Back to Journals » Drug Design, Development and Therapy » Volume 19
Edaravone in Digestive Diseases – A Narrative Review
Authors Lei H , Wang M, Huang M , Fu X
Received 11 February 2025
Accepted for publication 5 June 2025
Published 12 June 2025 Volume 2025:19 Pages 5071—5084
DOI https://doi.org/10.2147/DDDT.S522011
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Yan Zhu
Haiyun Lei,* Mingchun Wang,* Ma Huang,* Xiaoyun Fu
Department of Critical Care Medicine, Affiliated Hospital of Zunyi Medical University, Zunyi, Guizhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoyun Fu, Department of Critical Care Medicine, Affiliated Hospital of Zunyi Medical University, Zunyi City, Gui Zhou, People’s Republic of China, Email [email protected]
Abstract: Digestive diseases represent a diverse and complex group of systemic disorders, often marked by intricate pathogenic mechanisms and substantial rates of morbidity, disability, and mortality. While effective therapies exist for certain conditions, such as peptic ulcers, gastrointestinal hemorrhage, and viral hepatitis, many others remain difficult to manage due to their limited treatment options, poor response to current therapies, and multifactorial etiologies. As a result, there is a pressing need to develop novel therapeutic agents that offer greater specificity and improved clinical outcomes. Edaravone, a free radical scavenger widely used in the management of neurological disorders, has demonstrated a favorable safety profile and minimal adverse effects. Recent research has expanded our understanding of Edaravone’s pharmacological actions, revealing its broad therapeutic potential beyond the nervous system. Its capacity to neutralize reactive oxygen species, reduce oxidative stress, suppress inflammation, inhibit apoptosis, modulate immune function, and enhance tissue repair positions it as a promising candidate for treating digestive disorders. This review highlights current advances in the application of Edaravone in digestive disease models and clinical settings, to offer new perspectives for future prevention, therapeutic strategies, and scientific investigation in this field.
Keywords: digestive diseases, edaravone, oxidative stress, inflammation, survival
Introduction
Economic development and improved living standards have led to increased dietary diversity, accompanied by a rise in diseases of the digestive system.1 According to the World Health Organization (WHO), the mortality and disability rates resulting from digestive diseases throughout the world are increasing steadily, placing a heavy economic and financial burden on families and national healthcare systems.2 The causes and underlying mechanisms of these diseases are extremely complex,3–5 and the medical community currently lacks a clear understanding of the etiology and mechanisms associated with most digestive disorders. For many of these conditions, conventional drug treatments are typically limited to symptomatic relief, failing to address the underlying pathology and often associated with serious side effects.6–8 Therefore, the development of more effective therapeutic agents with fewer adverse effects is particularly important in the management of digestive diseases.
Edaravone, 1-phenyl-3-methyl-2-pyrazolin-5-one, is a white or off-white crystalline powder, odorless, readily soluble in methanol, soluble in ethanol and chloroform, slightly soluble in acetonitrile, acetone, and 0.1 mol/L sodium hydroxide, and very slightly soluble in water and 0.1 mol/L hydrochloric acid.9,10 It is usually administered by intravenous infusion, and easily crosses the blood-brain barrier. Currently, Edaravone is used primarily as a first-line clinical drug for neuroprotection. Edaravone was officially marketed in Japan in 2001 and has since been included in the guidelines for stroke treatment in both China and Japan. Furthermore, supported by clinical trial evidence—particularly its demonstrated efficacy in amyotrophic lateral sclerosis—Edaravone has been approved and marketed in multiple countries.11 Moreover, several animal studies have extended the therapeutic potential of Edaravone to other neurological disorders, including cerebral aneurysms, epilepsy, and vascular dementia.12–14 It continues to be used as a first-line brain-protective drug, and has significant efficacy, high safety, and minimal side effects.15 Edaravone is associated with various properties, including antioxidant activity against oxidative stress,16 and antifibrotic,17 anti-inflammatory,18 and anti-apoptotic functions.10 Its therapeutic efficacy in neurological disorders is attributed primarily to its potent pharmacological actions. Its pharmacological effects have led to interest in exploring its therapeutic applications in other diseases. This has led to investigation of the effects of Edaravone on disorders associated with various systems, including the digestive,19 respiratory,20 urinary,21 reproductive,22 circulatory,23 and nervous systems,24 and particularly within the digestive system (Figure 1). Current research suggests that Edaravone possesses substantial therapeutic potential in a range of digestive diseases, including acute liver injury, liver fibrosis, pancreatitis, ischemia-reperfusion (I/R)-induced intestinal injury, inflammatory bowel disease (IBD), digestive system cancer, viral hepatitis, fulminant hepatic failure, and complications related to liver transplantation. To date, research and reviews on Edaravone have primarily focused on its applications in neurological diseases, with no comprehensive review addressing its potential use in the treatment of digestive system disorders. Therefore, we collected all relevant studies on Edaravone in digestive diseases published up to May 2025 from the PubMed and CNKI databases and conducted a comprehensive analysis. This review aims to summarize current research progress on the use of Edaravone in digestive diseases and to offer new insights into its potential roles in the prevention, treatment, and pathophysiological study of digestive system disorders. Table 1 provides a list of studies on Edaravone in different digestive diseases, which will be described in detail later in this review.
