Back to Journals » Advances in Medical Education and Practice » Volume 15
Confidence in Prescribing Practices: Perspectives of Senior Medical Students and Recent Graduates at Qatar University
Authors Allouch S, Ali RM, Seed Ahmed M , Akhtar S , Awaisu A , Bidmos M
Received 30 April 2024
Accepted for publication 8 November 2024
Published 28 December 2024 Volume 2024:15 Pages 1325—1337
DOI https://doi.org/10.2147/AMEP.S476352
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Soumaya Allouch,1 Raja Mahamade Ali,2 Mohammed Seed Ahmed,1 Saghir Akhtar,1 Ahmed Awaisu,2 Mubarak Bidmos1
1Department of Basic Medical Sciences, College of Medicine, QU Health, Qatar University, Doha, Qatar; 2College of Pharmacy, QU Health, Qatar University, Doha, Qatar
Correspondence: Mubarak Bidmos, Department of Basic Medical Sciences, College of Medicine, QU Health, Qatar University, Doha, Qatar, Tel +974 7054 3213, Email [email protected]
Purpose: This study aimed to determine the perceptions of senior medical students and recent graduates from College of Medicine (CMED) at Qatar University regarding their undergraduate education and training related to prescribing, their confidence in achieving the learning outcomes specified in the curriculum and their preparedness to prescribe in practice.
Patients and Methods: This was a cross-sectional web-based survey with qualitative elements, utilizing a 22-item pre-validated questionnaire developed through a multi-phase iterative process. The survey was administered to all senior medical students (year 4– 6) and recent graduates of CMED at Qatar University.
Results: One hundred sixty-seven medical students and graduates responded to the survey (response rate ~45%). Overall, the participants expressed positive attitude towards curricular content related to prescribing that aimed to prepare them for practice, including pharmacology and therapeutics, history-taking, physical examination, diagnostic investigations, application of evidence-based medicine, and other skills. Over 60% of the participants believed that the prescribing components of the undergraduate curriculum made them competent in providing safe and effective prescriptions in practice. Notably, there was an association between seniority and perceived curricular effectiveness, highlighting the impact of clinical experience on participants’ views. Recommendations for curriculum enhancement focused on practical integration, contextualized education, and a holistic approach to both theoretical and clinical learning.
Conclusion: The study revealed positive opinions regarding curricular content related to prescribing and identified areas for improvement in medical curriculum. Continuous monitoring, evaluation and refinement based on participants’ feedback are crucial for ensuring the preparedness of medical graduates for safe and effective prescribing in real-world clinical practice.
Keywords: medical education, curriculum evaluation, contextualized education, curriculum enhancement
Introduction
Medication therapy is the most frequently employed intervention in the management of acute and chronic medical conditions,1 making prescribing a very crucial competency for medical graduates. In the United States alone, it was estimated that about 6.7 billion prescriptions were dispensed in 2022.2 The increase in the number of older adults in the community, along with a significant surge in multi-morbidity rates, has contributed to the widespread occurrence of polypharmacy, characterized by the use of multiple medications. This trend has increased the complexity of prescribing process.3
Prescribing is one of the core competencies in medical curricula globally therefore, it is highly linked with key program learning outcomes.4,5 Developing the skill to prescribe safe and effective medicines for patients is crucial and should be instilled in physicians during their undergraduate medical education. Nonetheless, there is currently a lack of emphasis on providing comprehensive training to students in prescribing skills.1,6 This is further proven by the reported significant occurrence of prescribing errors committed by doctors within hospital environment.7–10 The bulk of these prescribing errors are attributed to early-career or junior doctors.8,11 Additionally, in the United Kingdom (UK), more than 80 million clinically significant medication errors resulted from prescribing in primary care alone in 2021.12
There is sufficient evidence in the literature that inadequate training in appropriate prescribing is often contributory to the occurrence of such events.8,11 Although the phenomenon of inadequate prescribing competency in medical curriculum is a global one, the intensity varies from one country to another, and many developed countries have taken measures to ensure safe prescribing practices. Deficiencies in prescribing knowledge and skills can result in fatal prescribing errors. However, providing prescribing related education has been shown to improve prescribing competencies among medical graduates and hence reduce prescribing errors in practice.5,13
In Qatar University, new medical graduates are expected to be competent in safe and effective prescribing as enshrined in the undergraduate medical curriculum. Starting from the fourth year of the Doctor of Medicine (MD) program at the College of Medicine (CMED), students are introduced to the concepts of prescription writing through organized workshops. During these clinical years, the students learn about pharmacology of drugs used in different disease states, history-taking, physical examination, clinical management of diseases, and other skills relevant to prescribing skills through clinical practice.
