Back to Journals » Advances in Medical Education and Practice » Volume 16
Comparison of Medical Students’ Peer Evaluation and Teaching Staff Evaluation of Community Health Projects: Perceptions and Experiences
Authors Mahmoud MA, Almutairi ZS, Mahmoud AM , Alanazi HB, Abdulrahman SM, Bin Abdulrahman KA
Received 10 October 2024
Accepted for publication 23 January 2025
Published 25 January 2025 Volume 2025:16 Pages 99—108
DOI https://doi.org/10.2147/AMEP.S494025
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Mahmoud A Mahmoud,1 Zaid Saud Almutairi,2 Abdulrahman M Mahmoud,2 Hind Bashir Alanazi,2 Sundus M Abdulrahman,2 Khalid A Bin Abdulrahman3
1Department of Family and Community Medicine, College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Kingdom of Saudi Arabia; 2College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Kingdom of Saudi Arabia; 3Department of Medical Education, College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Kingdom of Saudi Arabia
Correspondence: Mahmoud A Mahmoud, Email [email protected]
Background: Public health education increasingly emphasizes experiential learning and community engagement. Peer review complements traditional staff evaluation, enhancing learning outcomes and refining teaching strategies. This study aims to investigate the perceptions and experiences of medical students with peer evaluation of community health projects. Staff evaluation for the same projects will be used for comparison.
Methods: A cross-sectional survey study involving medical students from the epidemiology and community health course at the College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU). Students assessed their peers’ community health projects using a self-administered questionnaire. Staff evaluations were also compared. Data was analyzed by IBM SPSS 29.
Results: The study included 187 participants, primarily medical students (98.3%), who evaluated 20 community health projects. Three teaching staff members also rated the same projects. Medical students ranked effort expended (4.34), topic importance (4.26), and apparent participation (4.26) in descending order of value. The Staff evaluated the topic’s relevance as the highest (4.43), but they rated the tools as lower (3.9). Medical students ranked tools sufficiency significantly higher, with a mean of (4.16 vs 3.90) than Staff (p < 0.05). Both groups evaluated the project’s level of innovation and the clarity of its target audience in a comparable manner. The analysis of the Full Project Level indicated no substantial disparity between medical students and Staff, as evidenced by the p-value of 0.920.
Conclusion: This study validates that peer evaluation of student projects is equally practical as evaluation conducted by faculty members. Consequently, allocating resources toward enhancing peer students’ learning and evaluation capabilities is justifiable.
Keywords: student peer evaluation, medical students, community health, student projects, Saudi Arabia
Introduction
Public health education increasingly focuses on experiential learning and community participation.1,2 Community health projects are integral to medical education, as they allow students to utilize their knowledge and abilities to address real-life issues. Community health projects can enhance students’ cooperation, communication, and problem-solving skills.3
Peer evaluation is a procedure whereby students assess and evaluate the work of their fellow classmates. Peer review is an advantageous method for learning and evaluation, as it facilitates the development of students’ critical thinking abilities, enhances their writing proficiency, and enables them to get insights from the work of their peers.4,5
Peer review is a crucial tool for teachers since it offers feedback on their teaching and helps them discover areas where students require more support. There is increasing research on using peer review in medical education.6,7
Empirical evidence demonstrates that peer review is highly effective for enhancing student learning. Further investigation is required about the utilization of peer review as a means of assessing community health initiatives. The significance lies in the fact that community health projects are distinctive tasks that necessitate students to showcase a diverse array of talents and knowledge.8
This type of investigation will yield vital insights into the efficacy of peer evaluation in evaluating community health initiatives. The results will also benefit other educators who are interested in utilizing peer review as a means of evaluating community health initiatives. Peer evaluation of community health projects presents distinct obstacles.