 |
Table 1 Studies on Edaravone in Different Digestive Diseases |
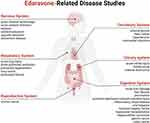 |
Figure 1 Edaravone-Related Disease Research. |
Research Progress on the Use of Edaravone in Digestive Diseases
Edaravone in the Treatment of Acute Liver Injury
Acute liver injury refers to severe damage and death of liver cells. It can be caused by various factors and leads to significant organ dysfunction.82 The primary causes of acute liver injury include infections, chemical toxicity, immune dysfunction, malnutrition, bile duct obstruction, tumors, and genetic factors.83 Acute liver injury can be classified in terms of its etiology into injuries induced by endotoxin, paraquat, ischemia-reperfusion, drugs, and alcohol, as well as damage caused by immune activity and severe acute pancreatitis (Figure 2). Current research has demonstrated the complex pathogenesis of these disorders, involving mechanisms such as inflammation, oxidative stress, and apoptosis of hepatocytes. Therefore, preventing or inhibiting these processes is crucial in mitigating liver damage.
 |
Figure 2 Causes and Classification of Acute Liver Injury. |
Endotoxin-Induced Acute Liver Injury
Clinically, sepsis and post-hepatic surgery can lead to acute liver injury. Infections can lead to an accumulation of reactive oxygen species (ROS), generating large amounts of free radicals and causing oxidative stress. Endotoxins can activate Kupffer cells, leading to the release of eicosanoids and inflammatory mediators, such as tumor necrosis factor-alpha (TNF-α), interleukin-1β (IL-1β), and interferon-gamma (IFN-γ), and cytokine-induced neutrophil chemoattractants (CINCs).84 Thus, oxidative stress and inflammation play vital roles in the progression of liver injury. In a mouse model of acute liver injury induced by D-galactosamine (GalN) and lipopolysaccharide (LPS), Edaravone reduced the levels of inflammatory markers (TNF-α, IL-6) and the activity of caspase-3, decreased hepatocyte apoptosis, improved liver function, and reduced mortality. These findings suggest that Edaravone may mitigate GalN/LPS-induced liver injury by reducing cellular inflammation and inhibiting apoptosis.25 Similarly, in a rat model of acute liver injury induced by GalN/LPS, Edaravone was found to significantly reduce the levels of the antioxidant enzyme heme oxygenase-1 and myeloperoxidase, as well as alleviate oxidative stress, prevent inflammatory cell infiltration, and lower the production of pro-inflammatory cytokines (TNF-α, IL-6), leading to a decrease in liver enzyme levels and reduced mortality.26 In a rat model of endotoxin-induced acute liver injury after partial hepatectomy, Edaravone not only alleviated inflammation induced by liver damage by inhibiting the activation of NF-κB but also suppressed oxidative stress in the liver, significantly reducing postoperative mortality.27
Paraquat-Induced Acute Liver Injury
Paraquat (PQ) is a widely used herbicide, known for its rapid non-selective action and high toxicity. Paraquat poisoning is associated with a high fatality rate after ingestion by humans or animals and can cause damage to various organs, especially the liver.85,86 Paraquat induces substantial oxidative stress87,88 and inflammation89 in the liver. A retrospective analysis of 44 cases of paraquat poisoning revealed that patients treated with Edaravone showed a notable increase in serum superoxide dismutase (SOD) levels, accompanied by significant reductions in inflammatory cytokines (IL-6, IL-10, TNF-α), malondialdehyde (MDA), and liver transaminases, compared to untreated individuals. These results suggest that Edaravone mitigates paraquat-induced hepatotoxicity by reducing oxidative stress and suppressing inflammatory responses.28 An early study also showed that in a mouse model of PQ-induced pulmonary injury, Edaravone markedly reduced liver damage and increased survival rates.29
Ischemia-Reperfusion Liver Injury