A further reinforcement on prescription writing skills is provided in the Preparation for Practice clerkship, which runs in the final year of the MD program at our university. The course is strategically placed at the end of the clerkship program and is considered to be a preparatory course for the residency program. A prescribing skills evaluation, contributing 20% to the overall grade, is one of the elements included in the final summative assessment at the conclusion of the course. Amongst other learning outcomes of the course, students should be able to “demonstrate competence in the safe prescribing of drugs and intravenous fluids”. Ultimately, as these students transition into practice as new graduates, they will encounter the responsibility of delivering care to diverse patient populations and prescribing a considerable number of medications.
In Australia and the UK, prescribing frameworks for healthcare professionals, including physicians, are available.14–16 In addition, the UK has developed a prescribing safety assessment for medical graduates to demonstrate knowledge and skills competencies in relation to the safe and effective use of drugs.17,18 This assessment is designed to be a valid and reliable battery for assessing prescribing competencies as defined by the General Medical Council (GMC).19 To enhance the prescribing safety and skills of graduating doctors, CMED at Qatar University requires medical students in their final year of undergraduate medical training to undergo a prescribing skill assessment. The Prescribing Skills Assessment (PSA) is an online educational and assessment tool for institutions and organizations to enhance students’ skills in prescribing.20 It is delivered as a joint partnership between the British Pharmacological Society and the Medical Schools Council in the UK.
In Qatar, there is currently no professional regulatory authority or professional body overseeing medical education, and there are no nationally recognized standards for knowledge and skills competencies in prescribing for medical graduates. Educators with diverse educational backgrounds have incorporated content related to prescribing competencies by adapting materials from other developed countries. However, the extent to which the learning objectives of this curricular content are met from the learner’s perspective remains unknown. Although a prior curricular mapping study had explored prescribing competencies within pharmacy curriculum at Qatar University,21 there is currently no research examining the perspectives and confidence level of recent medical graduates and senior medical students at CMED regarding their prescribing competencies and abilities. The perspectives and experiences of medical students and recent graduates hold a significant importance in ensuring that graduates possess the required skills and confidence to assume this role in practice. Thus, the aim of this study was to determine the perceptions of senior medical students and recent graduates from CMED at Qatar University regarding their undergraduate education and training related to prescribing, their confidence in achieving the learning outcomes specified in the curriculum and their preparedness to prescribe in practice.
Materials and Methods
Study Design
This study was a cross-sectional study with qualitative elements that was conducted using an online survey including close-ended and open-ended questions to collect both quantitative and qualitative data. Data were collected from November 2023 to January 2024. Qualitative data were collected through open-ended questions to increase the validity and ensure achievement of the study outcomes.22
Study Setting
The study was conducted at the College of Medicine (CMED), Qatar University. The CMED was founded in 2015, and offers a six-year MD degree. Currently, there are about 500 students across all professional years. Producing a community of future clinicians who are patient-centered and skilled in caring for people with respect and compassion is the College’s primary educational philosophy.
The College was established in line with international accreditation requirements for medical programs, as specified by the Accreditation Council for Graduate Medical Education (ACGME), the Liaison Committee on Medical Education (LCME) and the World Federation for Medical Education (WFME). In 2024, the CMED achieved full six-year accreditation status from the Association for Evaluation and Accreditation of Medical Education Programs (TEPDAD).
Study Population and Subjects
The study population comprised all current senior medical students in phases II and III of the MD program (ie, students in years 4, 5 and 6) and recent graduates from CMED (ie, graduates of 2020/21, 2021/22 and 2022/23 academic years). A database of current students and recent graduates (alumni) with their names and contacts was obtained from the Associate Dean for Academic Affairs.
Inclusion Criteria
All current senior medical students (from year 4 to year 6) at the CMED, Qatar University and recent graduates of 2020/21 and 2021/22 academic years were eligible for inclusion.
Subjects’ Identification and Recruitment
Potential participants who satisfied the eligibility criteria for the study (see above) were invited to participate in the study. This involved sending individual e-mail invitations containing the consent form and the link to the questionnaire to all eligible participants. The informed consent obtained from participants included permission for the publication of their anonymized responses and direct quotes. A reminder was sent via Email on a weekly basis for four weeks. Completing the online survey implied consent to participate as indicated in the informed consent form.
Sample Size
An invitation to participate in the study was sent to 202 senior medical students and 164 graduates (total = 366). A whole population sampling was used in this study since the population was small. Therefore, sample size determination was not required.