Evaluating the caliber of a community health initiative without possessing specialized knowledge in the project’s unique field can be challenging. Students also face difficulty providing and receiving feedback on very personal and time-intensive projects.9
Peer review can give advantages over staff evaluation, including increased student participation, including various perspectives, and promoting collaborative learning. On the other hand, regular evaluation of teachers provides insufficient evaluation. Nevertheless, other limitations of teacher evaluation may occur, such as limited student involvement, inadequate comprehension among staff members about the community context, and student perspectives, all of which could impact the project’s relevance.10,11
Furthermore, the inherent subjectivity in the evaluation process may result in personal biases or grading criteria that fail to accurately portray a project’s intricacies. The limited amount of time available and the thoroughness of the reviews put pressure on staff members, which may result in a restriction on providing detailed comments.12
Notwithstanding these difficulties, several prospects exist for efficiently utilizing peer evaluation to evaluate community health projects. One option is to utilize peer review to assess particular elements of the projects, such as the research methodology, intervention design, or evaluation strategy. Another option is to use peer review to offer input on the overall excellence of the project, encompassing the lucidity of the presentation, the efficacy of the communication, and the overall influence of the project.13
This strategy provides numerous advantages, such as cultivating critical thinking skills, improving writing talents, and encouraging mutual learning among students, and it has practical applications.14
Moreover, peer evaluation offers instructors vital feedback, allowing them to pinpoint areas where students need extra assistance and improve their teaching methods. Research has indicated that students who participate in peer review exhibit enhanced learning outcomes, as demonstrated by higher post-test scores and self-reported improvements in knowledge and abilities.15
Analyzing the perspectives and experiences of medical students will enhance our comprehension of the significance of peer review in assessing community health programs. Ultimately, this will optimize the efficacy of medical education and promote student learning outcomes. Additionally, it will yield practical recommendations for educators aiming to apply peer review methodologies for community health projects.
Experts in medical education have recognized the need to include peer evaluation in the medical curriculum.16 Some instructors have included this concept in various aspects of the curriculum to cultivate a beneficial practice for medical college students to foster. Researchers and medical educators are enthusiastic about student initiatives emphasizing community health concerns.17 An area that remains unexplored in the medical literature is the contrast between peer evaluation and teacher evaluation.
This study aims to examine medical students’ perspectives and encounters regarding their peers’ evaluation of their community health projects. Staff evaluations were utilized to compare the same projects.
Methods
Study Design and Participants
This cross-sectional analytical study involves all medical students enrolled in the Epidemiology and Community Health course of batch 2023 at Medical College, IMSIU. Furthermore, the three faculty members who were involved in subject teaching and attending the project day were involved in evaluating students’ work as a means of comparing them with peer evaluations. Inclusion criteria included participants being medical students enrolled in the Epidemiology and Community Health course of batch 2023 at Medical College, IMSIU; no exclusion criteria beyond this were employed among those who completed the evaluation. A convenience sampling technique helped to capture the broadest cross-section of medical students. A recruitment letter and a link to an online questionnaire were distributed to all targeted medical students via their official Email addresses. The investigators designed and validated the questionnaire using Cronbach’s Alpha Test and SPSS 23 software. A representative sample of survey respondents showed good dependability (>0.9). Data was collected through November 2023. Participants included 187 students and three faculty members after getting their consent for participation. The sample size was calculated using Raosoft (Raosoft Inc., Seattle, Washington, USA) based on a confidence level of 95% and a 5% margin of error. The total number of registered medical students in batch 2023 is 200. The total sample size calculated was 135. This study received institutional research ethics approval and was designated low risk to human subjects.
Study Measures
Each student was assigned to assess and appraise the community health projects of all their classmates, excluding their own group, by utilizing a peer review form they completed. The peer evaluation questionnaire assessed the facets of the community health projects identical to the instructor’s grading rubric. The questionnaire was utilized to evaluate many areas of each project, including the level of novelty in the project title, the clarity of the target population, the effectiveness of teamwork, the amount of time invested, the suitability of the tools used, the appropriateness and appeal of the designs, the quality of the presentation, and the overall evaluation. The scoring system utilized a rating scale ranging from 1 to 5, where a score of 1 denoted the lowest rating and a score of 5 indicated the best rating. Upon the conclusion of the semester, the instructor requested that all students submit their community health projects for evaluation. The instructor must be aware of the students’ peer evaluation results. There are 20 finished projects, with approximately 200 students enrolled, comprising both males and females. Additionally, there are three staff members, one of whom is female.