Ischemia-reperfusion (I/R) liver injury can occur during liver surgery, hypovolemia, or after liver transplantation. During liver I/R, large amounts of ROS are generated, leading to oxidative stress and exacerbating hepatocyte damage.90,91 Therefore, preventing or inhibiting oxidative stress during liver I/R injury is critical. In a study of liver I/R injury induced by the Pringle maneuver, Edaravone significantly reduced the activities of myeloperoxidase and serum transaminases, as well as the levels of pro-inflammatory cytokines such as IL-6. It also reduced inflammatory cell infiltration, thus increasing survival rates in experimental animals.30 Edaravone treatment also reduced lipid peroxidation in the liver and the leakage of liver enzymes, as well as the levels of pro-inflammatory cytokines, such as TNF-α, and the adhesion molecule E-selectin.31 In a rat model of liver I/R, Edaravone was found to improve blood flow in the portal vein, reduce the levels of liver enzymes in the perfusion fluid, and decrease histological changes and MDA concentrations, thereby mitigating hepatocyte injury.32 In both in vivo and in vitro liver I/R experiments, Edaravone was shown to lower elevated aspartate aminotransferase (AST) levels in liver cells, thus preserving hepatocyte ATP levels. In vivo, Edaravone reduced AST levels in rat sera, decreased the amount of phosphatidylcholine hydroperoxide (PCOOH) in the liver, and restored the energy balance. In conclusion, Edaravone effectively scavenges superoxide species in liver cells and mitigates oxidative liver damage during surgery.33 Studies have also shown that Edaravone can influence the release of inflammatory factors (TNF-α, IL-1β) by modulating the activities of the microRNA PC-3p-190-42101 in plasma exosomes, thereby protecting the liver from I/R injury.19 Liver I/R is associated with oxidative damage to the mitochondria; however, Edaravone can alleviate mitochondrial structural damage and protect against oxidative stress in the organelle, thus improving energy metabolism in the liver. Additionally, Edaravone can normalize levels of pro-inflammatory cytokines, alleviate leukocyte infiltration, and reduce liver lipid peroxidation caused by I/R.34 Additional studies have indicated that Edaravone reduces the levels of free radicals induced by I/R-associated liver injury, thus preventing organ damage by limiting the harmful effects of free radicals.35
Drug-Induced Liver Injury
Drug-induced liver injury (DILI) occurs during the metabolism of drugs in the liver through the cytochrome P450 system, resulting in the formation of toxic metabolites, such as electrophilic groups, free radicals, and oxygen species. These toxic metabolites can interfere with cellular metabolism, disrupt the integrity of cell membranes, and ultimately lead to the death of hepatocytes.92 The severity of DILI is often dose-dependent. When Edaravone enters the body, it is converted into its anionic form, which can donate an electron to oxygen free radicals, thus neutralizing these species and mitigating their potential damage. Additionally, Edaravone can increase the activity of the antioxidant enzyme SOD, increasing antioxidant defenses. It also inhibits inflammatory responses and reduces the release of pro-inflammatory cytokines.36 In a study by Huang et al, using a mouse model of acetaminophen-induced DILI, it was observed that Edaravone reduced the serum levels of alanine aminotransferase (ALT) and the pro-inflammatory IL-6, while increasing the levels of the anti-inflammatory cytokine IL-2. It also reduced lipid peroxide (LPO) and MDA concentrations in liver tissue, enhanced SOD activity, prevented hepatocyte degeneration, and reduced inflammatory cell infiltration, thereby alleviating liver necrosis.37 In a rat model of acute liver injury induced by carbon tetrachloride (CCl4), Edaravone significantly lowered the serum levels of ALT, lactate dehydrogenase (LDH), and total bilirubin (TB), reduced hepatic steatosis, and markedly reduced hepatocyte apoptosis.38 These findings suggest that Edaravone exerts a protective effect against DILI, potentially through mechanisms involving its antioxidant and anti-apoptotic properties, immune modulation, and inhibition of inflammatory responses.