Survey Instrument Development and Administration
A questionnaire (Supplementary Material 1) was developed by the investigators through a multi-step iterative process. First, a comprehensive review of the literature was conducted. Second, a thoughtful assessment of the pedagogical aspects of the investigation based on the study objectives was carried out by the investigators. Importantly, the UK General Medical Council (GMC) prescribing competence framework and Australia’s National Prescribing Competencies (NPS) MedicineWise Competencies Required to Prescribe Medicines were used in developing the relevant parts of the questionnaire.23,24 The questionnaire was validated using face and content validity. Face and content validity of the questionnaire were determined by a group of researchers with experience in the field of medical and pharmacy education. Several modifications were made to the first draft of the questionnaire through an iterative process, resulting in a reconciled second draft.
The second draft was subjected to a quantitative content validity analysis to determine the comprehensiveness and representativeness of items and identify items with low indices that may be removed from the questionnaire. A panel of six experts including four pharmacists and two physicians that are also educators from academia evaluated the relevance of each item in the instrument by scoring on a three-point Likert scale (1 = Not necessary, 2 = Useful but not necessary, 3 = Essential). Content Validity Index (CVI) was determined and changes were made in the questionnaire based on the suggestions of the experts to reach a final version. The language of the questionnaire was English, as it is the official language of instruction at CMED, Qatar University. The final instrument consisted of three sections: Section A for sociodemographic information (4 items); Section B contained close-ended questions about education and training related to prescribing competencies in the curriculum with 5-point Likert scale response options (15 items) and Section C comprised three open-ended questions. The response options for Section B ranged from strongly agree to strongly disagree. In addition, a reliability analysis was performed using Cronbach’s Alpha coefficient. The analysis revealed a Cronbach’s Alpha of 0.935 for the 15 standardized items assessing perceptions/confidence about education and training in prescribing competencies within the curriculum, demonstrating excellent reliability. A copy of the final version of questionnaire is available through the corresponding author.
The final version of the 22-item questionnaire was designed on SurveyMonkey® (SurveyMonkey®, San Mateo, California, United States). The web-based survey was used to obtain anonymous responses from current senior medical students and recent graduates. Participants received an initial Email as well as follow-up emails on weekly basis for one month. The initial Email identified the purpose of the study, the consents, and a link to the online survey.
Ethical Considerations
The study was approved by Qatar University Institutional Review Board (QU-IRB 1893-EA/23). All collected data were anonymous and no findings which could identify any individual participant are available.
Data Analysis
Data analyses were performed using Statistical Package for Social Sciences (SPSS®) version 26 (IBM Statistics for Windows; IBM Corp, Armonk, New York, USA). Both descriptive statistics and chi-square tests were used for the data analyses. Frequencies and percentages were used to summarize the responses generated, as items in Sections A and B were all categorical. Additionally, the chi-square test was used to examine the differences in perceived competence levels across various sociodemographic characteristics, including gender, year of study/graduation, country of origin, and GPA. The level of significance was set a priori at p <0.05. For the qualitative part of the analysis, an inductive thematic approach and content analysis were followed. Content analysis is an analytical approach followed to identify and interpret meaning in recorded communications such as open-ended questions.25 Qualitative data were read by the investigators for familiarization and to ensure immersion in the data, and then content analysis was conducted for the participants’ responses related to the open-ended questions, and units of meaning were identified then condensed and used to generate codes using these responses. Codes were compared and similar phrases were clustered together in the same category. Irrelevant codes were discarded, and similar category codes were placed under respective category. During the development of the codes and categories, the researchers followed the manifest analysis approach in which they focused on the words and phrases used by the respondents in answering the open-ended question and not the underlying meaning.26 Consensus and opinions of all research team members were required to finalize the categories.
Results
One hundred and sixty-seven participants responded to the survey, resulting in a response rate of 45.6%. A higher response rate was noted amongst current students (62.4%) when compared to the medical graduates (24.4%). The majority of the respondents were female (65.9%) and non-Qatari (63.5%). Notably, 70.5% of the participants reported a Grade Point Average (GPA) of 3 or higher. Detailed demographic characteristics are provided in Table 1.
 |
Table 1 Demographic Characteristics of Medical Students and Graduates at Qatar University (n = 167) |
Quantitative Results
Around 60.5% of the participants opined that the knowledge acquired in pharmacology and clinical management during their undergraduate education was effective in developing safe and effective prescribing skills. The majority of the participants (85.6%) agreed that the knowledge and skills they acquired during their undergraduate education at CMED on history taking and physical examination have helped them in developing the skills of safe and effective prescribing. Similarly, diagnostic and clinical investigations of various diseases taught in the undergraduate curriculum were perceived to be useful in developing prescribing competence by around 75% of the study participants (see Table 2).
