancestry.
Results: The association between lactate and cardiovascular diseases, including 60801 cases from coronary heart disease, 7018 cases from myocardial infarction, 14334 cases from coronary atherosclerosis, 60620 cases from atrial fibrillation, 54358 cases from hypertension, 71 cases from hypertrophic cardiomyopathy, 47309 cases from heart failure, 7055 cases from stroke, 7193 cases from cardioembolic ischemic stroke, 4373 cases from ischemic stroke caused by large vascular atherosclerosis, 2118 cases from pulmonary embolism, 1230 cases from peripheral artery disease, and 4620 cases from venous thromboembolism. Genetically predicted coronary atherosclerosis was associated with a higher risk of lactate level (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024); this association was also evident for peripheral artery disease (OR = 1.003; 95% CI (0.000, 0.005); P = 0.021). No genetically predicted associations were noted for the other cardiovascular diseases.
Conclusion: The findings of this study provide genetic evidence supporting a higher risk of lactate level only in coronary atherosclerosis and peripheral artery disease. However, no genetic association between lactate level and the other cardiovascular diseases.
Keywords: Mendelian randomization, atherosclerosis, peripheral artery disease, GWAS, single nucleotide polymorphisms
Introduction
Since cardiovascular diseases (CVDs) continue to be the world’s leading cause of mortality, there is a pressing need to find new and targeted diagnostic and therapeutic approaches.1 With an estimated yearly impact of more than $200 billion and an exponential growth in estimates by 2060, CVDs are the leading public health problems.2,3 CVDs include atherosclerosis (AS), myocardial infarction (MI), heart failure (HF), coronary heart disease (CHD) and so on, which effect the structure and function of the heart.
Since its discovery in 1780, lactate has been believed to be a metabolic waste product resulting from glycolysis with no primary physiological role.4,5 Recent years have seen a progressive identification of lactate’s cryptic significance as study has become more thorough. The relationship between lactate levels and CVDs has been controversial.6 Even though there have been many observational studies looking at the connections between LA level and CVDs, the results have been skewed due to confounding variables and uncertain causal direction.7–9
By reducing residual confounding and reverse causation, the Mendelian randomization (MR) strategy can enhance the causal inference when genetic variations are used as instrumental variables for an exposure (in this example, lactate).10 This approach uses genetic risk of disease as a stand-in for the actual disease within the context of instrumental variant analysis. In a manner comparable to a randomized clinical trial, this results in effective randomization to either high or low genetic risk of a disease, reducing the possibility of confounding and reverse causation.11 MR estimates may be seen as the projected impact of the exposure on the result, given a set of assumptions.12
Since allelic randomization always occurs before the start of disease, the MR analysis can avoid reverse causation bias when compared to typical observational research.13 Furthermore, by integrating genetic markers as instrumental variables (IVs) of exposures, random segregation and the independent assortment of genetic polymorphisms at conception allow the MR analysis to reduce the influence of confounding factors.14 The investigation of causation is made possible in part by the availability of extensive genome-wide association studies (GWASs).15 Because genetic data is publicly available, MR analysis is being routinely used to evaluate possible causal links between different exposures and CVDs.16
Therefore, the aim of this MR study was to comprehensively investigate the association of lactate level with the risk of 13 CVDs, including CHD, MI, coronary AS, atrial fibrillation (AF), hypertension, hypertrophic cardiomyopathy (HCM), HF, stroke, cardioembolic ischemic stroke (IS), IS caused by large vascular AS, pulmonary embolism (PE), peripheral artery disease (PAD), and venous thromboembolism (VTE).