Alcoholic Liver Injury
Approximately 90% of ethanol is metabolized in the liver, and chronic or excessive alcohol consumption leads to progressive liver damage. The metabolism of ethanol induces oxidative stress in the liver and reduces the antioxidant capacity of the cells.93 The induction of apoptosis in hepatocytes is a major contributor to the development of alcoholic liver injury, with ethanol triggering lipid peroxidation and inducing apoptosis.94 The pro-inflammatory cytokine, TNF-α, plays a key role in liver cell necrosis and is associated with the development of alcoholic liver injury. It generates a positive feedback loop with ROS intermediates, stimulating the production of other inflammatory factors, promoting neutrophil infiltration, and triggering lipid peroxidation, while also activating caspases to induce apoptosis.95,96 Edaravone can protect against alcoholic liver injury by the alleviation of oxidative stress and the scavenging of free radicals in liver cells. It also reduces ethanol-induced hepatocyte apoptosis by inhibiting the Caspase-3 pathway. Additionally, Edaravone alleviates the inflammatory response by lowering TNF-α production and reduces Caspase-3-induced apoptosis.39
Immune-Mediated Liver Injury
Immune-mediated liver injury is associated particularly with viral infections. Concanavalin A (ConA) can induce lipid peroxidation in hepatocyte membranes and promote the generation of ROS, leading to structural damage, dysfunction, degeneration, and necrosis in hepatocytes, and causing acute immune-mediated liver injury.97 SOD is an important antioxidant enzyme that protects liver organelles from free radical damage, while MDA is a toxic byproduct of lipid metabolism. The levels of glutathione (GSH) are also a reflection of the body’s antioxidant capacity; decreased GSH concentrations are indicative of reduced antioxidative defense and increased generation of free radicals.98,99 In a study by Chen et al, Edaravone was found to raise the levels of SOD in the liver, as well as reducing the production of MDA, increasing GSH, and alleviating lipid peroxidation in a mouse model of immune-mediated liver injury, thereby mitigating liver damage caused by oxidative stress. These results suggest that Edaravone protects against immune-mediated liver injury by enhancing the body’s antioxidant capacity and shielding liver organelles from damage caused by free radicals.40
Liver Injury Induced by Severe Acute Pancreatitis
Severe acute pancreatitis (SAP) is not only a pancreatic disease but also a systemic syndrome that involves damage to various organs, including the liver, kidneys, lungs, and brain.100 The liver, as the body’s metabolic center, plays a crucial role in regulating metabolism, detoxification, and the inactivation of cellular inflammatory mediators during SAP progression.100 The liver can neutralize the initiating pro-inflammatory factor TNF-α, which triggers a cascade of inflammatory reactions, leading to systemic inflammation and potentially to the systemic inflammatory response syndrome (SIRS) and multi-organ dysfunction syndrome (MODS).101,102 Liver damage caused by SAP is a complex pathological process associated with multiple factors. Liver injury induced by SAP can result in liver failure, disrupting the detoxification and inflammatory mediator inactivation functions of the organ and leading to widespread inflammation and ultimately MODS. In a study by Zhang et al, rats treated with Edaravone showed significantly lower serum amylase (AMY) levels at all time points compared to rats in the SAP model group. Serum ALT and AST activities were reduced, and pathological changes in the pancreas and liver were alleviated. Edaravone also reduced serum TNF-α, IL-6, and MDA levels, while increasing the levels of SOD. Therefore, it can be concluded that Edaravone protects the liver and pancreas from damage in SAP by scavenging excess ROS, enhancing SOD activity, and alleviating oxidative stress-induced injury to these organs.41
Edaravone in the Treatment of Liver Fibrosis
Liver fibrosis is a common occurrence in various chronic liver diseases and is characterized by excessive deposition of extracellular matrix (ECM) material, the formation of fibrous scars, hepatocyte damage, distortion of liver lobules, and changes in the structures of blood vessels. Ultimately, it may lead to cirrhosis, hepatocellular carcinoma, or liver failure.103 The production of ROS and the consequent generation of lipid peroxidation end products can activate hepatic stellate cells (HSCs), resulting in their proliferation and excessive ECM synthesis while reducing ECM degradation, contributing to the development of liver fibrosis.104 Therefore, damage to DNA caused by excessive ROS production is considered a major contributor to liver injury and fibrosis. In a rat model of dimethylnitrosamine (DMN)-induced cirrhosis, Edaravone was found to inhibit HSC activation, thereby reducing liver fibrosis.42 Edaravone also inhibited the recruitment of monocytes/macrophages and the production of IL-1β in macrophages. Additionally, Edaravone suppressed the production of ROS in macrophages and blocked the NF-κB signaling pathway, thus reducing IL-1β secretion, which in turn prevented HSC activation.43 In a thioacetamide (TAA)-induced model of chronic liver fibrosis, Edaravone reduced ROS production, suppressed the NF-κB pathway, and decreased IL-1β release from macrophages, thereby inhibiting HSC activation and preventing TAA-induced liver fibrosis.44 Furthermore, in a study by Li et al, rats with liver fibrosis induced by CCl4 showed significantly lower levels of MDA and higher SOD activities in the liver following Edaravone treatment, along with a reduction in hydroxyproline (HYP) content in liver tissue, suggesting that Edaravone enhanced ROS clearance and protected hepatocytes from damage caused by lipid peroxidation, thus playing a role in the prevention and treatment of liver fibrosis.45