 |
Table 2 Medical Students’ and Graduates’ Perceptions About Education and Training Related to Prescribing Competencies in the Curriculum (n = 167) |
Additionally, nearly two-thirds of the students and graduates (66.5%) indicated that the amount of teaching they received in the area of concepts and application of evidence-based medicine was sufficient, aiding in their learning process and acquisition of safe and effective prescribing skills. However, only 44.3% of the participants agreed that the prescribing competencies taught within the curriculum were well distributed across different units, clerkships and professional years. The majority of the respondents (80.8%) reported that the educational system facilitated their access to drug information resources like UpToDate® and British National Formulary (BNF), aiding in their acquisition of the required prescribing competencies and skills. A relatively lower proportion of the respondents (approximately 59%) believed that the methods used to deliver prescribing content successfully integrated both theoretical and practical aspects. Likewise, only 46.1% of the responding students and graduates believed that formative feedback was a useful educational tool that enhanced their understanding of safe and effective prescribing practices. Yet, the majority of them (71.3%) indicated that the summative assessments, presented in the form of quizzes and other forms of professional examinations, provided them with realistic examples of the prescribing role of a physician in practice (Table 2).
More than half of the participants (59.9%) indicated that the prescribing content taught to them during their undergraduate studies was representative of real-life experiences they faced in clinical practice either during their clerkships or at work after graduation. However, around 11% of the respondents perceived the prescribing components of the curriculum as distant from practice, while 29% of the participants took a neutral stance. Nevertheless, approximately, 80% of the participants believed that prescribing skills are predominantly acquired through practical experience, either during clerkships or in the professional settings after graduating from CMED.
Overall, 62.9% of the respondents expressed their confidence to apply the knowledge and skills acquired during undergraduate medical education for safe and effective prescribing in clinical practice. Furthermore, the majority of participants affirmed their ability to integrate the ethics and professionalism-related knowledge and skills obtained from the medical curriculum into the practice of prescribing safely and effectively. Many of the participants (61.1%) believed that the prescribing-related content of the curriculum has helped them in becoming competent in prescribing safely and effectively in practice (Table 2).
The outcomes of our study indicate an association between seniority of the students/graduates and their perceptions of the effectiveness of prescribing elements in the undergraduate curriculum. The results suggest that the number of years of education has a significant impact on how individuals perceive their proficiency in prescribing medication safely and effectively (P < 0.001) (Table 3). For instance, only 43.1% of year 4 students agreed that the prescribing components of the undergraduate curriculum made them competent in prescribing safely and effectively in practice, whereas this percentage increased to 95% among recent graduates.
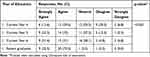 |
Table 3 Medical Students’ Perception of Their Prescribing Competence |
Open-Ended Responses’ Results
Elements of the Curriculum Which Helps in Developing Prescribing Skills
Several codes emerged from the participants’ responses to the open-ended questions (Table 4). Clinical skills, pharmacology content and problem-based learning sessions were identified by the respondents as elements of the curriculum which helped students in developing prescribing competencies.
 |
Table 4 Categories Emerging from Responses to Open-Ended Questions |
Clinical skills sessions were very helpful and prepared me for the real work at hospitals. It was also beneficial that we got exposed to clinical settings like PHCC (Primary Health Care Centers) from early academic years. This helped me practice my history taking and physical examination skills more. (a year 6 student)
However, other students were not satisfied with the prescribing content in the curriculum as they felt it did not prepare them sufficiently for their practice:
The only support we had as students was pharmacology lectures that provide basic ideas on how medications work. However, I do not think that this information is sufficient to be able to officially prescribe medications to patients as there are other factors (aside from learning in university) that influence what and how certain medications should be prescribed. I think my experience in hospital made me more confident to prescribe, but I still have a lot to learn. (a year 5 student)
Areas for Improvement in the Curriculum
The participants also highlighted several areas requiring improvement in the curriculum. To enhance effective prescribing skills acquisition among medical students, the participants recommended providing students with opportunities to practice prescribing during clinical rotations and realistic case scenarios. Others recommended offering prescribing sessions, courses or workshops, and some suggested integrating prescribing content into pharmacology lectures.
Prescribing should be integrated in the clerkship phase in all the different rotations. There should be dedicated lectures for the management of various conditions. These lectures should cover how the conditions are approached in the clinical setting rather than just the theoretical aspect. It should integrate the proper investigations and detailed management with a focus on medication aspects. Teaching about the medications should include the dosage, interactions, adverse effects and choice of the medication and the relevant differences in the outcome. (a recent graduate)
It is interesting to note that the participants emphasized the significance of both theoretical knowledge and clinical practice when it comes to acquiring prescribing competencies. This perspective reflects a holistic approach to medical education and suggests that a balance between understanding theoretical concepts and gaining hands-on experience in a clinical setting is crucial for developing effective prescribing skills.
