Back to Journals » Advances in Medical Education and Practice » Volume 16
Comparative Study of Problem-Based Learning and Traditional Teaching Methods on Medical Students’ Outcomes in Pediatrics Clerkships
Authors Ba H, Xu L , Gu Y, Li Y, Jiang X, Li X, Li S
Received 3 January 2025
Accepted for publication 10 April 2025
Published 16 April 2025 Volume 2025:16 Pages 615—624
DOI https://doi.org/10.2147/AMEP.S515527
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Hongjun Ba,* Lingling Xu,* Yufen Gu, Yijuan Li, Xiaoyun Jiang, Xiaoyu Li, Shujuan Li
Department of Pediatrics, First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoyu Li, Email [email protected] Shujuan Li, Email [email protected]
Background: Problem-Based Learning (PBL) is an engaging, student-centered teaching approach that has become increasingly popular in the field of medical education. Particularly during clinical rotations, PBL is thought to enhance students’ clinical reasoning and skills. However, the impact of PBL in pediatric clerkships has not been fully explored.
Objective: This study aimed to assess the influence of PBL on the clinical skills of medical interns during pediatric rotations, comparing the outcomes between PBL and traditional teaching methods.
Methods: A randomized controlled trial was conducted with 72 medical interns (38 male, 34 female) participating in pediatric rotations at our hospital between November 2023 and September 2024. The interns were assigned at random to either the PBL group (36 students) or the traditional teaching group (36 students), with stratification based on baseline clinical examination scores. Both groups participated in a two-week pediatric internship, encountering identical clinical cases. The PBL group received instruction supplemented with PBL, while the traditional group received bedside teaching. The outcomes were evaluated using a theoretical knowledge exam, Mini-CEX assessments, and a PBL group satisfaction survey.
Results: The results of the theoretical knowledge exam showed no significant difference between the groups (PBL group: 90.25 ± 2.15, traditional group: 89.78 ± 2.14, p > 0.05), indicating similar support for theoretical learning. Mini-CEX evaluations demonstrated that the PBL group showed significant improvements in history taking, medical decision-making, physician-patient interactions, and comprehensive clinical skills compared to the traditional group. Feedback from the PBL group was overwhelmingly positive, with students highlighting significant improvements in clinical reasoning and diagnostic skills.
Conclusion: PBL significantly enhanced clinical skills in pediatric clerkships, particularly in clinical reasoning, diagnosis, and communication. Although both teaching methods supported theoretical learning equally, PBL fostered greater student engagement and deeper learning, suggesting that it could be a valuable model for future medical education.
Keywords: pediatrics, teaching methods, problem-based learning, clinical clerkship
Introduction
Pediatrics is a multidisciplinary field that integrates knowledge from various areas, including physiology, diagnostics, anatomy, pathophysiology, and other specialties.1 Pediatric diseases often present with varied and rapidly evolving symptoms, posing unique challenges for both practitioners and learners. Due to the young age of pediatric patients, who may have difficulty communicating their symptoms effectively, healthcare providers often rely on family-provided histories, introducing complexities in diagnosis and management. This reliance on indirect communication can make pediatric medicine particularly challenging for medical students, especially when they encounter these complexities for the first time during clinical clerkships. Without effective teaching methods, students may experience a decline in motivation and engagement in this crucial field of medicine.
Traditional lecture-based teaching methods, while effective in delivering foundational knowledge, tend to be passive, often failing to actively engage students in the development of critical thinking and clinical reasoning skills.2 This approach may also struggle to connect theoretical knowledge to practical application in clinical settings, leading to suboptimal preparation for real-world scenarios. As a result, students may not develop the independent problem-solving skills necessary for successful medical practice, especially in fields like pediatrics, where clinical decisions often need to be made rapidly and under uncertainty.