Edaravone in the Treatment of Pancreatitis
Severe acute pancreatitis (SAP) is a common acute abdomen condition, characterized by rapid onset and progression, numerous complications, and high mortality.105 SAP begins with the production of digestive enzymes in pancreatic acinar cells, leading to cell injury and both local and systemic inflammatory responses.106 Cyclooxygenase-2 (COX-2) is closely involved in SAP development as it is the rate-limiting enzyme that converts arachidonic acid to prostaglandins, promoting inflammation.107 The expression of COX-2 has been found to be positively correlated with pancreatic damage, AMY levels, and the volume of ascitic fluid. In a rat model of SAP, Edaravone treatment significantly reduced COX-2 protein expression in the pancreas, lowered AMY levels, reduced ascitic fluid volumes, and mitigated pathological damage in the pancreas, thereby alleviating pancreatic injury.46 A clinical report involving 31 patients observed that Edaravone significantly relieved abdominal pain, reduced serum and urinary AMY levels, alleviated pancreatic pathology, slowed the development of pancreatitis, and improved patient prognosis and survival rates.47 Additionally, when somatostatin was combined with Edaravone in treating pancreatitis, the effects were even more pronounced, lowering the levels of C-reactive protein (CRP) and increasing the cure rate.48 In a mouse model of SAP, Edaravone was observed to modulate the Toll-like receptor 4 (TLR4)/NF-κB signaling pathway, reduce apoptosis in pancreatic cells, and lower the levels of inflammatory cytokines (IL-6, IL-1β, TNF-α), thus reducing pancreatic damage after SAP.49 In a duodenal loop-induced SAP model, Edaravone treatment blocked increases in the pancreatic wet weight, reduced ascitic fluid volumes, lowered the levels of LPO and serum AMY, and attenuated pancreatic damage.50 Similarly, in rat models of SAP, Edaravone reduced serum AMY levels and MPO activity, prevented neutrophil infiltration, and alleviated pathological damage in the pancreas and lungs. Edaravone also significantly reduced the levels of IL-6, TNF-α, and MDA in the lungs of rats with acute pancreatitis, suggesting that the drug may not only treat acute pancreatitis but also protect against associated lung injury.51 In studies on chronic pancreatitis (CP), Edaravone demonstrated antioxidant, anti-inflammatory, and anti-fibrotic properties, alleviating pathological damage in pancreatic tissue. In a study by Zhou et al, in a dibutyltin dichloride (DBTC)-induced model of CP, Edaravone lowered MDA concentrations, reduced the release of inflammatory cytokines such as transforming growth factor-β (TGF-β), IL-6, and TNF-α, and increased SOD activity, thereby preventing pancreatic fibrosis and the activation of pancreatic stellate cells (PSCs).52
Edaravone in the Treatment of Ischemia-Reperfusion-Induced Intestinal Injury
The intestine represents the largest reservoir of bacteria and endotoxins in the body, with the intestinal mucosa acting as a barrier to prevent the entry of bacteria and endotoxins into the circulation.108 Conditions such as severe infection, trauma, shock, intestinal obstruction, extracorporeal circulation surgery, and small intestinal transplantation can lead to I/R injury in the intestine, resulting in the generation of excessive ROS, and leading to oxidative stress, disruption of the intestinal mucosal barrier, increased vascular permeability, bacterial translocation to the circulation, and the release of inflammatory mediators and apoptotic factors. This cascade of events ultimately leads to systemic inflammation, cytokine storms, MODS, and even death.109–111 In a rat model of intestinal I/R injury, Edaravone was found to reduce ROS production, alleviate mucosal erosion and hemorrhage in the small intestine, and inhibit increases in lumen proteins, hemoglobin, thiobarbituric acid-reactive substances (TBA), and MPO activity. Edaravone also reduced both the mRNA and protein expression of CINC-1, thereby providing protective effects against small intestinal I/R injury.53 A study by Liao et al used an in vitro oxygen-glucose deprivation (OGD) model to induce ischemia-hypoxia damage in crypt epithelial cells in the rat small intestine showed that Edaravone blocked the accumulation of free radicals, thereby preventing damage to membrane lipids, proteins, and nucleic acids, as well as apoptosis.54 In a rat intestinal I/R model, Edaravone reduced the levels of MDA in the serum and intestinal tissues and decreased the activities of antioxidant enzymes such as SOD, thus alleviating damage to the intestinal mucosa.55 In a study by Kang, Edaravone was effective in reducing necrosis in the villi of the small intestine, accompanied by decreased villus shedding, lowered levels of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α), increased production of the anti-inflammatory IL-10, and inhibition of bacterial translocation.56 When octreotide was combined with Edaravone to treat acute pancreatitis, reduced generation of intestinal free radicals, lowered lipid peroxidation, decreased ROS-induced inflammatory oxidative stress, and lowered levels of endotoxins, D-lactic acid, and IL-1β were observed, thus protecting intestinal mucosal function in patients with SAP.57 After acute mesenteric artery thrombosis (ASMAT), intra-arterial administration of Edaravone significantly reduced pathological damage in the intestinal mucosa of rabbits and increased their survival.58,59