I just think that the experience in the hospital is unique in providing us with the confidence to be able to understand why prescriptions are given the way they should be. University lectures are important, but not enough. If there is a way to integrate these two experiences, then prescribing medications would be more efficient. (a year 5 student)
Participants also highlighted the need to facilitate students’ access to educational applications and websites focused on content required for prescribing. An important category which emerged from the student’s responses was related to the need to focus on clinical practice guidelines and formulary of medications commonly used in Qatar within the undergraduate curriculum in CMED. Overall, there was a general sense among the participants that there were areas of improvement in curricular content dedicated to teaching medical students effective and safe prescribing, essential for achieving and mastering prescribing competency.
The prescribing instrument developed in this study was found to have excellent content validity with a Content validity Index CVI/Average of 0.9; exceeding a threshold of 0.7.27 Thus, this indicates that the items of this instrument are representative of the intended construct evaluating prescribing competencies in a medical curriculum.
Discussion
This study provided an overview of medical students’ and recent graduates’ perceptions of the extent to which the medical curriculum prepared them to prescribe safely and effectively. The findings showed that nearly two-thirds of the respondents were confident in their prescribing skills. The majority of the participants were satisfied with the prescribing content taught within the undergraduate medical curriculum at Qatar University, which they believed provided them with the knowledge and skills required for safe and effective prescribing. However, these results conflict with the findings of previous studies from various contexts which reported that most medical students expressed dissatisfaction with their medical curricula in preparing them for effective prescribing.4,28–33 One of these studies is a systematic review, which showed that final year medical students often feel unprepared prescribe as they lack the necessary knowledge and skills to assume such a role.28 The lack of preparedness reported in this review may be due to insufficient learning opportunities available for prescribing, particularly within the medical training phase.28 This finding was also confirmed by a scoping review which revealed that medical students often complained of insufficient prescribing related education and a lack of prescribing opportunities.30 Inadequate preparation for prescribing by medical curricula was also reported by other studies which investigated the perceptions of medical students from the UK, Canada and South Africa.29,31,32
The relatively high confidence level of prescribing competence observed among the respondents in our study might be a result of low self-awareness of their real prescribing capabilities and skills. This was also shown in a scoping review which found that medical students and junior doctors tended to overestimate their prescribing competence as compared to the actual competence assessed objectively through prescribing examinations or through the number of prescribing errors committed.30 A study conducted among final year medical students reported a weak positive correlation between self-confidence in prescribing and objective prescribing competence.34 Nevertheless, students’ self-assessment of their prescribing skills is not a reliable measure of prescribing competence. Surprisingly, one study’s findings suggest that prescribing examinations offered by universities might not be an accurate measure of students’ prescribing skills.32 It shows that medical students tend to perform well in recall questions compared to relational questions requiring analytical thinking and evaluative skills.32 These skills are important in real practice where prescribers have to take individualized patient factors into consideration and assess the efficacy and safety of the medications for each case before prescribing. Therefore, Canadian medical school leaders recommended developing a prescribing competence examination and to make it part of the licensing process in Canada.35
When the participants in this study were asked about the contribution of the different courses taught to the development of their prescribing competencies, history taking and physical examination related content received the highest agreement (86%) among the participants. Diagnostic and clinical investigations of diseases received the second highest agreement rate among the participants (75%), while knowledge of concepts and application of evidence-based medicine was useful according to around 67% of the respondents. Interestingly, only 60.9% reported that pharmacology and clinical management knowledge was useful in developing prescribing skills. This result is surprising, mainly because knowledge of pharmacology and therapeutics is the foundation required for safe and effective prescribing. Thus, the lack of positive response from more than one-third of the respondents about these subjects is intriguing and merits further investigation. However, results of a European study in which medical students expressed their dissatisfaction with the clinical pharmacology and pharmacotherapy content taught to them, indicated that the time dedicated for these subjects was not sufficient.4 Similarly, the majority of medical students and junior doctors from the UK indicated that the amount of the teaching they received in pharmacology, therapeutics and prescribing was limited.33
The responding medical students and recent graduates from CMED reported adequate access to drug information resources such as BNF and UpToDate®, which are useful for obtaining the required information when prescribing either during training or clerkships. The participants indicated that the methods used to deliver prescribing material integrated the practical aspects with the theoretical information. The incorporation of practical prescribing concepts and providing students with opportunities to prescribe during their training is important to help them acquire the essential prescribing skills. Teaching of practical prescribing was also common within British medical schools, often provided using an integrated approach.36 The need for practical prescribing training during undergraduate years was highlighted by medical students in the literature.4 The respondents in our study also believed that the practical experience was essential to develop prescribing competencies. In fact, a previous study reported that students who had written more than 10 prescriptions were less likely to make prescribing errors.4