In contrast, PBL offers a more active, student-centered approach that has been shown to improve student engagement, critical thinking, and the application of knowledge in clinical settings.3,4 PBL involves presenting students with real-world problems that require them to work collaboratively to find solutions, promoting not only knowledge acquisition but also essential skills such as self-directed learning, communication, and teamwork. Research has demonstrated that PBL can bridge the gap between theory and practice, particularly in clinical fields like pediatrics, where practical, hands-on problem-solving is essential for effective patient care.4 Furthermore, PBL has been shown to enhance students’ abilities to synthesize complex information and make informed decisions in clinical contexts.
However, while PBL offers several advantages, it is not without its challenges. It can be time-consuming for both students and instructors and requires careful design to ensure that problems are appropriately challenging yet manageable. Additionally, the effectiveness of PBL is contingent on factors such as the design of the curriculum, the readiness of students, and the facilitation skills of instructors.5 Despite these challenges, a growing body of literature supports the use of PBL in medical education, particularly in clinical environments like pediatrics.6,7
The current study builds on this body of evidence by exploring the impact of PBL in pediatrics clerkships. While the integration of PBL into basic medical education has been widely studied,2,3 its application in pediatrics clerkships remains underexplored. This study aims to investigate the effectiveness of PBL in improving medical students’ clinical outcomes during pediatric rotations. Specifically, the study evaluates the use of the Maastricht model of PBL, which emphasizes collaborative problem-solving and self-directed learning.8 This model was chosen for its focus on clinical reasoning and its structured approach to problem analysis, which aligns well with the goals of pediatric clerkships.
The study involves 72 undergraduate medical students who participated in pediatrics clerkships at our institution between November 2023 and September 2024. The research will assess the comparative outcomes of students exposed to traditional teaching methods versus those who engaged in PBL-based learning.
Objectives and Methods
Study Participants
This study involved a selection of undergraduate clinical medical interns who participated in pediatrics rotations at our hospital between November 2023 and September 2024. This study assessed how PBL influences the clinical skills of 72 medical interns participating in a five-year program at Sun Yat-sen University. The participants, comprising 38 male and 34 female students, were randomly divided into four groups according to their practicum rotation, utilizing a computer-generated randomization list. Each cohort, consisting of 3 to 4 students, was assigned to either the PBL or conventional teaching approach during a two-week pediatric internship. To ensure comparability between the groups, randomization was stratified based on their initial clinical examination scores.
Methods
Study Design
This study utilized a controlled, exploratory trial design, featuring blinded assessment methods. The interns were allocated at random to either the PBL group, consisting of 36 students, or the traditional group, also comprising 36 students. There were no substantial differences between the groups in terms of gender, age, or initial clinical evaluation scores (p > 0.05). The PBL group engaged in instruction enhanced by PBL, while the traditional group experienced conventional bedside instruction, as illustrated in Figure 1. Both groups worked on the same clinical case scenarios related to common pediatric conditions, including urinary tract infection, diarrhea, congenital heart disease, pneumonia, and encephalitis. Each intern had the same opportunity to access identical learning materials, trainers, and course intensity. The primary textbook used was the 9th edition of “Pediatrics” published by the People’s Healthcare Publishing company. Ethical authorization was granted by the ethics committee, and knowledgeable consent was obtained, with particular attention given to privacy considerations due to the use of data from child patients.
 |
Figure 1 Study framework and flow diagram. |
Teaching Implementation
Traditional Teaching Group
In the control group, traditional teaching methodologies were employed. This involved a preliminary selection of representative pediatrics cases by the instructors, followed by securing consent from the patients’ families. Prior to the commencement of the clinical internship, instructors escorted the students to the bedside of these pre-selected cases. Here, under the guidance of their instructors, students engaged in the collection of medical histories and the conduction of physical examinations. They also analyzed pertinent laboratory findings and interpreted radiological data related to their cases. This hands-on experience was complemented by a structured debriefing session, where students summarized their cases and discussed them with the instructors. The session culminated in a comprehensive review, led by the instructors, which focused on reinforcing the key theoretical concepts and knowledge that underpinned each clinical case.