Edaravone in the Treatment of Inflammatory Bowel Disease (IBD)
Ulcerative colitis (UC) is closely associated with the production of excessive ROS in the intestinal microenvironment. Disruption of oxidative homeostasis caused by the release of metabolites from epithelial cells generates large amounts of ROS, which can damage structural proteins associated with the epithelia and tight junctions, leading to impairment of the intestinal mucosal barrier.112,113 Damaged intestinal epithelial cells activate the NF-κB pathway by binding to gut bacteria through pattern recognition receptors, which in turn promotes the expression and release of inflammatory cytokines, such as IL-6, TNF-α, and IFN-γ. The release of ROS plays an important role in the pathogenesis of clinical IBDs, such as UC and Crohn’s disease.114 In an experimental rat model of colitis induced by dextran sulfate sodium (DSS), administration of Edaravone at a dose of 20 mg/kg/day was found to markedly suppress ROS production in the intestine, while decreasing mucosal MPO activity, LPO, and serum IL-6 levels, thereby inhibiting UC progression.60,61 Furthermore, Compound injection containing Edaravone significantly reduced the levels of pro-inflammatory cytokines, increased those of anti-inflammatory cytokines, reduced M1 macrophage infiltration, increased M2 macrophage numbers, enhanced the integrity of the intestinal barrier, reduced the disease activity index (DAI), and minimized both weight and colon length loss, thus exhibiting a better anti-inflammatory effect than Edaravone alone.62 Similarly, in an indomethacin-induced rat model of acute Crohn’s disease, Edaravone, functioning as a free radical scavenger, significantly alleviated the severity of mesenteric longitudinal ulcers.63
Edaravone in the Treatment of Digestive System Cancer
Recent studies have revealed that Edaravone shows significant antitumor activity across various digestive system cancer models, showing potential for enhancing the effectiveness of chemotherapy. In vitro investigations have demonstrated that Edaravone can suppress the proliferation and differentiation of hepatocellular carcinoma (HepG2) and gastric cancer (TMK-1) cells by modulating the EGFR signaling pathway and interfering with cell cycle progression.64 In a murine colon cancer model, the combined treatment of Edaravone and irinotecan (CPT-11) led to a notable reduction in tumor volume and pulmonary metastatic foci. This effect is attributed to Edaravone’s ability to neutralize chemotherapy-induced ROS, inhibit NF-κB activation, and induce caspase-3-dependent apoptosis.65,66 Beyond its potent antitumor effects, Edaravone also alleviates various chemotherapy-induced toxicities, such as cardiotoxicity,67 nephrotoxicity,68,69 neurotoxicity,70,71 ototoxicity,72,73 and alopecia,74 significantly reducing the side effects of cancer treatments. Furthermore, Edaravone helps mitigate radiotherapy-induced side effects by inhibiting radiation-triggered apoptosis, preventing the formation of phosphorylated histone H2AX (γH2AX) foci, and reducing the incidence of radiation-induced brain necrosis and oral mucositis.75–78 These collective findings underscore the therapeutic potential of Edaravone in the treatment of digestive system cancer.
Edaravone in the Treatment of Other Digestive System Diseases
There are numerous factors that cause hepatitis, including viral infections, autoimmune abnormalities, and alcohol. Among these, viral hepatitis, resulting from infection by different viruses, is associated with inflammation and necrosis of the liver. During this process, the liver generates large amounts of ROS, which in turn activate hepatic Kupffer cells (CD68+ Kupffer cells).115–117 The targeting of CD68+ Kupffer cells plays an important role in the treatment of viral hepatitis. A study by Yasuda et al encapsulated Edaravone in nanoparticles which were used to treat a mouse model of hepatitis induced by ConA, simulating viral hepatitis. The results showed that Edaravone was distributed rapidly to Kupffer cells in the liver where it scavenged excess ROS, inhibited liver necrosis and oxidative stress, and increased the survival rates of the mice, along with notable improvements in liver function.79 Therefore, Edaravone has the potential for use as a nanoparticle therapy for viral hepatitis due to its redox properties and ability to target Kupffer cells. Moreover, Edaravone has potential therapeutic value for several other diseases of the digestive system. For instance, in a Fas-induced mouse model of fulminant hepatic failure, Edaravone not only reduced serum transaminase levels but also alleviated pathological liver damage. Further mechanistic studies revealed that Edaravone prevented the release of cytochrome c and activation of caspase-3, reducing apoptosis in hepatocytes. The anti-apoptotic mechanism of Edaravone might involve modulation of mitochondrial Bcl-xL and Bax.80 Additionally, Edaravone can inhibit apoptosis in transplanted liver cells, thus increasing the survival of transplanted hepatocytes. Specifically, during hepatocyte transplantation, Edaravone administration was found to significantly reduce the number of TUNEL(+) apoptotic cells in donor livers, increase hepatocyte numbers, and enhance the number of hepatocytes in recipients along with elevated levels of serum albumin.81