Materials and Methods
Study Design and Data
We performed a comprehensive two-sample bidirectional MR study to investigate the causality between lactate levels and CVDs (Figure 1A). The schematic view of the study design, and the three key assumptions of MR are as follows: (I) single nucleotide polymorphisms (SNPs) are strongly associated with lactate level; (II) SNPs only affect CVDs via lactate level; (III) SNPs are independent of known confounders (Figure 1B). The validity of the MR method depends on the IVs being satisfied for the three key assumptions in two-stage approach. Initially, SNPs associated with lactate levels will be identified from the database and confirmed in our dataset. These SNPs will be considered valid IVs if they are associated with lactate level at a genome-wide significance level (P < 5×10^-6) and are not in linkage disequilibrium with each other (R^2 < 0.01).
All data used in this genome-wide genetic association study are deidentified publicly available. All cited data sources obtained participant informed consent and relevant ethical approval. The study was conducted from December 28, 2023 to July 15, 2024. Details of the studies used as data sources are outlined in eTable 1. This study is reported following recommendations by the Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization (STROBE-MR) reporting guideline.17
Instrumental Variants for Exposures
The exposure of this study considered lactate. Genome-wide SNPs associated with lactate levels were obtained from the MR Base GWAS Catalog (https://gwas.mrcieu.ac.uk/datasets/met-d-Lactate/). It included 114,802samples (males and females) and 12,321,875 SNPs from Europe, released in 2020 by Borges CM. Instrumental variants were selected if they were associated with exposure at a genomewide significance threshold of P < 5×10^-6. This was achieved by packages “VariantAnnotation”, “gwasglue”, “dplyr”, “tidyr”, and “CMplot” in R software. The Manhattan figure was shown in eFigure 1.
Harmonization and Clumping
Data harmonization will be conducted to ensure that SNP alleles are consistently coded with respect to the effect on lactate levels. Clumping will be performed to prune out SNPs in linkage disequilibrium with more strongly associated IVs. Since two-sample MR methods require that the instruments be independent and do not have Linkage Disequilibrium (LD) between them, we used the “clump_data” function in R available via the “TwoSampleMR” package. We pruned SNPs in LD (R^2 < 0.01) within a clumping distance of 1000 kb. Next, to test the strength and validity of the IVs, we calculated F-statistics for each variant and only included the variants associated with lactate at an F-statistic > 10.18 All effect alleles were aligned to the LA-increasing allele. Finally, the package “MendelianRandomization” in R software and PhenoScanner website (http://www.phenoscanner.medschl.cam.ac.uk/) were used to remove confounding factors (P < 1×10^-5). A list of instrumental variants used in the analysis for the exposures can be found in eTable 2.
Genetic Associations for Outcomes
Publicly available summary statistics from UK Biobank (UKB), European Bioinformatics Institute (EBI), and Integrative Epidemiology Unit (IEU) GWAS from the MR Base GWAS Catalog were used to obtain genetic variants associated with CVDs as the outcome. If multiple catalogs were available for extracting summary statistics for a given outcome, we chose the most recent and the one containing the most significant number of cases/controls to keep our analysis robust.
The association between the IVs for lactate and cardiovascular outcomes were evaluated using genetic association analysis. Cardiovascular outcomes included CHD, MI, coronary AS, AF, hypertension, HCM, HF, stroke, cardioembolic IS, IS caused by large vascular AS, PE, PAD, and VTE. Association tests were performed using logistic regression, adjusting for age, sex, principal components of ancestry, and other relevant confounders. The final lists of SNPs used of different CVDs in the analysis were shown in eTable 3–eTable 15.
Statistical Analysis
The primary method used for analysis was inverse-variance-weighted (IVW) MR with multiplicative random effects in all instances,19 the other four methods including MR Egger regression, weighted median (WM) analysis, simple mode method, and weighted mode method were also performed. Multiple MR methods allow robust estimates even if potential violations are encountered in the MR approach. In addition, using different methods allows for optimal MR analysis as they differ in efficiency, limitations, and strengths.20 IVW is the most efficient MR method and has the most considerable statistical power, but it assumes that all variants are valid or have no pleiotropy.21 On the other hand, the MR Egger regression is used to detect violations of assumptions or the presence of outliers in the MR method and performs well in terms of bias under the null and Type I error rate, but it lacks precision and has the lowest power to detect a positive effect.22,23 The WM method is robust in the presence of outliers and can provide firm estimates even when 50% of the IVs are invalid, but has high Type I error rate.22,23 The weighted mode-based estimation method generally has low bias and low Type I error rate inflation with up to 40 invalid instruments, but also has low power to detect a causal effect.23 If the results of five MR methods are different, we referred to the IVW result.