Statistical Data Analysis
An extensive statistical analysis was performed on the dataset, incorporating descriptive and inferential methods. Firstly, we conduct a descriptive study of the average and variability of replies by examining the mean and standard deviation. This presents a summary of the research results. Afterward, inferential studies, such as the Mann–Whitney U-Test (used for Non-Parametric Data), investigate the difference in scores between Peer and Staff evaluation. Statistical significance is determined when the p-value is equal to or less than 0.05 and when a 95% Confidence Interval is used. The statistical studies are performed using IBM’s SPSS Software, specifically version 29.0.0.
Results
The study involved a total of 187 participants. Among them, 184 were medical students who conducted 3566 evaluations of the projects, while the remaining 3 participants were Teaching Staff who evaluated the projects 60 times. Furthermore, Table 1 presents the peer evaluation results among medical students. They examined 3496 community health programs, examining different aspects of these projects and reflecting on their own thoughts and experiences. The assessment of various factors, including the level of effort exerted, the significance of the chosen topic, active participation of all students, presentation abilities, clarity in defining the target audience, coordination and adequacy of resources, suitability of tools utilized, attractiveness and appropriateness of designs, and the originality of the project title. The data suggests that the students greatly appreciated the work put in, as evidenced by a mean score of 4.34 out of 5 (SD=0.8), which ranked it in the 1st position.
 |
Table 1 Peer Evaluation of Different Components of Community Health Project by Medical Students (Their Perceptions and Experiences) With Ranking |
Furthermore, the selected issue garnered considerable emphasis, placing it in the second position with a score of 4.26 (SD=0.9). The involvement of every student and the ability to provide effective presentations were both considered essential, receiving scores of 4.26 and 4.25, respectively, and ranking 3rd and 4th. The target group’s definition, coordination of offerings, and provision of adequate tools were significantly less important but still crucial, with average scores ranging from 4.21 to 4.16. In contrast, the designs’ appropriateness and the project title’s innovativeness received lower rankings in comparison, with mean values of 4.05 and 3.78, respectively, ranking 8th and 9th.
Table 2 displays the evaluation outcomes of a team of three staff members. They analyzed 60 distinct community health projects on various aspects of these programs. Based on the staff evaluation, the chosen topic was rated as highly important, receiving a mean score of 4.43 out of 5 (SD=0.5), which ranked it in the 1st position. The participation of all pupils was evident, with a mean score of 4.25 (SD=0.7), placing them in the second position. The level of exertion and the organization and adequacy of received proposals had average scores of 4.22, putting them in the third and fourth positions, respectively. Identifying the specific audience and creating visually appealing designs received somewhat lower ratings, with mean scores of 4.15 and 4.13, respectively, placing them in the 5th and 6th positions. The instruments’ adequacy obtained an average score of 3.9 (SD=0.8), putting it in the 7th position. The project title’s innovativeness obtained the lowest mean score of 3.83 (SD=0.9), ranking 8th. In summary, the staff evaluation highlights the necessity of choosing a suitable and pertinent topic for community health initiatives, the value of student involvement, and the effort they put in.
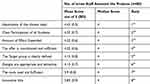 |
Table 2 Peer Evaluation of Different Components of Community Health Project by Staff With Ranking |
Table 3 compares evaluations between medical students and staff members regarding several components of community health projects. Both students and Staff gave similar ratings for the innovative title, with mean scores of 3.78 (SD = 1.1) and 3.83 (SD = 0.9) respectively (p = 0.908). The clarity in defining the target group was rated 4.21 (SD = 0.8) by students and 4.15 (SD = 0.8) by Staff (p = 0.428). The importance of the chosen topic was slightly higher among Staff, 4.43 (SD = 0.5), compared to 4.26 (SD = 0.9) by students (p = 0.461). The effort expended was rated similarly high by both groups but slightly higher by students at 4.34 (SD = 0.8) compared to 4.22 (SD = 0.6) by Staff (p = 0.056). Both groups agreed on the evident participation of all students, 4.26 (SD = 0.8) for students and 4.25 (SD = 0.7) for Staff (p = 0.623). A significant difference was found in the use of sufficient tools, where students rated it higher at 4.16 (SD = 0.9) compared to 3.90 (SD = 0.8) by Staff (p = 0.013). The appropriateness and attractiveness of designs and the coordination and sufficiency of the offer were similarly rated between both groups, with no significant differences observed (p = 0.992 and p = 0.508, respectively).