Conclusion
Advancements in medical science and technology have led to significant progress in diagnosing and treating digestive diseases. However, these conditions’ complex pathogenesis and diversity, especially in the absence of specific, effective drugs, continue to pose a major challenge in clinical practice. Digestive system disorders often present with similar symptoms, such as abdominal pain and indigestion, highlighting the urgent need for a broad-spectrum, effective therapeutic drug. Edaravone, a widely used clinical treatment, has garnered increasing attention for its potential in managing digestive diseases, owing to its excellent safety profile and consistent therapeutic effects. A wealth of animal studies and preclinical evidence has established the notable therapeutic efficacy of Edaravone in the treatment of various digestive disorders, including acute liver injury, liver fibrosis, pancreatitis, I/R-induced intestinal injury, IBD, digestive system can, viral hepatitis, fulminant hepatic failure, and liver transplantation. These diseases are frequently linked to oxidative stress, and Edaravone, with its strong antioxidant properties, can neutralize excess free radicals, thereby reducing tissue damage, inhibiting inflammation, and promoting tissue repair. Moreover, with its well-established pharmacological mechanisms and excellent safety profile, Edaravone offers promising new insights and potential for clinical applications in the treatment of digestive diseases.
Despite these promising findings, several limitations and challenges in applying Edaravone for treating digestive diseases need further investigation. Firstly, the scope of research needs to be broadened. While Edaravone has demonstrated therapeutic efficacy across a range of digestive disorders and common conditions, there is a notable lack of studies exploring its potential for treating other conditions, such as esophageal disorders, peptic ulcers, biliary diseases, and appendicitis. Therefore, future studies should expand the research scope to explore Edaravone’s therapeutic effects across a broader range of digestive diseases, enhancing its clinical applicability and treatment potential. Furthermore, there is a need to integrate basic and clinical research further. Most studies on Edaravone for digestive disorders have focused on laboratory experiments and small-scale clinical trials, resulting in limited large-scale clinical data. Thus, future research should emphasize combining basic research with clinical studies. Larger, more comprehensive clinical trials are necessary to verify its efficacy across diverse patient populations and investigate its underlying mechanisms. This approach will facilitate the transition of Edaravone from laboratory research to widespread clinical application in digestive diseases. Finally, monitoring and managing potential adverse effects requires further exploration. Although Edaravone is generally regarded as safe, some risks, such as liver and kidney damage and allergic reactions, may still arise.118 Future research should address the potential adverse effects of Edaravone when treating digestive diseases to assess its safety profile further and determine ways to minimize possible adverse reactions through dose adjustments or combination therapies. Finally, the potential of Edaravone as a targeted therapy remains largely unexplored. Future research should focus on strategies to enhance its targeting capabilities, such as leveraging nanotechnology to deliver Edaravone to affected areas, thereby improving its therapeutic efficacy.
In conclusion, Edaravone is a clinically recognized drug with a well-established safety profile and a broad range of pharmacological effects. Moreover, it demonstrates considerable promise in treating digestive disorders. With continued exploration of its underlying mechanisms and the advancement of novel drug delivery systems, Edaravone has the potential to become a cornerstone therapy for a variety of digestive diseases.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the National Natural Science Foundation of China (grant number: 82160362).
Disclosure
All authors declare that they have no known conflicts of interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Bultman SJ. Interplay between diet, gut microbiota, epigenetic events, and colorectal cancer. Mol Nutr Food Res. 2017;61(1). doi:10.1002/mnfr.201500902
2. Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: update 2018. Gastroenterology. 2019;156(1):254–272.e211. doi:10.1053/j.gastro.2018.08.063
3. Morgan WL. Diseases of the Digestive Organs, as the Primary Causes of Consumption and of Many Other Diseases. Homoeopath Physician. 1893;13(3):130–137.