Heterogeneity in inverse-variance-weighted analyses and MR-Egger methods were estimated using the Cochran Q statistic. Additional sensitivity analyses were performed through MR-Egger regression to assess and address the key MR assumptions regarding instrumental variants. The MR-Egger intercept test to verify the potential pleiotropy. The assumptions were explored by removing confounding factors (P < 1×10^-5) and quantifying the strength of instruments using genome-wide significance level (P < 5×10^-6), R^2 (< 0.01) and F statistics (> 10).24
All statistical analysis was conducted in R software (version 4.3.2, R Foundation for Statistical Computing) using different packages, including “TwoSampleMR”, “MendelianRandomization”, “VariantAnnotation”, “gwasglue”, “dplyr”, “tidyr”, and “CMplot”. Results are presented as ORs with 95% confidence intervals. For all analyses, a p-value of less than 0.05 at 2- sided will be considered statistically significant.
Results
High Risk of Lactate Level in CVDs
Genetically predicted a higher risk of lactate level (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) associated with coronary AS, as illustrated in Figure 2C and Table 1. Sensitivity analyses revealed no evidence of directional pleiotropy for genetically predicted coronary AS (MR-Egger intercept P = 0.949) and no heterogeneity was noted (Q statistic = 10.961, P = 0.140 in IVW method; Q statistic = 10.968, P = 0.204 in MR Egger method) in eTable 16. The results of single SNP analysis are reported in eFigure 2C.
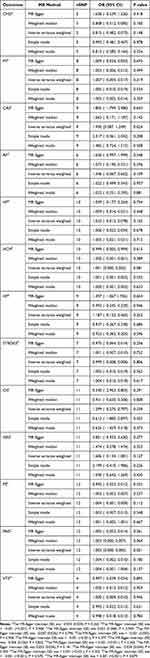 |
Table 1 MR Estimates for the Effect of Lactate of CVDs |
As shown in Figure 2L and Table 1, genetically predicted a higher risk of lactate level (OR = 1.003; 95% CI (0.000, 0.005); P = 0.021) associated with PAD. Sensitivity analyses revealed no evidence of directional pleiotropy for genetically predicted PAD (MR-Egger intercept P = 0.570). Significant heterogeneity was also not noted for PAD (Q statistic = 8.670, P = 0.564 in IVW method; Q statistic = 9.015, P = 0.620 in MR Egger method) in eTable 16. The results of single SNP analysis are reported in eFigure 2L.
Not Associated with High Risk of Lactate Level in CVDs
No association with lactate level genetically predicted in CHD (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2A), genetically predicted MI (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2B), genetically predicted AF (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2D), genetically predicted hypertension (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2E), genetically predicted HCM (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2F), genetically predicted HF (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2G), genetically predicted stroke (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2H), genetically predicted cardioembolic IS (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2I), genetically predicted IS caused by large vascular AS (OR = 1.950; 95% CI (0.087, 1.249) (Figure 2J); P = 0.024), genetically predicted PE (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2K), and genetically predicted VTE (OR = 1.950; 95% CI (0.087, 1.249); P = 0.024) (Figure 2M) were not associated with lactate level, as shown in Table 1.