 |
Table 3 Evaluation of Different Components of Community Health Project Between Medical Students and Staff |
Figure 1 displays a visual comparison of average ratings (ranging from 1 to 5) for different components of community health projects, as evaluated by medical students and staff members. Medical assessed students and the relevance of the chosen topic was lower than that of Staff, with mean values of 4.26 and 4.43, respectively. In contrast, medical students consistently rated the effort exerted higher (4.34 compared to 4.22 by Staff) and the clarity of defining the target group higher (4.21 compared to 4.15 by Staff). Furthermore, there was a notable disparity in the evaluation of tool adequacy, as medical students assigned an average score of 4.16, while staff members ranked it lower at 3.9. Although the majority of components received similar ratings, significant variations were observed in areas such as tool adequacy.
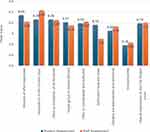 |
Figure 1 Graph showing the comparison of mean scores (out of 5) between Different Components of Community Health Project between Medical Students and Staff. |
Table 4 presents the comprehensive evaluation at the Full Project Level, comparing medical students and Staff. For the student evaluation, the mean score is 4.19 with an SD of 0.8, compared with the staff evaluation with a mean score of 4.20 with an SD of 0.7 with a minimal effect size of −0.00 (Cohen’s d). The Mann–Whitney U-test resulted in a p-value of 0.920, suggesting no statistically significant difference in the overall perception of the entire project between medical students and Staff. Therefore, medical students and Staff had equal evaluations of the overall impression at the Full Project Level, as evidenced by the insignificant p-value obtained from the Mann–Whitney U-test.
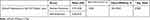 |
Table 4 Overall Impression at the Full Project Level Between Medical Students and Staff |
Figure 2 displays the ratio of different community projects evaluated by both students and staff members. Projects focused on improving respiratory health, namely addressing asthma and depression in teenagers, achieved 5% and 4.6% success rates, respectively. Additional notable initiatives encompass Diabetes control (4.4%), Obesity awareness (4.2%), and Cervical cancer screening (4.2%). Projects focused on mental health, patient safety, and Alzheimer’s had a participation rate of approximately 4%. Projects that specifically targeted illnesses such as PCOS and Rabies had moderate scores of 3.7% and 3.3%, respectively. Projects such as ADHD awareness, Forensic Medicine, and Malaria elimination had lower involvement percentages, specifically 2.8%, 2.5%, and 2.3%, respectively. The participation rate for smoking cessation was the lowest, at 1.7%.
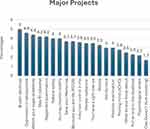 |
Figure 2 Proportion of essential community projects assessed by participants. |
Discussion
Public health education prioritizes hands-on learning and active involvement in the community, creating a mutually beneficial relationship between academic institutions and community organizations. This approach allows students to develop their skills and knowledge.18 Community health initiatives in medical education promote the development of teamwork, communication, and problem-solving abilities. Lestari et al (2019) demonstrate that students in the health professions can acquire collaborative practice abilities while encountering challenges in communication and mutual support.19 According to Marie et al (2021), peer evaluation facilitates learning, offers feedback, and enables students to evaluate the learning results of peers with similar standing, leading to self-reflection on their own learning experiences.20 Challenges encompass evaluating the standard of the project and obtaining feedback from students. Peer review, in comparison to staff evaluation, actively involves students and provides a variety of viewpoints, hence improving learning results. Our study offers useful insights into how medical students and teaching staff perceive and experience peer evaluation of community health projects.
Undoubtedly, fostering students’ mastery of peer evaluation skills enhances their acquisition of various skills and boosts their self-confidence and capacities. One of the benefits that students get from evaluating their peers is the ability to provide constructive criticism.21 They learn to highlight the positive elements first and then address areas that need work. These factors encompass the development of accountability, self-validation, collaborative task execution, effective problem-solving, teamwork abilities, and satisfaction upon project completion.22
The distinguishing factor is the gratification derived from actively resolving societal distress and health predicaments.23 Our study demonstrated the favorable implications of implementing this paradigm at medical and health institutions, particularly for student community health projects.