PBL Group
The PBL approach in the experimental group was structured according to the 7-step Maastricht model, developed following a thorough review of relevant literature6,7 The PBL process in this study adhered to the following seven steps (Figure 2):
 |
Figure 2 PBL process and flow chart. |
1. Problem Presentation: At the beginning of each PBL session, the instructor presented a clinical problem relevant to the pediatric syllabus, such as community-acquired pneumonia, diarrhea, congenital heart disease, malnutrition, and acute nephritis. Each problem was selected based on its representativeness and relevance to common pediatric conditions that medical students must master during their internship. The problem was designed to challenge students’ existing knowledge and stimulate inquiry. Students were provided with an initial patient history prior to class to familiarize themselves with the case and to prepare for the analysis.
2. Analysis and Learning Objectives: Students were asked to break down the clinical problem and identify key issues, such as the main complaints, underlying mechanisms, and potential diagnoses. In this phase, students collaboratively formulated learning objectives, which guided their self-directed learning. The instructor facilitated this process, helping students develop a clear understanding of the clinical questions that needed to be addressed. This step ensured that the learning was focused and aligned with the curriculum.
3. Self-Directed Learning: In the self-directed learning phase, students independently researched the relevant medical literature, textbooks, and online resources to gather information related to the case. Each student was responsible for acquiring the knowledge needed to address the learning objectives set in the previous step. They were encouraged to explore the underlying pathophysiology, diagnostic procedures, treatment options, and potential complications associated with the case. The instructor provided support and guidance as needed but did not dictate the direction of students’ learning. This phase encouraged critical thinking and independent problem-solving.
4. Group Discussion: After completing their individual research, students gathered in small groups (3–4 members per group) to discuss the case and share their findings. During this group discussion, students collaborated to refine their understanding of the clinical problem, critically evaluate their learning, and discuss alternative hypotheses. The instructor facilitated the discussion, guiding students to clarify complex concepts, question assumptions, and integrate their findings into a comprehensive understanding of the case. This collaborative approach allowed students to learn from one another and develop communication and teamwork skills.
5. Integration and Theory Application: Following the group discussion, students worked together to integrate the theoretical knowledge they had acquired and apply it to the clinical scenario. They collectively formulated a management plan, which included diagnosis, treatment, and preventive measures. In this phase, students demonstrated their ability to translate theoretical knowledge into practical clinical decision-making. The instructor played a key role in ensuring that the integrated solution was evidence-based and aligned with current pediatric practices.
6. Summary and Reflection: At the end of each session, the instructor summarized the key learning points and clarified any unresolved issues. Students were encouraged to reflect on their learning process, discuss what went well, and identify areas for improvement. This reflection helped consolidate their understanding and provided insights into their own learning strategies. The instructor used this opportunity to reinforce critical concepts and offer additional resources for further study.
7. Feedback and Evaluation: The instructor provided constructive feedback on both the group discussions and individual contributions. This feedback focused on students’ critical thinking, problem-solving skills, teamwork, and understanding of the case. In addition, students received individual assessments based on their participation, presentation, and the quality of their proposed solutions. The feedback session also included a peer review component, allowing students to evaluate each other’s performance and offer suggestions for improvement. This process helped students refine their learning and foster a growth mindset.
Assessment Methods
The Interns’ Performance After Rotation Was Evaluated Using Three Evaluation Instruments
Theory Examination
The theory exam was designed based on the requirements of the pediatric curriculum, while also considering the diseases covered in the clinical rotation. It included both multiple-choice and short-answer questions. The exam assessed students’ theoretical understanding of pediatric diseases. The grading scale is as follows: A: ≥90; B: 80–89; C: 70–79; D: 60–69; F: <60.
