Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Comparative Sedative Effects of Esketamine and Dexmedetomidine Versus Dexmedetomidine Alone in Patients Undergoing Spinal Tumor Surgery
Authors Lin C, Yuan L, Shi J, Kong L , Luo N, Wang J
Received 20 February 2025
Accepted for publication 17 May 2025
Published 23 May 2025 Volume 2025:21 Pages 747—755
DOI https://doi.org/10.2147/TCRM.S515869
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Chuanyan Lin, Liyong Yuan, Jun Shi, Lingsi Kong, Ni Luo, Jianlin Wang
Department of Anesthesiology, Ningbo Sixth Hospital, Ningbo City, Zhejiang Province, 315140, People’s Republic of China
Correspondence: Jianlin Wang, Department of Anesthesiology, Ningbo Sixth Hospital, 1059 Zhongshan East Road, Yinzhou District, Ningbo City, Zhejiang Province, 315140, People’s Republic of China, Tel +86 0574-87990640, Email [email protected]
Objective: Esketamine and dexmedetomidine are commonly used sedatives in surgery, which can result in minimal respiratory depression and analgesic activity. This study investigated the sedative effect of esketamine combined with dexmedetomidine on patients undergoing spinal tumor (ST) surgery.
Methods: We did a retrospective analysis at the Anesthesiology Department of Ningbo City’s the sixth Hospital. They studied 75 ST surgery patients who got esketamine in combination with dexmedetomidine (Group ED) between April 2022 and June 2024. In a 1:1 cohort, compare these individuals to those who only received dexmedetomidine at the same time period (Group D). The primary outcome is perioperative hemodynamic status. The secondary outcomes were pain intensity, intraoperative neurophysiological monitoring (IONM), and the occurrence of adverse responses.
Results: Compared with group E, the group ED had lower mean arterial pressure (MAP), heart rate (HR), and visual-analogue scale (VAS) scores after the start of surgery (all P< 0.05). There was no significant difference in the waiting time for perioperative motor evoked potential (MEP) and the intensity of the first induced MEP current between the two groups (all P> 0.05); The Group ED first induced MEP amplitude, somatosensory evoked potential (SEP) amplitude, and MEP amplitude greater than the Group D, while SEP latency and MEP latency were smaller than the Group D (all P< 0.05). There was no significant difference in the incidence of perioperative adverse events between the two groups (P> 0.05).
Conclusion: Compared with dexmedetomidine alone, the combination of esketamine and dexmedetomidine during ST surgery can demonstrated superior sedation and pain control without increasing adverse event risk, making it a viable alternative for ST surgery anesthesia.
Keywords: esketamine, dexmedetomidine, spinal tumor, sedative effect
Introduction
In recent years, affected by many factors such as the aging of the population and the formation of bad living habits, the incidence rate of malignant tumors has continued to increase.1 As a clinical multiple malignant tumor type, the incidence rate of spinal tumor (ST) also increases.2 STs pose a great threat to the physical and mental health as well as the quality of life of patients, therefore, early implementation of safe and effective treatment is necessary.2,3 Surgery is an important measure for clinical treatment of ST.2–4 But ST surgery is more complex, with a large number of sensitive nerves distributed in the joint capsule and periosteum, which can easily cause severe pain due to invasive surgical procedures. This can easily cause inflammatory stress reactions and hemodynamic fluctuations, which is not conducive to the smooth progress of surgery.3–5
Effective anesthesia management during ST surgery plays an important role in improving the effectiveness and safety of surgical treatment.5,6 As is well known, the spine’s special position and intricate functions make spinal surgery challenging and increase the risk of serious bodily trauma. Additionally, once the effects of postoperative anesthesia medications wear off, the pain becomes worse, which negatively impacts the recovery process following surgery. Dexmedetomidine is a general anesthesia drug that is an alpha 2 receptor agonist. It has hypnotic, analgesic, and sedative effects, can alleviate pain, and has little impact on respiratory function.7,8 Esketamine is a new type of anesthetic drug, which is the dextrorotatory form of esketamine. It has a strong affinity with N-methyl-D-aspartate (NMDA) receptors, which can reduce adverse cardiovascular reactions and alleviate discomfort.9,10 At present, relevant evidence has shown the sedative effect of esketamine combined with dexmedetomidine in orthopedic and thoracic surgery.10,11 Zhang et al discovered in 2023 that people with chronic pain after scoliosis correction surgery experienced considerably better analgesia and subjective sleep quality when the mini-dose esketamine–dexmedetomidine combination was given to sufentanil PCIA, without seeing an increase in adverse effects.10 However, its sedative effect in specific populations undergoing ST surgery has not been confirmed. The aim of this study is to investigate whether the combination of esketamine and dexmedetomidine can further improve the perioperative sedative effect in patients undergoing ST surgery.