A substantial proportion (60%) of the medical students and graduates from CMED found that the prescribing content taught to them was similar to real-life cases encountered in clinical practice. The current medical curriculum at QU ensures adequate preparation of medical students for practice. However, around 11% of the participants had an opposite opinion and felt that the prescribing content was unrelated to practice. Furthermore, the distribution of prescribing-related content across the medical curriculum was a potential area of concern among the participants as only 44% believed that the distribution was adequate. This is consistent with a previous study finding in which students addressed this issue and recommended introducing practical prescribing in earlier years.29
While a moderately large proportion of participants reported disagreement with the usefulness of formative feedback in enhancing their prescribing competencies, a majority believed that the formative assessments exemplified and exposed them to the real-world physician’s role as a prescriber. The discrepancy might stem from students undervaluing formative feedback due to its perceived indirect impact on grades, preference for the immediate results of summative assessments, and relevance of formative feedback. Studies in the literature documented a positive improvement in medical students and doctors’ prescribing skills with a reduction in prescribing errors after the provision of formative feedback.37–39
A key finding in our study was a significant association between the participants’ year of study and the perceived effectiveness of the prescribing components of the curriculum. A similar finding was also reported in previous studies where more senior participants (students or graduates) believed that their curricula were useful in preparing them for rational prescribing role.29,33 The higher perceived effectiveness by the graduates might be related to the fact that they were exposed to the entire curriculum at CMED and have enough practical prescribing opportunities. Similarly, higher-level students who had more experiential education experience in clinical practice probably had more opportunities to reflect on the prescribing components taught within the medical curriculum and realize its relevance to practice than their lower-level counterparts.
In their responses to the open-ended questions, the participants identified clinical skills and pharmacology lectures among the most useful components of the program helping them in developing prescribing skills. The participants also highlighted the need to expand the students’ prescribing learning opportunities to include additional practical training sessions. Indeed, medical students and junior doctors need to enhance their pharmacology knowledge as it was previously shown that students’ knowledge of drug interactions and contraindications is often poor and results in the selection of incorrect medications, medication dose and duration or length of therapy.4,30 The participants also stressed on the need to introduce medical students to clinical practice guidelines and frequently used medications in Qatar during the undergraduate training at CMED. Evidence-based clinical practice guidelines provide the best practice recommendations for healthcare providers to ensure the best care possible for their patients.40
The current findings underscore the significant correlation between high levels of prescribing errors among junior providers, as initially highlighted in the introduction. This suggests that the effectiveness of the prescribing curriculum could have important implications for patient safety.41 Understanding how improvements in educational interventions influence prescribing practices and accuracy is critical, as it may directly affect the rates of prescribing errors and subsequent patient harm. This connection reinforces the necessity of continually evaluating and enhancing the prescribing curriculum to mitigate risks associated with junior provider prescribing practices.30,42,43
This study is a valuable addition to the medical education literature in the Arab region, as it assesses medical students’ and graduates’ perception of the prescribing components within the medical curriculum. It developed a new instrument designed for the evaluation of curriculum prescribing components from the perspective of students or graduates. The newly developed instrument is brief and easy to use. The limitations of this study include lack of full assessment of psychometric properties of the study instrument such as construct and criterion validity, due to the limited time available for the study. Therefore, further assessment of its psychometrics is warranted. Although this study is primarily cross-sectional in design and incorporates qualitative analysis of open-ended questions to enrich our understanding of participants’ perspectives on prescribing skills/competencies in medical curriculum, a more robust approach would be a well-designed mixed-methods study. Such a study would employ a coherent philosophical paradigm to effectively integrate both qualitative and quantitative methods. Additionally, a future study could investigate the impact of a structured prescribing curriculum for junior providers on reducing prescribing errors and patient harm. By exploring this relationship, we can better understand how educational interventions might enhance patient safety and reduce adverse outcomes related to prescribing practices.
Conclusion
This study provides insight into the perceptions of senior medical students and recent graduates from Qatar University’s CMED regarding their prescribing competence. It also introduces a new validated instrument assessing prescribing competency among medical students. Overall, the findings reflect a positive outlook and confidence among the students in their prescribing skills. To enhance the development of prescribing competency development through the medical curriculum it is recommended to increase students’ prescribing opportunities both within the college. Additionally, incorporating prescribing content into pharmacology courses and providing dedicated prescribing sessions or workshops is essential. There is also a need for tailoring the curriculum to the local context, emphasizing local guidelines and commonly used medications in Qatar. This insight underscores the importance of contextualized education that aligns with the specific challenges and practices in the country and the region as a whole. Overall, this study offers actionable recommendations for curricular improvement in our college and institutions with similar academic programs. Continuous evaluation and quality improvement based on participants’ feedback will contribute to the ongoing enhancement of prescribing education, ensuring that graduates are well prepared for effective prescribing in professional practice.