Sensitivity analyses revealed no evidence of directional pleiotropy for genetically predicted CHD (MR-Egger intercept P = 0.265), MI (MR-Egger intercept P = 0.908), AF (MR-Egger intercept P = 0.796), hypertension (MR-Egger intercept P = 0.958), HCM (MR-Egger intercept P = 0.377), HF (MR-Egger intercept P = 0.822), stroke (MR-Egger intercept P = 0.265), cardioembolic IS (MR-Egger intercept P = 0.181), IS caused by large vascular AS (MR-Egger intercept P = 0.455), PE (MR-Egger intercept P = 0.302), and VTE (MR-Egger intercept P = 0.879) as shown in Table 1.
No significant heterogeneity was noted for CHD (Q statistic = 3.554, P = 0.314 in IVW method; Q statistic = 5.765, P = 0.217 in MR Egger method), HCM (Q statistic = 10.851, P = 0.210 in IVW method; Q statistic = 12.034, P = 0.211 in MR Egger method), stroke (Q statistic = 5.232, P = 0.388 in IVW method; Q statistic = 6.881, P = 0.332 in MR Egger method), IS caused by large vascular AS (Q statistic = 15.638, P = 0.075 in IVW method; Q statistic = 16.697, P = 0.081 in MR Egger method), PE (Q statistic = 20.044, P = 0.029 in IVW method; Q statistic = 22.423, P = 0.021 in MR Egger method), VTE (Q statistic = 1.640, P = 0.440 in IVW method; Q statistic =1.670, P = 0.644 in MR Egger method), although some heterogeneity was noted for MI (Q statistic = 17.857, P = 0.007 in IVW method; Q statistic = 17.900, P = 0.012 in MR Egger method), AF (Q statistic = 20.864, P < 0.001 in IVW method; Q statistic = 21.261, P = 0.001 in MR Egger method), hypertension (Q statistic = 98.478, P < 0.001 in IVW method; Q statistic = 98.514, P < 0.001 in MR Egger method), HF (Q statistic = 25.671, P = 0.001 in IVW method; Q statistic = 25.871, P = 0.001 in MR Egger method), cardioembolic IS (Q statistic = 18.124, P = 0.034 in IVW method; Q statistic = 22.350, P = 0.013 in MR Egger method) in eTable 16. The results of single SNP analysis are reported in eFigures 2A, B, D–K and M.
Discussion
Researchers have long been interested in the relationship between lactate level and CVDs. This work has made progress in clarifying the genetic relationships between lactate levels and different cardiovascular diseases by utilizing the GWAS database dataset. In order to give a more comprehensive picture of the function of lactate in CVDs, we sought to address the shortcomings of observational research, such as biases and residual confounding, by utilizing the MR approach.
Our results point to a correlation between genetically predicted lactate levels and coronary AS and PAD. This suggests that these diseases are more likely to occur in those who have a genetic propensity to produce more lactate. Despite the small confidence intervals, the ORs of 1.950 for PAD and 1.950 for coronary AS indicate a statistically significant association that calls for more research. These findings are consistent with previous research suggesting lactate is not only a metabolic waste product but also a signaling molecule that affects vascular smooth muscle cells and vascular remodeling.25–27 Blood lactate levels were found to be positively correlated with carotid atherosclerosis in a cross-sectional investigation of 1496 people, regardless of other cardiovascular risk factors.28
Studies on the relationship between lactate and PAD are limited. Lactate’s significance in peripheral vascular health is further supported by the hereditary link with PAD in our results. We speculate that the possible reason is that lactate may impair limb perfusion and contribute to the pathophysiology of illness by influencing muscle metabolism and vascular function. However, a clinical study suggests that lactate production is not directly correlated with improvement of endothelial function and walking abilities in PAD.29 Based on these, personalized medicinal methods are necessary since the genetic link may also indicate that individuals with a tendency for greater lactate levels may suffer different disease progression or response to therapy. With this specificity, tailored treatments for PAD and coronary AS may be developed. These treatments may involve changing the signaling pathways or lactate levels.