Materials And Methods
Research Design and Participants
This study is a retrospective study conducted in the Anesthesiology Department of the Sixth Hospital of Ningbo City. They included a cohort of 75 ST surgery patients who received esketamine combined with dexmedetomidine (Group ED) from April 2022 to June 2024. Match these patients with patients who received dexmedetomidine alone during the same period (Group E) in a 1:1 cohort.
Inclusion Criteria
-Meets the diagnostic criteria for ST;1
-Accept surgical treatment;
-ASA classification falls between I–II;
-Complete clinical data.
Exclusion Criteria
-Electrolyte disorders (such as hypokalemia and hypocalcemia);
-Individuals with coagulation dysfunction;
-Having serious cardiovascular, lung, kidney, or liver diseases;
-Serious respiratory or circulatory system diseases;
-Pregnant or lactating women;
-Long term use of analgesics and sedatives;
-Preoperative bradycardia.
Sedation Protocol
Group D
Dexmedetomidine alone was used (China National Pharmaceutical Group Industrial Langfang Branch, China). Intravenous injection of sufentanil (Yichang Renfu Pharmaceutical Co., Ltd., China) at a dose of 5 μg/kg for anesthesia induction; Administer ropivacaine (0.375%) (AstraZeneca AB, Sweden) for local infiltration anesthesia; Intraoperative infusion of dexmedetomidine 0.5 μg/(kg h) was administered to maintain sedation.
Group ED
The combination of esketamine (Jiangsu Hengrui Pharmaceutical Co., Ltd., China) and dexmedetomidine was administered. Intravenous injection of 0.25 mg/kg esketamine for anesthesia induction; The rest of the operations are the same as Group D.
Outcome
Main outcome
The main outcome of this study is the intraoperative hemodynamic status. Mean arterial pressure (MAP) and heart rate (HR) were measured at preoperatively (T0), before skin incision (T1), 30 minutes during surgery (T2), and immediately after closure (T3). The multifunctional monitoring device (B40I; GE Healthcare Finland Oy; USA) recorded MAP and HR at different time points.
Secondary Outcomes
Visual Analog Scale (VAS) was used to assess the degree of pain before surgery, at 6, 12, 24, and 48 hours after surgery; A total of 10 points, the higher the score, the stronger the pain. Record the waiting time, current intensity, amplitude, somatosensory evoked potential (SEP) amplitude, SEP latency, MEP amplitude, and MEP latency of the first motor evoked potential (MEP) during surgery (using the Nicolet Endeavor intraoperative neurophysiological monitoring system from the United States). Sedative adverse events include tachycardia, respiratory depression, hypertension, and postoperative nausea and vomiting (PONV). Surgical related adverse events include pneumothorax, asphyxia and cough, pulmonary hemorrhage, chest pain, heat absorption, and pulmonary infection.
Statistical Analysis
Statistical software SPSS 26.0 (IBM SPSS Inc., Armonk, United States) and GraphPad Prism 8.0 were used for data processing. Use Shapiro Wilk test to evaluate normal distribution. The continuous data of normal distribution and the data of non normal distribution are represented as mean ± standard deviation (SD) and median (interquartile range), respectively. Classification data is represented as frequency and percentage. Use independent sample t-test to evaluate continuous data with normal distribution, such as age and body mass index (BMI). Mann–Whitney U-test is used for data with non normal distribution. Chi square test is used for classifying data. P<0.05 is considered statistically significant.