Our study found that most actively involved students are willing to participate in peer evaluation. This is in contrast to the findings of N.-F. Liu et al (2006) discovered that many students resist peer evaluation when assigning grades. Additionally, most students reported that they only sometimes rate their peers in evaluation activities.24 Significantly, the peer evaluation among medical students unveiled other crucial discoveries. Initially, the students greatly appreciated the effort put into community health projects, as indicated by the high average score of 4.34 out of 5 and its position as the highest priority. This focus on exertion is consistent with other research by Pfarr et al (2013), which suggests that medical students frequently acknowledge and value the commitment and diligent effort invested in endeavors.25 In addition, the chosen issue garnered considerable interest from students, placing second with a mean score of 4.26. This conclusion supports the existing literature that emphasizes the importance of choosing relevant and impactful issues in community health programs, as mentioned by Battista et al, demonstrating that selecting relevant and impactful subjects is an essential step.26
In addition, medical students considered the active involvement of all students and effective presentation abilities to be essential, ranking them third and fourth in importance, respectively. The focus on participation and communication skills highlights the cooperative aspect of community health programs and their function in promoting collaboration and efficient communication among students. Rowthorn et al (2014) stress the significance of universities prioritizing students’ engagement with various professionals, improving their communication abilities, and promoting their involvement in community health projects that require teamwork to address intricate global health issues.27
Significantly, the study revealed that students hold their peers’ work and projects in higher regard and value than that of their teachers. This can be attributed to the students’ profound recognition of the beneficial influence that encouragement and assistance have on their academic success, particularly when it pertains to grades and improving the student’s academic performance. The student also enjoys improving his colleagues’ marks, experiencing the same satisfaction he experiences when his colleagues assess his own performance.
Furthermore, the evaluation carried out by the teaching staff offered further perspectives on community health projects. Staff members highlighted the significance of choosing a suitable project topic, as evidenced by the highest average score of 4.43 and its ranking as the top priority. This discovery emphasizes the importance of educators in directing students toward choosing subjects that align with the aims and objectives of community health initiatives.
In addition, the staff members highlighted the significance of student involvement and the effort put forward, as seen by the high marks given to these aspects. The agreement between students’ perspectives and this alignment indicates a mutual comprehension between both groups regarding the crucial elements of community health projects. Nevertheless, variations in evaluating particular aspects, such as the originality of project titles, emphasize the subtle viewpoints of staff members in contrast to students.
The comparison between medical students and teaching staff indicated similarities and differences in their evaluations of community health projects. Although both groups gave equal ratings to most components, there were notable disparities in evaluating the adequacy of the tool. Medical students evaluated the adequacy of tools substantially higher than teaching professionals, suggesting a possible disparity in comprehension or priorities between the two groups. Schiekirka and Constantinou et al (2018, 2022) demonstrate the contrasting perspectives of students and teachers about an evaluation instrument employed in surveys conducted at two medical schools in Germany.28,29
The results of this study align with earlier research conducted by Könings et al (2014), which emphasized the differences in viewpoints between students and staff members on several areas of education and learning.30 The discrepancy in evaluations highlights the significance of considering various viewpoints when assessing the caliber and efficacy of community health initiatives. Furthermore, it underscores the importance of continuous communication and collaboration between students and Staff to guarantee consistency in expectations and priorities.
The significance of the effort exerted, the selection of a suitable topic, and the function of efficient communication and participation have constantly been recognized as crucial elements in achieving community health projects. Similarly, Hegg et al (2020) presented the findings of their study, which revealed that facilitators exhibited greater leniency compared to peer observers when evaluating team performance. The reliability was high for medical and postgraduate nursing students and moderate for undergraduates. Peer evaluation is a supplement to faculty evaluation, but it does not substitute it.31
Furthermore, the differences between the evaluations made by students and staff members reflect the results of prior research investigating various individuals’ viewpoints in educational environments.32
These disparities emphasize the necessity of thoroughly comprehending various perspectives and the significance of promoting transparent discussions and cooperation among all parties engaged in community health initiatives.