Funding
The College of Medicine, QU Health, Qatar University provided open access funding for this paper.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Nayak V, Adiga S, Shenoy S, Holla S. Implementation and assessment of a module to enhance prescribing competency in undergraduate medical students. Med J Armed Forces India. 2021;77:S122–S128. doi:10.1016/j.mjafi.2020.12.025
2. Mikulic M Total drug prescriptions dispensed in the U.S. Available from: https://www.statista.com/statistics/238702/us-total-medical-prescriptions-issued/.
3. Picton C, Loughrey C, Webb A. The need for a prescribing competency framework to address the burden of complex polypharmacy among multiple long-term conditions. Clin Med Lond. 2016;16(5):470–474. doi:10.7861/CLINMEDICINE.16-5-470
4. Brinkman DJ, Tichelaar J, Schutte T, et al. Essential competencies in prescribing: a first European cross-sectional study among 895 final-year medical students. Clin Pharmacol Ther. 2017;101(2):281–289. doi:10.1002/cpt.521
5. Langford NJ, Martin U, Kendall MJ, Ferner RE. Medical errors. Medical schools can teach safe drug prescribing and administration. BMJ. 2001;322(7299):1424.
6. Ross S, Maxwell S. Prescribing and the core curriculum for tomorrow’s doctors: BPS curriculum in clinical pharmacology and prescribing for medical students. Br J Clin Pharmacol. 2012;74(4):644–661. doi:10.1111/J.1365-2125.2012.04186.X
7. Alanazi MA, Tully MP, Lewis PJ. A systematic review of the prevalence and incidence of prescribing errors with high-risk medicines in hospitals. J Clin Pharm Ther. 2016;41(3):239–245. doi:10.1111/JCPT.12389
8. Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet. 2002;359(9315):1373–1378. doi:10.1016/S0140-6736(02)08350-2
9. Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf. 2009;32(5):379–389. doi:10.2165/00002018-200932050-00002/METRICS
10. Omer U, Danopoulos E, Veysey M, Crampton P, Finn G. A rapid review of prescribing education interventions. Med Sci Educ. 2021;31(1):273–289. doi:10.1007/s40670-020-01131-8/Published
11. Ross S, Bond C, Rothnie H, Thomas S, MacLeod MJ. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol. 2009;67(6):629–640. doi:10.1111/J.1365-2125.2008.03330.X
12. Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. 2021;30(2):96–105. doi:10.1136/BMJQS-2019-010206
13. Garbutt JM, DeFer TM, Highstein G, McNaughton C, Milligan P, Fraser VF. Safe prescribing: an educational intervention for medical students. Teach Learn Med. 2006;18(3):244–250. doi:10.1207/S15328015TLM1803_10
14. British Pharmacological Society. Ten principles of good prescribing. Available from: https://www.bps.ac.uk/education-engagement/ambassadors-scheme/support-for-ambassadors/resources-to-support-your-ambassador-activity%E2%80%8B/plain-text-careers-resources/plain-text-careers-resources/ten-principles-of-good-prescribing.
15. Medicine Wise N.. Prescribing Competencies Framework. Embedding Quality Use of Medicines into Practice; 2021.
16. Royal Pharmaceutical Society. A Competency Framework for All Prescribers; 2016.
17. Maxwell SRJ, Coleman JJ, Bollington L, Taylor C, Webb DJ. Prescribing safety assessment 2016: delivery of a national prescribing assessment to 7343 UK final-year medical students. Br J Clin Pharmacol. 2017;83(10):2249–2258. doi:10.1111/bcp.13319
18. Maxwell SRJ, Cameron IT, Webb DJ. Prescribing safety: ensuring that new graduates are prepared. Lancet. 2015;385(9968):579–581. doi:10.1016/S0140-6736(14)62339-4
19. Mucklow J, Bollington L, Maxwell S. Assessing prescribing competence. Br J Clin Pharmacol. 2012;74(4):632–639. doi:10.1111/j.1365-2125.2011.04151.x
20. Harrison C, Hilmer S. The prescribing skills assessment: a step towards safer prescribing. Aust Prescr. 2019;42(5):148–150. doi:10.18773/austprescr.2019.050
21. Abdallah O, Ageeb RA, Hamza W, et al. Evaluating prescribing competencies covered in a Canadian-accredited undergraduate pharmacy program in Qatar: a curriculum mapping process. BMC Med Educ. 2020;20:253. doi:10.1186/s12909-020-02109-1
22. Pluye P, Nha Hong Q. Combining the power of stories and the power of numbers: mixed methods research and mixed studies review. Annu Rev Public Health. 2014;35:29–45. doi:10.1146/annurev-publhealth-032013-182440
23. NPS. Competencies required to prescribe medicines: putting quality use of medicines into practice; 2012. Available from: https://www.nps.org.au/assets/682949fec05647bc-2c0de122631e-Prescribing_Competencies_Framework.pdf.