Results
Selection and Basic Characteristics of Participants
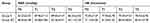
This study included a total of 150 patients, including 94 males and 56 females; Age range: 39–78 years old, 59.2 ± 8.1 years old; 75 patients in the Group ED were matched with the E group in a 1:1 ratio (Figure 1). There were no significant differences in age, gender, tumor type, BMI, American Society of Anesthesiologists (ASA) grading, and surgical site between the two groups of patients (all P>0.05) (Table 1).
 |
Table 1 Comparison of Basic Characteristics Between Two Groups |
 |
Figure 1 Patient flowchart. |
Hemodynamic State
At T0, there was no significant difference in MAP and HR levels between the two groups (all P>0.05); At T1, T2, and T3, the MAP and HR of the Group ED were significantly lower than those of the Group D (all P<0.05) (Figure 2 and Table 2).
 |
Pain Level
Before surgery, there was no significant difference in VAS scores between the two groups (P>0.05); At 6, 12, 24, and 48 hours postoperatively, the VAS scores in the Group ED were significantly lower than those in the Group D (all P<0.05) (Figure 3 and Table 3).
 |
Table 3 Comparison of VAS Scores at Different Time Points Between the Two Groups |
 |
Figure 3 VAS score curve. Comparing two groups, *P<0.05. Abbreviations: ED, esketamine combined with dexmedetomidine; D, dexmedetomidine; VAS, visual-analogue scale. |
Ionm
There was no significant difference in the waiting time and current intensity for the first induction of MEP between the two groups (all P>0.05); The Group ED first induced MEP amplitude (1554±178), SEP amplitude (1.85±0.24), and MEP amplitude (1597±17) were greater than those inMEP amplitude (1488±173), SEP amplitude (1.73±0.29), and MEP amplitude (1514±230) of the Group D, while the SEP latency (18.3±2.9) and MEP latency (21(18–23)) were lower than those in SEP latency (20.7±3) and MEP latency (23 (20–25)) of the Group D (all P<0.05) (Table 4).
 |
Table 4 Comparison of IONM Between Two Groups |
Perioperative Adverse Events
The incidence of sedation-related adverse events in this study was 20.67% (31/150); Among them, the incidence rate of Group ED was 16.00% (12/75), and the incidence rate of Group D was 25.33% (19/75), with no significant difference between the two groups (P>0.05). The incidence of surgery related adverse events was 22.67% (34/150); Among them, the incidence rate of Group ED was 18.67% (14/75), and the incidence rate of Group D was 20.67% (20/75); There was no significant difference between the two groups (P>0.05) (Table 5).
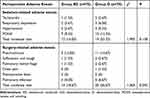 |
Table 5 Incidence of Adverse Reactions in Two Groups, n (%) |
Discussion
The results of this study indicate that the combination of esketamine and dexmedetomidine is more effective in inhibiting hemodynamic status and reducing postoperative pain in ST surgery compared to using dexmedetomidine alone; It has little effect on MEP and SEP, and does not increase the incidence of adverse events.
Surgery is an important treatment for ST.3–5,12 Zheng et al12 found that the spine has a unique position and complex functions, which makes spinal surgery difficult and can easily cause significant trauma to the body; And after the efficacy of postoperative anesthesia drugs subsides, the pain is stronger, which has an adverse effect on postoperative recovery. Therefore, anesthesia management for spinal surgery should be strengthened.5–10,12 Dexmedetomidine is a commonly used analgesic drug for ST surgery.7,8,13 Wu et al13 found that dexmedetomidine can block the sympathetic nervous system, inhibit sympathetic nerve activity, and thus exert stress relief and sedative effects. Esketamine is also a commonly used anesthetic in clinical practice.9,10 It has both analgesic and sedative effects. Compared to esketamine, its potency is stronger, and its site of action is similar to esketamine; But its affinity with N-methyl-D-aspartate is about twice that of esketamine.9,10,14
Based on the above background, some clinical studies attempt to use dexmedetomidine combined with esketamine for spinal surgery treatment.10,15 Zhang et al10 applied dexmedetomidine and esketamine in scoliosis correction surgery, and the results showed that a combination intervention of low-dose esketamine and dexmedetomidine could effectively improve postoperative analgesia and subjective sleep quality. The results of this study also showed that the VAS scores of the Group ED were lower than those of the Group D at different time points after surgery, which is consistent with the research results of the aforementioned scholars. This confirms that the combined anesthesia regimen of dexmedetomidine and esketamine can help alleviate postoperative pain in patients undergoing ST surgery. Mainly due to the sedative, analgesic, anti anxiety, and stress reducing effects of dexmedetomidine.7,8,15 It can reduce pain by acting on alpha 2 receptors in the central nervous system, downregulating sympathetic nervous activity. Esketamine acts on NMDA receptors and opioid receptors, inhibiting the transmission of pain signals and thereby reducing pain.9,10,14–16 The combination of the two can play a role in different pain transmission pathways and mechanisms, enhancing the analgesic effect. Lu et al16 applied a combined anesthesia regimen of dexmedetomidine and esketamine in lung cancer surgery patients, and the results showed that the VAS scores of patients were lower than those who only received sufentanil. This is consistent with the conclusion of this study.