It’s interesting to note that lactate levels were not shown to be genetically predicted to be associated with other eleven types of CVDs. This might imply that more important genetic and environmental variables predominate under these situations, making lactate’s impact either insignificant or invisible. The specificity of lactate as a biomarker or therapeutic target is also called into doubt given its lack of relationship with other types of CVDs. It is possible that lactate’s involvement in CVDs is more complex than previously believed, and that treating lactate transport or synthesis will only help some subgroups of cardiovascular diseases. We review articles about relationship between lactate and CVDs, such as HF. In recent years, basic and clinical studies have reported the role of lactate in HF. Many studies have shown that high levels of lactate in the blood are a marker of poor prognosis in patients with HF.2,8 The role of lactate in acute and chronic HF seems to be different. Blood lactate levels significantly increase during acute HF, while in patients with chronic HF, there is little change in their blood lactate levels.30 Maybe that is one reason we drew the conclusion of no association between lactate and HF. For another example, several clinical investigations have demonstrated the strong predictive usefulness of circulating lactate levels in predicting worse clinical outcomes in patients with MI.31,32 But according to a different study, during the early stages of MI, monocytes’ lactylation of H3K18la stimulates the production of genes involved in cardiac repair, including IL-10, VEGF-A, and LRG1, which helps to heal infarcted hearts.33 All things considered, there is disagreement regarding lactate’s advantageous function in MI patients. The specific impact of lactate could vary depending on the cell types implicated in myocardial infarction, the stage of the illness, the existence of coexisting conditions, etc.6
When interpreting our findings, several important limitations must be considered. First, the predominance of European ancestry within the study population may limit the generalizability of our results to other ethnic groups. Cardiovascular disease is influenced by a complex interplay of genetic, socioeconomic, and lifestyle factors, many of which vary significantly across populations. This homogeneity in genetic background may obscure variant-disease associations that are relevant in other ancestries, potentially biasing the study’s conclusions. Future research should prioritize including ethnically and geographically diverse cohorts to ensure broader applicability and to uncover population-specific genetic and environmental interactions. Second, pleiotropy presents a critical challenge to the reliability of MR findings. Although MR is a powerful tool for causal inference, the possibility that genetic variants used as instrumental variables influence multiple traits beyond the exposure of interest remains a concern. Such horizontal pleiotropy can introduce bias, leading to spurious associations or an overestimation of causal effects. While statistical methods to detect and adjust for pleiotropy are increasingly robust, they are not foolproof. Future studies should incorporate rigorous sensitivity analyses and employ multiple complementary methods to strengthen the validity of MR conclusions.
Conclusion
In conclusion, our univariable MR analysis concludes that, with the exception of coronary AS and PAD, there is no evidence connecting lactate level to any of the 13 CVDs outcomes in the GWAS database. The genetic associations found with PAD and coronary AS may serve as a foundation for further investigation into the molecular mechanisms linking lactate to these illnesses. They also provide inspiring chances for the development of innovative therapeutic modalities. More study with a broader patient population and mechanistic studies is required to adapt these findings to therapeutic practice.
Abbreviations
MR, Mendelian randomization; CVDs, coronary vascular diseases; nSNP, number of single nucleotide polymorphisms; OR, odds ratio; CI, confidential interval; CHD, coronary heart disease; MI, myocardial infarction; CAS, coronary atherosclerosis; AF, atrial fibrillation; HP, hypertension; HCM, hypertrophic cardiomyopathy; HF, heart failure; CIS, cardioembolic ischemic stroke; ISAS, IS caused by large vascular atherosclerosis; PE, pulmonary embolism; PAD, peripheral artery disease; VTE, venous thromboembolism.
Acknowledgments
This study was supported by the National Natural Science Foundation to YRW [grant number 82204849], to PL [grant number 82074200]; Traditional Chinese Medicine Research Project of Shanghai Municipal Health Commission to YRW [grant number 2022QN056]; “Clinical research-oriented talents training program” in the Affiliated Hospital of Shanghai University of Traditional Chinese Medicine to YRW [grant number 2023LCRC01]; Clinical Technology Innovation Cultivation Program of Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine to YRW [grant number PY2022008]; Regional Medical Centre of Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine to YRW [grant number ZYZK001-029].