Mini-CEX Assessment
The Mini-CEX, a well-acknowledged tool for evaluating clinical skills,9,10 was used to assess practical competencies. Students took medical histories from young patients’ guardians and conducted physical exams on young children, under instructor supervision. The Mini-CEX assessed students across seven criteria, using a nine-point scale:
History Taking: Accuracy in gathering patient history, responding to non-verbal cues, and demonstrating empathy.
Physical Examination: Competence in conducting exams in an organized manner, maintaining patient privacy, and managing discomfort.
Professionalism: Respect, compassion, ethical standards, and confidentiality.
Clinical Judgment: Assesses the student’s ability to select and execute suitable diagnostic assessments and evaluate the advantages and disadvantages of different treatment choices.
Doctor-Patient Communication: Clarity in explaining medical tests, obtaining consent, and educating patients.
Organizational Efficiency: Skill in prioritizing patient care and effectively utilizing resources.
Overall Competence: Integration of clinical knowledge and overall patient care effectiveness.
The Mini-CEX scoring spanned from below expectations (1–3 points), meeting expectations (4–6 points), to exceeding expectations (7–9 points). All assessments were carried out by one evaluator to ensure consistency.
To minimize evaluator bias, multiple evaluators were involved in the Mini-CEX assessments. Inter-rater reliability was assessed using Cohen’s Kappa to evaluate consistency across evaluators. A Kappa value of 0.73 was obtained, indicating substantial agreement among evaluators. This approach ensured that the evaluation of students’ clinical skills was both reliable and objective.
Satisfaction Survey
A feedback survey was exclusively conducted for PBL group to assess the educational impact of the PBL method. The survey demonstrated a strong reliability, with a Cronbach’s Alpha value of 0.832, indicating good internal consistency among the items. The survey evaluated several key aspects of student learning, including engagement, clinical reasoning, communication and team collaboration, feedback quality, and overall satisfaction.
A Likert scale was utilized in the survey, ranging from 1 (strongly disagree) to 5 (strongly agree), to assess participants’ perceptions across various statements. These statements were carefully selected based on a review of the literature on PBL and its effectiveness, as well as expert opinions in medical education. The selected areas were designed to reflect the core components of the PBL approach, which aims to enhance active learning, critical thinking, and collaborative problem-solving skills (Appendix A).
The areas covered included:
Engagement: Students’ active participation and investment in the PBL process.
Clinical Reasoning and Diagnostic Skills: Perceived improvements in clinical judgment, decision-making, and diagnostic reasoning as a result of PBL.
Communication and Team Collaboration: The impact of PBL on students’ communication skills and their ability to collaborate effectively within teams.
Feedback Quality: Students’ perceptions of the quality and usefulness of the feedback they received throughout the PBL sessions.
Overall Satisfaction: Students’ overall satisfaction with the PBL approach, including its perceived effectiveness compared to traditional teaching methods.
Rationale for Item Selection
The items included in the survey were derived from key domains of the PBL methodology as outlined in previous studies.6,7 These domains reflect the primary educational objectives of PBL, namely: increasing student engagement, improving clinical reasoning, fostering teamwork, and providing timely and constructive feedback. To ensure comprehensive coverage of these aspects, we consulted existing PBL evaluation frameworks and sought expert input from faculty members who have substantial experience in PBL-based teaching.
Pilot Testing
Before administering the main survey, a pilot test was conducted with a group of 15 students who had participated in a PBL program. The purpose of the pilot testing was to evaluate the clarity and relevance of the survey items, as well as to identify any ambiguities in the wording.
Feedback from the pilot phase indicated that some items needed minor revisions for clarity and specificity. For example, a question regarding teamwork was revised to better reflect the collaborative nature of PBL. The pilot data also suggested that certain items, particularly those related to clinical reasoning, required slight adjustments to ensure they accurately captured the participants’ experiences. Based on this feedback, minor wording changes were made to improve ease of understanding, but no major structural changes were necessary.