Hemodynamic stability is an important prerequisite for ensuring the effectiveness and safety of surgical treatment. The results of this study showed that the MAP and HR of the Group ED were significantly lower than those of the Group D during surgery. This confirms that the combination of dexmedetomidine and esketamine can also help suppress intraoperative blood pressure and heart rate fluctuations in patients undergoing ST surgery, and maintain hemodynamic stability. This is consistent with the research results of Lin et al11 and Liu et al.17 The main reason for this is that esketamine and dexmedetomidine can act on the sympathetic nervous system, reducing the activity of the sympathetic nervous system, thereby reducing the release of catecholamines in children, lowering blood pressure and heart rate.11,17,18
In addition, there is a risk of new neurological deficits during the postoperative period of ST surgery. Therefore, intraoperative neurophysiological monitoring and mapping (IONM) is highly necessary.19,20 Li et al21 found that SEP refers to the electrical activity recorded by sensory nerve fibers that stimulate the skin or peripheral nerves in the corresponding sensory transmission pathways/cortical sensory projection areas on the scalp; MEP is the electrical/magnetic stimulation of the brain motor area/efferent pathway, which records the electrical response of the efferent pathway/muscle at the stimulation point. Both play an important role in the evaluation of anesthesia status. The results of this study showed that the Group ED first induced MEP amplitude, SEP amplitude, and MEP amplitude greater than the Group D, while the SEP latency and MEP latency were significantly lower than the Group D. This indicates that the combined anesthesia regimen of esketamine and dexmedetomidine can also reduce the impact on MEP and SEP, ensuring the effectiveness of anesthesia.19–21
Various adverse events often occur during the perioperative period.22 This study observed sedation related adverse events and surgery related adverse events separately. Among them, vomiting and nausea were the main sedation related adverse events, with an incidence rate of 11.33% (17/150), followed by hypertension (4.0%, 6/150) and respiratory depression (3.33%, 5/150). Opioids are a key trigger factor for PONV, and there is evidence to suggest that intravenous injection of dexmedetomidine or esketamine can reduce the need for opioid drugs during surgery.19–22 Pneumothorax is the main surgical related adverse event, with an incidence rate of 13.33% (20/150), followed by pulmonary infection (5.33%, 8/150). Stable MAP and HR are more beneficial for elderly patients with lower heart rates or more fragile cardiovascular systems.22,23 However, regardless of whether it was sedation or surgery related adverse events, although the incidence rate was lower in the Group ED, there was no statistically significant difference between the two groups. Additionally, we found no discernible difference between the two groups in terms of side effects associated with either dexmedetomidine (such as bradycardia and hypotension) or esketamine (such as mental symptoms). No psychological signs appeared in any of our individuals. This is inconsistent with previous research results, and we believe this may be due to the nature of the study and the small sample size. As a result, this patient population can safely employ our dosage schedule. However, this result is unique to this study, and further patient data is required to validate it.
This study has the following obvious shortcomings. Firstly, this is a retrospective analysis conducted at a tertiary center, and only a sample size of 150 was matched. Secondly, we only evaluated pain scores within the first 48 hours after surgery, which does not reflect long-term outcomes; Postoperative chronic pain can affect patient satisfaction and quality of life. Thirdly, we only used a single dose of esketamine and dexmedetomidine, which may not be the most appropriate dosage. The findings of this study should be supported by future research, including more centers and broader patient participation.
Conclusion
The combination of esketamine and dexmedetomidine during ST surgery can suppress hemodynamic status, reduce postoperative pain, have minimal impact on MEP and SEP, and do not increase the risk of adverse events. Esketamine may still have certain drawbacks when used in surgery, though, thus further research is required to support this study in subsequent investigations.