24. Good practice in prescribing and managing medicines and devices. General Medical Council. Available from: www.gmc-uk.org/guidance.
25. Kleinheksel AJ, Rockich-Winston N, Tawfik H, Wyatt TR. Qualitative research in pharmacy education demystifying content analysis.
26. Bengtsson M. How to plan and perform a qualitative study using content analysis. Nurs Plus Open. 2016;2:8–14. doi:10.1016/j.npls.2016.01.001
27. Gilbert GE, Prion S. Making sense of methods and measurement: lawshe’s content validity index. Clin Simul Nurs. 2016;12(12):530–531. doi:10.1016/j.ecns.2016.08.002
28. Brinkman DJ, Tichelaar J, Graaf S, Otten RHJ, Richir MC, van Agtmael MA. Do final-year medical students have sufficient prescribing competencies? A systematic literature review. Br J Clin Pharmacol. 2018;84(4):615–635. doi:10.1111/bcp.13491
29. Kennedy MB, Haq I, Ferns G, Williams SE, Okorie M. The role of undergraduate teaching, learning and a national prescribing safety assessment in preparation for practical prescribing: UK medical students’ perspective. Br J Clin Pharmacol. 2019;85(10):2390–2398. doi:10.1111/bcp.14058
30. Woit C, Yuksel N, Charrois TL. Competence and confidence with prescribing in pharmacy and medicine: a scoping review. Int J Pharm Pract. 2020;28(4):312–325. doi:10.1111/ijpp.12595
31. Holbrook A, Liu JT, Rieder M, et al. Prescribing competency assessment for Canadian medical students: a pilot evaluation. Can Med Educ J. 2019;10(1):e103–110. doi:10.36834/cmej.61646
32. Moch S. Developing Rational Prescribing Competence in Medical School: An Investigation of the Relation Between Student Perceptions and Examination Performance. 2009.
33. Heaton A, Webb DJ, Maxwell SRJ. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008;66(1):128–134. doi:10.1111/j.1365-2125.2008.03197.x
34. Brinkman DJ, Tichelaar J, Van Agtmael MA, De Vries TPGM, Richir MC. Self-reported confidence in prescribing skills correlates poorly with assessed competence in fourth-year medical students. J Clin Pharmacol. 2015;55(7):825–830. doi:10.1002/jcph.474
35. Liu J, Wong S, Foster G, Holbrook A. Prescribing competency of medical students: national survey of medical education leaders. J Popul Ther Clin Pharmacol. 2018;25(1):e18–e24. doi:10.22374/1710-6222.25.1.2
36. Kennedy MB, Williams SE, Haq I, Okorie M. UK medical students’ perspectives on practical prescribing teaching and learning provisions: a cross-sectional survey. Eur J Clin Pharmacol. 2019;75(10):1451–1458. doi:10.1007/s00228-019-02718-w
37. Lloyd M, Watmough SD, O’Brien SV, Hardy K, Furlong N. Exploring the impact of feedback on prescribing error rates: a pilot study. Int J Clin Pharm. 2017;39(5):1013–1017. doi:10.1007/s11096-017-0503-x
38. Coombes I, Donovan P, Bullock B, Mitchell C, Noble C. Can a novel constructivist theory-informed feedback intervention reduce prescribing errors ? A pre-post study. BMC Med Educ. 2023;23(1). doi:10.1186/s12909-023-04095-6
39. Kalfsvel LS, Peeters LEJ, Hoek K, et al. Does formative assessment help students to acquire prescribing skills? Eur J Clin Pharmacol. 2023;79(4):533–540. doi:10.1007/s00228-023-03456-w
40. Panteli D, Legido-Quigley H, Reichebner C, et al. Clinical practice guidelines as a quality strategy. In: Busse R, Klazinga N, Panteli D, editors. Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies [Internet]. European Observatory on Health Systems and Policies; 2019:233.
41. Green W, Shahzad MW, Wood S, et al. Improving junior doctor medicine prescribing and patient safety: an intervention using personalised, structured, video-enhanced feedback and deliberate practice. Br J Clin Pharmacol. 2020;86(11):2234–2246. doi:10.1111/bcp.14325
42. Bos JM, van den Bemt PMLA, de Smet PAGM, Kramers C. The effect of prescriber education on medication-related patient harm in the hospital: a systematic review. Br J Clin Pharmacol. 2017;83(5):953–961. doi:10.1111/bcp.13200
43. Kamarudin G, Penm J, Chaar B, Moles R. Educational interventions to improve prescribing competency: a systematic review. BMJ Open. 2013;3(8):e003291. doi:10.1136/bmjopen-2013-003291
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