Implications and Recommendations
Our study indicates that students and Staff should communicate continuously to ensure that their expectations are in agreement. To resolve disparities in evaluations, particularly about the adequacy of tools, it is necessary to have access to resources and get help from Staff. Subsequent investigations should examine the enduring effects of peer evaluation on educational achievements and the quality of projects by conducting longitudinal studies.
Limitations
This study has a few drawbacks, including the possibility of biases in peer evaluation, such as leniency or subjectivity. The limited generalizability of the findings may be attributed to the very small sample size, which consists mainly of medical students. A lack of control over external circumstances, such as fluctuations in project complexity or student ability, could influence the validity of the results.
Conclusion
The objective of our study is to examine the perspectives of medical students and teaching staff regarding the evaluation of community health programs by their peers. The text highlights the significance of exertion, choice of subject, and proficient communication. The disparities in tool adequacy evaluation emphasize the necessity for continuous collaboration. By addressing these inequalities, peer evaluation can improve the quality and efficacy of projects. This empowers students to take an active role in promoting community health and making positive changes.
Data Sharing Statement
All data sets collected during this study are available upon reasonable request from the corresponding author.
Ethical Approval
The Institutional Review Board, Imam Muhammad Ibn Saud Islamic University, approved the study (project number 567/2023 approval date, 9/1/2024). All writing was done according to the ethical principles of the Declaration of Helsinki. The survey link included a brief study description and a more detailed explanation on the front page.
Informed Consent
Written informed consent was obtained from all participants included in the study.
Acknowledgment
The authors would like to thank the college students who all participated in the survey.
Funding
This research received no external funding.
Disclosure
The authors declare no conflict of interest.
References
1. Blenner SR, Roth SE, Manukyan R, et al. Community partnerships and experiential learning: investing in the next generation of a diverse, qualified public health workforce. Pedagogy Health Promotion. 2021;7(1_suppl):51S–62S. doi:10.1177/23733799211046974
2. Ezezika O, Gong J. Experiential learning in the classroom: the impact of entrepreneurial pitches for global health pedagogy. Pedagogy Health Promotion. 2021;7(2):118–126. doi:10.1177/2373379920930723
3. Chorazy ML, Klinedinst KS. Learn by doing: a model for incorporating high-impact experiential learning into an undergraduate public health curriculum. Front Public Health. 2019;7:437671. doi:10.3389/fpubh.2019.00031
4. Elshami W, Abdalla ME. Peer evaluation in health professions education. J Edu Technol Health Sci. 2018;5(1):8–14.
5. Boase-Jelinek D, Parker J, Herrington J. Student reflection and learning through peer reviews. Issues Edu Res. 2013;23(2):119–131.
6. Hanrahan SJ, Isaacs G. Assessing self-and peer-evaluation: the students’ views. Higher Edu Res Dev. 2001;20(1):53–70. doi:10.1080/07294360123776
7. Sriwigati D, Musharyanti L. Benefits and challenges of peer learning methods in health professional students: a literature review. Bali Med J. 2022;11(3):1626–1631. doi:10.15562/bmj.v11i3.3755
8. Mukherjee S, Gangopadhyay T, Bagchi H, Mukherjee S, Sinha B. Implementing peer evaluation to explore medical student’s conceptual learning and contribution to project-based assignment. Nat J Physiol Pharm Pharmacol. 2023;13(7):1504.
9. Boud D, Molloy E. Rethinking models of feedback for learning: the challenge of design. Eval Eval Higher Edu. 2013;38(6):698–712.
10. Magolda MBB. Making Their Own Way: Narratives for Transforming Higher Education to Promote Self-Development. Routledge; 2001.
11. McKay VC, Estrella J. First-generation student success: the role of faculty interaction in service-learning courses. Commun Educ. 2008;57(3):356–372. doi:10.1080/03634520801966123
12. Carless D, Boud D. The development of student feedback literacy: enabling uptake of feedback. Eval Eval Higher Edu. 2018;43(8):1315–1325.
13. Søndergaard H, Mulder RA. Collaborative learning through formative peer review: pedagogy, programs and potential. Computer Sci Edu. 2012;22(4):343–367. doi:10.1080/08993408.2012.728041
14. Eyler J, D.e. G Jr. Where’s the Learning in Service-Learning? Jossey-Bass Higher and Adult Education Series. ERIC; 1999.