Abbreviations
E, Esketamine; ED, Esketamine and dexmedetomidine; ST, spinal tumor; IONM, intraoperative neurophysiological monitoring; MAP, mean arterial pressure; HR, heart rate; VAS, visual-analogue scale; MEP, motor evoked potential; SEP, somatosensory evoked potential; PONV, postoperative nausea and vomiting; SD, standard deviation; BMI, body mass index.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The ethics committee of Ningbo Sixth Hospital approved this study with the number L2021075, Date: November 15th 2021. All procedures involving human subjects adhered to the 1964 Declaration of Helsinki and its subsequent amendments or equivalent ethical standards. Given the retrospective nature of the study, informed consent was waived by the Ethical Committee of Ningbo Sixth Hospital. All data were stored securely, and confidentiality was maintained throughout the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Xu Y, Shi F, Zhang Y, et al. Twenty-year outcome of prevalence, incidence, mortality and survival rate in patients with malignant bone tumors. Int J Cancer. 2024;154(2):226–240. doi:10.1002/ijc.34694
2. Liu Z, Li X, Lu J. Application evaluation of mixed-reality holographic imaging technology in the surgical treatment of spinal cord glioma. Pak J Med Sci. 2022;38(7):1958–1963. doi:10.12669/pjms.38.7.4777
3. Nadeem SF, Khan AA, Shamim MS. Role of Proton Beam Therapy in Spinal Chordomas: a Narrative Review of The Literature. J Pak Med Assoc. 2024;74(9):1718–1720. doi:10.47391/JPMA.24-72
4. Lamperti M, Tufegdzic B, Avitsian R. Management of complex spine surgery. Curr Opin Anaesthesiol. 2017;30(5):551–556. doi:10.1097/ACO.0000000000000494
5. Li X, Liu ZJ, Liang L, Dong HQ. Application evaluation of intraoperative ultrasound combined with neuro electrophysiological detection in the spinal cord glioma surgery. Pak J Med Sci. 2021;37(3):879–884. doi:10.12669/pjms.37.3.3638
6. Tariq A, Sohail A, Shah Z, Bakhshi S, Shamim MS. Spinal meningiomas: management and outcomes. J Pak Med Assoc. 2023;73(7):1548–1550. doi:10.47391/JPMA.23-52
7. Huda AU, Yasir M, Mughal MZ, Arif A. Effect of Intravenous Dexmedetomidine Before Extubation on Emergence Delirium after Nasal Surgeries. J Coll Physicians Surg Pak. 2024;34(5):509–513. doi:10.29271/jcpsp.2024.05.509
8. Keating GM. Dexmedetomidine: a Review of Its Use for Sedation in the Intensive Care Setting. Drugs. 2015;75(10):1119–1130. doi:10.1007/s40265-015-0419-5
9. Mion G, Himmelseher S. Esketamine: less Drowsiness, More Analgesia. Anesth Analg. 2024;139(1):78–91. doi:10.1213/ANE.0000000000006851
10. Zhang Y, Cui F, Ma JH, Wang DX. Mini-dose esketamine-dexmedetomidine combination to supplement analgesia for patients after scoliosis correction surgery: a double-blind randomised trial. Br J Anaesth. 2023;131(2):385–396. doi:10.1016/j.bja.2023.05.001
11. Lin Z, Li S, Zhou Y, et al. A comparative study of esketamine-dexmedetomidine and sufentanil-dexmedetomidine for sedation and analgesia in lung tumor percutaneous radiofrequency ablation (PRFA): a randomized double-blind clinical trial. BMC Anesthesiol. 2023;23(1):304. doi:10.1186/s12871-023-02266-y
12. Zheng H, Zhang P, Shi S, Zhang X, Cai Q, Gong X. Sub-anesthetic dose of esketamine decreases postoperative opioid self-administration after spine surgery: a retrospective cohort analysis. Sci Rep. 2024;14(1):3909. doi:10.1038/s41598-024-54617-5
13. Wu J, Ku SC, Ko AL. Use of Dexmedetomidine for Postoperative Pain Management Following Spine Fusion Surgery in a Highly Opioid-Tolerant Patient. J Pain Palliat Care. Pharmacother. 2019;33(1––2):49–53. doi:10.1080/15360288.2019.1651439
14. Feeney A, Papakostas GI. Pharmacotherapy: ketamine and Esketamine. Psychiatr Clin North Am. 2023;46(2):277–290. doi:10.1016/j.psc.2023.02.003
15. Zhou JS, Chen Z, Liu YY, et al. Observation on the Analgesic Effect of Different Doses of a Combination of Esketamine and Dexmedetomidine Administered for Percutaneous Endoscopic Transforaminal Discectomy: a Randomized, Double-Blind Controlled Trial. CNS Drugs. 2024;38(7):547–558. doi:10.1007/s40263-024-01083-2
16. Lu Y, Yin G, Jin C, et al. The Application Value of Esketamine and Dexmedetomidine in Preventing Postoperative Delirium and Hyperalgesia in Elderly Patients with Thoracic Anesthesia. Altern Ther Health Med. 2024;30(3):80–85.