Cronbach’s Alpha Value
The Cronbach’s Alpha value of 0.832 indicated good internal consistency, meaning that the survey items were reliably measuring the same underlying constructs. Typically, a Cronbach’s Alpha value above 0.7 is considered acceptable, and the value of 0.832 supports the reliability of the instrument in assessing students’ perceptions of PBL.
Data Analysis
Statistical analysis of the collected data was executed utilizing SPSS version 22.0. The data were presented as mean ± standard deviation ( ± s). For comparative analysis, quantitative data between the groups were subjected to the t-test, and the chi-square test was employed to analyze the categorical data. A P-value less than 0.05 was deemed to indicate statistical significance. Due to the significance tests conducted for multiple Mini-CEX dimensions, we applied the Bonferroni correction to control the risk of false positives arising from multiple comparisons. The adjusted significance level is 0.007.
± s). For comparative analysis, quantitative data between the groups were subjected to the t-test, and the chi-square test was employed to analyze the categorical data. A P-value less than 0.05 was deemed to indicate statistical significance. Due to the significance tests conducted for multiple Mini-CEX dimensions, we applied the Bonferroni correction to control the risk of false positives arising from multiple comparisons. The adjusted significance level is 0.007.
Results
Theoretical Knowledge Exam Scores
The results from the theoretical knowledge exam showed no significant difference across both groups. The PBL group achieved a mean score of 90.25 ± 2.15, while the traditional teaching group scored 89.78 ± 2.14. No substantial difference was observed between the groups in the independent t-test (p > 0.05), indicating that both teaching methods provided similar support for theoretical learning. Additionally, the grading of the theoretical exam results also showed no noticeable difference between the two groups.
Mini-CEX Evaluation Results
All participants finished the Mini-CEX assessment within an average of 35 ± 0.6 minutes, with post-evaluation feedback taking an average of 6.5 ± 0.5 minutes for each student. The PBL group indicated statistically substantial improvements in several key areas, including medical history taking, clinical decision-making, and comprehensive clinical proficiency in comparison to the traditional teaching group. Table 1 provide a comprehensive comparison of the CEX scoring between the two student groups.
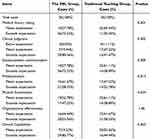 |
Table 1 The Scale Outcomes of the Mini-CEX Evaluation for Both Groups |
Satisfaction Survey Results
The PBL group’s feedback was predominantly positive. Trainees reported considerable satisfaction and eagerness in the teaching method (Table 2). The survey results particularly highlighted active engagement and improvements in Clinical Reasoning and Diagnostic Skills as the most appreciated aspects of the PBL approach.
 |
Table 2 Assessment of Students’ Satisfaction with the PBL Group (n = 36) |
Discussion
This study compares the outcomes of PBL and traditional pedagogical approaches within pediatric clinical clerkships, evaluating the efficacy of PBL in enhancing key aspects of medical education for future pediatricians. Pediatrics, as a specialty, presents unique challenges, including the young age of patients, communication barriers between clinicians, children, and parents, and the complexity of managing pediatric health issues. These factors demand advanced diagnostic and therapeutic skills from pediatricians. Traditional educational models, which often emphasize passive learning, may inadequately prepare students for the multifaceted nature of clinical practice, potentially leading to reduced engagement, limited clinical reasoning, and underdeveloped problem-solving abilities.9
Our study’s PBL model was specifically designed to address these challenges by fostering a learning environment focused on real-life clinical cases, expert guidance, and group collaboration. By incorporating pediatric experts in the PBL sessions and presenting authentic clinical cases for discussion, we ensured the learning experience was both clinically relevant and robust. This aligns with the findings of Hay PJ and Katsikitis M, who highlighted the importance of expert input in enhancing the effectiveness of PBL.10 Additionally, our approach encouraged students to conduct in-depth analyses of clinical cases, considering psychological, familial, and disease-related factors. This multidimensional approach deepened students’ understanding of pediatric care, promoting critical thinking and holistic problem-solving skills.