Ethics Statement
This study is exempt from ethics approval based on item 1 and 2 of Article 32 of the Measures for Ethical Review of Life Science and Medical Research Involving Human Subjects dated February 18, 2023, China. The details are as follows:
- Item 1 of Article 32: using legally obtained public data or conducting research through observation without interfering with public behavior.
- Item 2 of Article 32: using anonymized information data to conduct research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93–e621. doi:10.1161/CIR.0000000000001123
2. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596–e646. doi:10.1161/CIR.0000000000000678
3. Mohebi R, Chen C, Ibrahim NE, et al. Cardiovascular disease projections in the United States based on the 2020 census estimates. J Am Coll Cardiol. 2022;80(6):565–578. doi:10.1016/j.jacc.2022.05.033
4. Haas R, Cucchi D, Smith J, Pucino V, Macdougall CE, Mauro C. Intermediates of metabolism: from bystanders to signalling molecules. Trends Biochem Sci. 2016;41(5):460–471. doi:10.1016/j.tibs.2016.02.003
5. Ferguson BS, Rogatzki MJ, Goodwin ML, Kane DA, Rightmire Z, Gladden LB. Lactate metabolism: historical context, prior misinterpretations, and current understanding. Eur J Appl Physiol. 2018;118(4):691–728. doi:10.1007/s00421-017-3795-6
6. Ouyang J, Wang H, Huang J. The role of lactate in cardiovascular diseases. Cell Commun Signal. 2023;21(1):317. doi:10.1186/s12964-023-01350-7
7. Vermeulen RP, Hoekstra M, Nijsten MW, et al. Clinical correlates of arterial lactate levels in patients with ST-segment elevation myocardial infarction at admission: a descriptive study. Crit Care. 2010;14(5):R164. doi:10.1186/cc9253
8. Zymlinski R, Biegus J, Sokolski M, et al. Increased blood lactate is prevalent and identifies poor prognosis in patients with acute heart failure without overt peripheral hypoperfusion. Eur J Heart Fail. 2018;20(6):1011–1018. doi:10.1002/ejhf.1156
9. Biegus J, Zymlinski R, Sokolski M, Jankowska EA, Banasiak W, Ponikowski P. Elevated lactate in acute heart failure patients with intracellular iron deficiency as identifier of poor outcome. Kardiol Pol. 2019;77(3):347–354. doi:10.5603/KP.a2019.0014
10. Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32(1):1–22. doi:10.1093/ije/dyg070
11. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–525. doi:10.1093/ije/dyv080
12. de Leeuw C, Savage J, Bucur IG, Heskes T, Posthuma D. Understanding the assumptions underlying Mendelian randomization. Eur J Hum Genet. 2022;30(6):653–660. doi:10.1038/s41431-022-01038-5
13. Kim MS, Kim WJ, Khera AV, et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J. 2021;42(34):3388–3403. doi:10.1093/eurheartj/ehab454
14. Sanderson E, Glymour MM, Holmes MV, et al. Mendelian randomization. Nat Rev Meth Primers. 2022;2:6. doi:10.1038/s43586-021-00092-5
15. Bowden J, Holmes MV. Meta-analysis and Mendelian randomization: a review. Res Synth Methods. 2019;10(4):486–496. doi:10.1002/jrsm.1346
16. Larsson SC, Butterworth AS, Burgess S. Mendelian randomization for cardiovascular diseases: principles and applications. Eur Heart J. 2023;44(47):4913–4924. doi:10.1093/eurheartj/ehad736
17. Skrivankova VW, Richmond RC, Woolf BAR, et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ. 2021;375:n2233. doi:10.1136/bmj.n2233
18. Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan NA, Thompson JR. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Int J Epidemiol. 2016;45(6):1961–1974. doi:10.1093/ije/dyw220
19. Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–665. doi:10.1002/gepi.21758
20. Walker VM, Davies NM, Hemani G, et al. Using the MR-base platform to investigate risk factors and drug targets for thousands of phenotypes. Wellcome Open Res. 2019;4:113. doi:10.12688/wellcomeopenres.15334.2
21. Burgess S, Davey Smith G, Davies NM, et al. Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res. 2019;4:186. doi:10.12688/wellcomeopenres.15555.3
22. Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–314. doi:10.1002/gepi.21965
23. Burgess S, Foley CN, Allara E, Staley JR, Howson JMM. A robust and efficient method for Mendelian randomization with hundreds of genetic variants. Nat Commun. 2020;11(1):376. doi:10.1038/s41467-019-14156-4
24. Palmer TM, Lawlor DA, Harbord RM, et al. Using multiple genetic variants as instrumental variables for modifiable risk factors. Stat Methods Med Res. 2012;21(3):223–242. doi:10.1177/0962280210394459
25. Hunt TK, Aslam RS, Beckert S, et al. Aerobically derived lactate stimulates revascularization and tissue repair via redox mechanisms. Antioxid Redox Signal. 2007;9(8):1115–1124. doi:10.1089/ars.2007.1674
26. Yang L, Gao L, Nickel T, et al. Lactate promotes synthetic phenotype in vascular smooth muscle cells. Circ Res. 2017;121(11):1251–1262. doi:10.1161/CIRCRESAHA.117.311819
27. Chen J, Zhang M, Liu Y, et al. Histone lactylation driven by mROS-mediated glycolytic shift promotes hypoxic pulmonary hypertension. J Mol Cell Biol. 2023;14(12). doi:10.1093/jmcb/mjac073
28. Shantha GP, Wasserman B, Astor BC, et al. Association of blood lactate with carotid atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) Carotid MRI Study. Atherosclerosis. 2013;228(1):249–255. doi:10.1016/j.atherosclerosis.2013.02.014
29. Januszek R, Mika P, Nowobilski R, Maga P, Nizankowski R. The improvement of walking abilities and endothelial function after the supervised training treadmill program (STTP) in patients with peripheral artery disease (PAD) is not related to prostacyclin and thromboxane release. Int J Cardiol. 2016;222:813–818. doi:10.1016/j.ijcard.2016.07.274
30. Adamo L, Nassif ME, Novak E, LaRue SJ, Mann DL. Prevalence of lactic acidaemia in patients with advanced heart failure and depressed cardiac output. Eur J Heart Fail. 2017;19(8):1027–1033. doi:10.1002/ejhf.628
31. Davierwala PM, Leontyev S, Verevkin A, et al. Temporal trends in predictors of early and late mortality after emergency coronary artery bypass grafting for cardiogenic shock complicating acute myocardial infarction. Circulation. 2016;134(17):1224–1237. doi:10.1161/CIRCULATIONAHA.115.021092
32. Gjesdal G, Braun OO, Smith JG, Schersten F, Tyden P. Blood lactate is a predictor of short-term mortality in patients with myocardial infarction complicated by heart failure but without cardiogenic shock. BMC Cardiovasc Disord. 2018;18(1):8. doi:10.1186/s12872-018-0744-1
33. Wang N, Wang W, Wang X, et al. Histone lactylation boosts reparative gene activation post-myocardial infarction. Circ Res. 2022;131(11):893–908. doi:10.1161/CIRCRESAHA.122.320488
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Mendelian Randomization Analysis Supports a Causal Relationship Between Circulating Inflammatory Proteins and Basal Cell Carcinoma
Fu ZD, Wang Y, Yan HL, Wu JH
Clinical, Cosmetic and Investigational Dermatology 2025, 18:767-779
Published Date: 31 March 2025