17. Liu C, Zhang T, Cao L, Lin W. Comparison of esketamine versus dexmedetomidine for attenuation of cardiovascular stress response to double-lumen tracheal tube intubation: a randomized controlled trial. Front Cardiovasc Med. 2023;10:1289841. doi:10.3389/fcvm.2023.1289841
18. Zhang W, You J, Hu J, et al. Effect of esketamine combined with dexmedetomidine on delirium in sedation for mechanically ventilated ICU patients: protocol for a nested substudy within a randomized controlled trial. Trials. 2024;25(1):431. doi:10.1186/s13063-024-08287-3
19. Liu K, Ma C, Li D, et al. The role of intraoperative neurophysiological monitoring in intramedullary spinal cord tumor surgery. Chin Neurosurg J. 2023;9(1):33. doi:10.1186/s41016-023-00348-x
20. Scibilia A, Terranova C, Rizzo V, et al. Intraoperative neurophysiological mapping and monitoring in spinal tumor surgery: sirens or indispensable tools? Neurosurg Focus. 2016;41(2):E18. doi:10.3171/2016.5.FOCUS16141
21. Li Y, Meng L, Peng Y, et al. Effects of Dexmedetomidine on motor- and somatosensory-evoked potentials in patients with thoracic spinal cord tumor: a randomized controlled trial. BMC Anesthesiol. 2016;16(1):51. doi:10.1186/s12871-016-0217-y
22. Ryvlin J, Javed K, la Garza Ramos R, et al. Is perioperative blood transfusion associated with postoperative thromboembolism or infection after metastatic spinal tumor surgery? Clin Neurol Neurosurg. 2023;235:108052. doi:10.1016/j.clineuro.2023.108052
23. Ji N, Zhang Y, Li L, Du J, Tan S, Liu F. Comparison of Recovery Effect for Sufentanil vs. Remifentanil Anesthesia in Elderly Patients Undergoing Curative Resection for Hepatocellular Carcinoma. Pain Ther. 2023;12(4):1017–1025. doi:10.1007/s40122-023-00522-0
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Effect of Dexmedetomidine and Two Different Doses of Esketamine Combined Infusion on the Quality of Recovery in Patients Undergoing Modified Radical Mastectomy for Breast Cancer - A Randomised Controlled Study
Huang Z, Liu N, Hu S, Ju X, Xu S, Wang S
Drug Design, Development and Therapy 2023, 17:2613-2621
Published Date: 28 August 2023
Opioid-Free Anesthesia for Pain Relief After Laparoscopic Cholecystectomy: A Prospective Randomized Controlled Trial
Yu JM, Tao QY, He Y, Liu D, Niu JY, Zhang Y
Journal of Pain Research 2023, 16:3625-3632
Published Date: 30 October 2023
Intranasal Dexmedetomidine-Esketamine Combination Premedication versus Monotherapy for Reducing Emergence Delirium and Postoperative Behavioral Changes in Pediatric Tonsillectomy and/or Adenoidectomy: A Randomized Controlled Trial

Liao Y, Xie S, Zhuo Y, Chen S, Luo Y, Wei Y, Yao Y
Drug Design, Development and Therapy 2024, 18:4693-4703
Published Date: 23 October 2024
Effects of Esketamine Combined with Dexmedetomidine on Early Postoperative Cognitive Function in Elderly Patients Undergoing Lumbar Spinal Surgery: A Double-Blind Randomized Controlled Clinical Trial
Tao QY, Liu D, Wang SJ, Wang X, Ouyang RN, Niu JY, Ning R, Yu JM
Drug Design, Development and Therapy 2024, 18:5461-5472
Published Date: 27 November 2024
The Effects of Opioid-Free Anesthesia with Dexmedetomidine and Esketamine on Postoperative Anesthetic-Related Complications for Hip Surgery in the Elderly
Ye Q, Hu Y, Xing Q, Wu Y, Zhang Y
International Journal of General Medicine 2024, 17:6291-6302
Published Date: 17 December 2024