PBL’s collaborative learning environment highlights the broader educational benefits of group-based learning. In PBL, students collaboratively set learning objectives, analyze case materials, and propose diagnostic and management strategies under the guidance of faculty. This teamwork improves communication skills, enhances clinical reasoning, and strengthens cooperative problem-solving abilities.11 In our study, PBL students performed better in clinical case analysis and medical documentation, further reinforcing the model’s effectiveness in preparing students for the complexities of pediatric practice.
While both groups performed similarly on the theoretical knowledge exam, with no significant difference in scores (PBL group: 90.25 ± 2.15, traditional group: 89.78 ± 2.14, p > 0.05), the minor differences in performance suggest that both teaching methods are equally effective in supporting students’ theoretical learning. The lack of significant improvement in theoretical exam scores between the PBL and traditional teaching groups may be attributed to the nature of the exam itself, which primarily assessed memorization of foundational knowledge rather than the application of knowledge in clinical contexts.12 PBL is designed to enhance higher-order cognitive skills, such as clinical reasoning and problem-solving, which may not be fully captured by traditional theoretical exams.8,11 This suggests that while PBL is highly effective in developing clinical competencies, its impact on rote memorization of theoretical knowledge may be limited.
This finding has important implications for teaching design. Future assessments could be redesigned to include more case-based questions that evaluate students’ ability to apply knowledge in clinical scenarios, thereby providing a more comprehensive measure of PBL’s impact. Additionally, a blended approach that combines PBL with traditional teaching methods may be optimal, as it could leverage the strengths of both approaches to support both theoretical learning and clinical skill development.
Our study also found that PBL students showed significant improvements in clinical competencies, including history taking, clinical decision-making, and comprehensive clinical proficiency, as assessed through the Mini-CEX evaluations. These improvements underscore the value of PBL in developing not just theoretical knowledge, but also the practical skills necessary for successful clinical practice. This is consistent with findings from other studies across different medical specialties, which have demonstrated the positive impact of PBL on clinical problem-solving and diagnostic reasoning.13,14 Additionally, feedback from the PBL group was overwhelmingly positive, with students reporting significant improvements in clinical reasoning, diagnostic skills, and overall engagement. This suggests that PBL not only contributes to tangible academic outcomes but also enhances the subjective educational experience by increasing student motivation, collaboration, and enthusiasm for learning.15,16
However, our study has certain limitations. Firstly, the evaluation primarily focused on examination scores and student satisfaction, which may not fully capture other important aspects of learning, such as long-term retention, real-world clinical performance, and the development of interpersonal skills. Secondly, the student satisfaction survey, being subjective, may have been influenced by factors such as prior familiarity with PBL or enthusiasm for novel teaching methods, which were not controlled for in this study. Additionally, the relatively small sample size of our study, consisting of a limited number of participants, may reduce the generalizability of the findings. The short duration of the intervention is another limitation, as it may not have allowed enough time to observe long-term effects or deeper behavioral changes associated with PBL. Furthermore, the study focused on a specific cohort of students within a unique setting, which may constrain the generalization of the results to different populations or educational contexts.
Despite these limitations, the study has notable strengths. The use of multiple assessment methods—including both objective performance evaluations and subjective feedback surveys—provides a comprehensive view of the PBL model’s impact. This dual approach offers a more nuanced understanding of how PBL influences both academic outcomes and the overall learning experience.
In conclusion, the implementation of PBL in pediatric clinical clerkships proves to be an effective educational strategy. It not only enhances students’ clinical skills and cognitive abilities but also fosters a more engaging and collaborative learning environment. The positive feedback from students suggests that PBL may also promote greater enthusiasm for learning and better prepare students for the complex realities of pediatric practice. As such, PBL should be further explored and integrated into pediatric education, with continued research into its long-term impact on student learning and clinical outcomes.
Data Sharing Statement
All data sets generated for this study were included in the manuscript.