15. Topping K. Peer evaluation between students in colleges and universities. Rev Educ Res. 1998;68(3):249–276. doi:10.3102/00346543068003249
16. Lerchenfeldt S, Taylor TAH. Best practices in peer assessment: training tomorrow’s physicians to obtain and provide quality feedback. Adv Med Educ Pract. 2020;11:571–578. doi:10.2147/AMEP.S250761. PMID: 32922116; PMCID: PMC7457869.
17. Buhumaid R, Otaki F, Czabanowska K, et al. Professionalism-training in undergraduate medical education in a multi-cultural, multi-ethnic setting in the Gulf Region: an exploration of reflective essays. BMC Med Educ. 2024;24(1):117. doi:10.1186/s12909-024-05103-z. PMID: 38321450; PMCID: PMC10848390.
18. Comeau DL, Palacios N, Talley C, et al. Community-engaged learning in public health evaluation of utilization and value of student projects for community partners. Pedagogy Health Promotion. 2019;5(1):3–13. doi:10.1177/2373379918772314
19. Lestari E, Scherpbier A, Stalmeijer R. Stimulating students’ interprofessional teamwork skills through community-based education: a mixed methods evaluation. J Multidiscipl Healthcare. 2020;13:1143–1155. doi:10.2147/JMDH.S267732
20. Marie S, Mangrio E, Bengtsson M, et al. Formative peer evaluation in higher healthcare education programmes: a scoping review. BMJ Open. 2021;11(2):e045345. doi:10.1136/bmjopen-2020-045345
21. Chin P. Peer assessment. New Directions Teaching Nat Sci. 2016;3:13–18. doi:10.29311/ndtps.v0i3.410
22. Altınay Z. Evaluating peer learning and assessment in online collaborative learning environments. Behaviour Inf Technol. 2016;36(3):312–320. doi:10.1080/0144929X.2016.1232752
23. Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. 2010;30(7):865–878. doi:10.1016/j.cpr.2010.03.001. Epub 2010 Mar 12. PMID: 21151705; PMCID: PMC2998793.
24. Liu N-F, Carless D. Peer feedback: the learning element of peer evaluation. Teach Higher Educ. 2006;11(3):279–290. doi:10.1080/13562510600680582
25. Pfarr CM, Bramblett D, Osborne D, et al. A laboratory for education in molecular medicine: a dedicated resource for medical student research. Med Sci Educator. 2013;23:108–118. doi:10.1007/BF03341815
26. Battista RN, Hodge MJ. Setting priorities and selecting topics for clinical practice guidelines. Cmaj. 1995;153(9):1233–1237.
27. Rowthorn V, Olsen J. All together now: developing a team skills competency domain for global health education. J Med Law Ethics. 2014;42(4):550–563. doi:10.1111/jlme.12175
28. Schiekirka‐Schwake S, Dreiling K, Pyka K, et al. Improving Evaluation at two medical schools. ClinTeacher. 2018;15(4):314–318. doi:10.1111/tct.12686
29. Constantinou C, Wijnen-Meijer M. Student evaluations of teaching and the development of a comprehensive measure of teaching effectiveness for medical schools. BMC Med Educ. 2022;22(1):113. doi:10.1186/s12909-022-03148-6
30. Könings KD, Seidel T, Brand-Gruwel S, van Merriënboer JJ. Differences between students’ and teachers’ perceptions of education: profiles to describe congruence and friction. Instructional Sci. 2014;42:11–30.
31. Hegg RM, Ivan KF, Tone J, et al. comparison of peer evaluation and faculty evaluation in an interprofessional simulation-based team training program. Nurse Edu Pract. 2020;42:102666. doi:10.1016/j.nepr.2019.102666
32. Haarala-Muhonen A, Ruohoniemi M, Katajavuori N, et al. Comparison of students’ perceptions of their teaching–learning environments in three professional academic disciplines: a valuable tool for quality enhancement. Learning Environ Res. 2011;14:155–169. doi:10.1007/s10984-011-9087-x
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