Ethical Approval and Participant Consent
This study complies with the Declaration of Helsinki. The approval was granted by the Committee on Ethics of The First Affiliated Hospital, Sun Yat-sen University. All subjects provided informed consent, with particular attention to data protection concerns considering the inclusion of child health data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project was supported by the Medjaden Academy & Research Foundation for Young Scientists (Grant No. MJA202306065).
Disclosure
All authors confirm no conflicts of interest in this work.
References
1. Fromme HB, Whicker SA, Mahan JD, Turner TL. Update in medical education for pediatrics: insights and directions from the 2010 literature. Med Educ Online. 2012;17:
2. Faisal R, Bahadur S, Shinwari L. Problem-based learning in comparison with lecture-based learning among medical students. J Pak Med Assoc. 2016;66(6):650–653.
3. Zhou J, Zhou S, Huang C, et al. Effectiveness of problem-based learning in Chinese pharmacy education: a meta-analysis. BMC Med Educ. 2016;16:23. doi:10.1186/s12909-016-0546-z
4. Barrows HS, Tamblyn RM. Problem-Based Learning: An Approach to Medical Education. Springer Publishing Company; 1980.
5. Trullàs JC, Blay C, Sarri E, Pujol R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ. 2022;22(1):104. doi:10.1186/s12909-022-03154-8
6. Harriel KL, Parboosingh JT. Improving pediatric problem-based learning sessions in undergraduate and graduate medical education. Curr Opin Pediatr. 2020;32(6):832–836. doi:10.1097/MOP.0000000000000962
7. Ma Y, Lu X. The effectiveness of problem-based learning in pediatric medical education in China: a meta-analysis of randomized controlled trials. Med Baltim. 2019;98(2):e14052. doi:10.1097/MD.0000000000014052
8. Stankunas M, Czabanowska K, Avery M, Kalediene R, Babich SM. The implementation of problem-based learning in health service management training programs. Leadersh Health Serv. 2016;29(4):392–401. doi:10.1108/LHS-04-2015-0010
9. Shamsan B, Syed AT. Evaluation of problem based learning course at college of medicine, Qassim University, Saudi Arabia. Int J Health Sci. 2009;3(2):249–258.
10. Hay PJ, Katsikitis M. The ‘expert’ in problem-based and case-based learning: necessary or not? Med Educ. 2001;35(1):22–26. doi:10.1046/j.1365-2923.2001.00679.x
11. Forbes H, Duke M, Prosser M. Students’ perceptions of learning outcomes from group-based, problem-based teaching and learning activities. Adv Health Sci Educ Theory Pract. 2001;6(3):205–217. doi:10.1023/a:1012610824885
12. Gao J, Yang L, Zhao J, et al. Comparison of problem-based learning and traditional teaching methods in medical psychology education in China: a systematic review and meta-analysis. PLoS One. 2020;15(12):e0243897. doi:10.1371/journal.pone.0243897
13. Galvao TF, Silva MT, Neiva CS, Ribeiro LM, Pereira MG. Problem-based learning in pharmaceutical education: a systematic review and meta-analysis. Sci World J. 2014;2014:578382. doi:10.1155/2014/578382
14. Yoo DM, Cho AR, Kim S. Satisfaction with and suitability of the problem-based learning program at the Catholic University of Korea College of Medicine. J Educ Eval Health Prof. 2019;16:20. doi:10.3352/jeehp.2019.16.20
15. Alduraibi SK, Sadik AE, Elzainy A, Alsolai A, Alduraibi A. Medical imaging in problem-based learning and impact on the students: a cross-sectional study. J Pak Med Assoc. 2022;72(9):1731–1735. doi:10.47391/JPMA.3479
16. Stentoft D. Problem-based projects in medical education: extending PBL practices and broadening learning perspectives. Adv Health Sci Educ Theory Pract. 2019;24(5):959–969. doi:10.1007/s10459-019-09917-1
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