4. Castro RE, Rodrigues CMP. Cell Death and microRNAs in Cholestatic Liver Diseases: update on Potential Therapeutic Applications. Curr Drug Targets. 2017;18(8):921–931. doi:10.2174/1389450116666151019102358
5. Tee Yu HH, Tsang S, Cheung TT. An unusual cause of acute abdomen-Gas-forming liver abscess due to Salmonella enteritidis. Asian J Surg. 2017;40(1):66–69. doi:10.1016/j.asjsur.2013.07.014
6. Hindryckx P, Levesque BG, Holvoet T, et al. Disease activity indices in coeliac disease: systematic review and recommendations for clinical trials. Gut. 2018;67(1):61–69. doi:10.1136/gutjnl-2016-312762
7. Kotze PG, Yamamoto T, Damiao A. Postoperative Approach for Crohn’s Disease: the Right Therapy to the Right Patient. Curr Drug Targets. 2018;19(7):729–739. doi:10.2174/1389450116666151102094922
8. Jee SL, Jarmin R, Lim KF, Raman K. Outcomes of early versus delayed cholecystectomy in patients with mild to moderate acute biliary pancreatitis: a randomized prospective study. Asian J Surg. 2018;41(1):47–54. doi:10.1016/j.asjsur.2016.07.010
9. Shakkour Z, Issa H, Ismail H, et al. Drug Repurposing: promises of Edaravone Target Drug in Traumatic Brain Injury. Curr Med Chem. 2021;28(12):2369–2391. doi:10.2174/0929867327666200812221022
10. Ding Y, Zhu W, Li T, Zou P, Chen H, Chen H. Edaravone attenuates neuronal apoptosis in hippocampus of rat traumatic brain injury model via activation of BDNF/TrkB signaling pathway. Arch Med Sci. 2021;17(2):514–522. doi:10.5114/aoms.2019.89849
11. Mikuriya S, Takegawa-Araki T, Tamura M. Edaravone mitigates TDP-43 mislocalization in human amyotrophic lateral sclerosis neurons with potential implication of the SIRT1-XBP1 pathway. Free Radic Biol Med. 2025;230:283–293. doi:10.1016/j.freeradbiomed.2025.01.012
12. Aoki T, Nishimura M, Kataoka H, Ishibashi R, Nozaki K, Hashimoto N. Reactive oxygen species modulate growth of cerebral aneurysms: a study using the free radical scavenger edaravone and p47phox(-/-) mice. Lab investigat. 2009;89(7):730–741. doi:10.1038/labinvest.2009.36
13. Qiu W, Chen R, Pan L, et al. Edaravone dexborneol exerts anti-epileptic effects on rodent temporal lobe epilepsy by promoting NMDAR deactivation and inhibiting oxidative stress. Phytomedicine. 2025;140:156558. doi:10.1016/j.phymed.2025.156558
14. Guo H, Jia Z, Ma S, Zhang J, Zhang J. Edaravone dexborneol attenuates cognitive impairment in a rat model of vascular dementia by inhibiting hippocampal oxidative stress and inflammatory responses and modulating the NMDA receptor signaling pathway. Brain Res. 2024;1833:148917. doi:10.1016/j.brainres.2024.148917
15. Firuzi O, Miri R, Tavakkoli M, Saso L. Antioxidant therapy: current status and future prospects. Curr Med Chem. 2011;18(25):3871–3888. doi:10.2174/092986711803414368
16. Agresti C, Mechelli R, Olla S, et al. Oxidative Status in Multiple Sclerosis and Off-Targets of Antioxidants: the Case of Edaravone. Curr Med Chem. 2020;27(13):2095–2105. doi:10.2174/0929867326666190124122752
17. Wang S, Lu Z, Xu W, Chen Y, Chen X. Effect of edaravone on oxidative stress and myocardial fibrosis induced by isoproterenol in rats. Nan Fang Yi Ke Da Xue Xue Bao. 2015;35(11):1591–1596.
18. Pan Y, Li W, Feng Y, Xu J, Cao H. Edaravone attenuates experimental asthma in mice through induction of HO-1 and the Keap1/Nrf2 pathway. Exp Ther Med. 2020;19(2):1407–1416. doi:10.3892/etm.2019.8351
19. Fei Y, Shao J, Huang G, et al. Effect of Edaravone on MicroRNA Expression in Exosomes after Hepatic Ischemia-reperfusion Injury. Curr Mol Pharmacol. 2022;15(6):870–882. doi:10.2174/1874467214666211130162152
20. Huang M, Mo Y, Lei H, Chen M. Edaravone: a Possible Treatment for Acute Lung Injury. Int J Gen Med. 2024;17:3975–3986. doi:10.2147/ijgm.S467891
21. Yamamura M, Miyamoto Y, Mitsuno M, Tanaka H, Ryomoto M. Edaravone protects against tissue damage in the lung and kidney induced by myonephropathic metabolic syndrome. Int J Angiol. 2010;19(1):e38–40. doi:10.1055/s-0031-1278366
22. Ergenoglu M, Erbaş O, Akdemir A, et al. Attenuation of ischemia/reperfusion-induced ovarian damage in rats: does edaravone offer protection? Eur Surg Res. 2013;51(1–2):21–32. doi:10.1159/000353403
23. Xu H, He K, Li Y, et al. Cytoprotective Effects Evaluation of a Novel Danshensu Derivative DEX-018 against Oxidative Stress Injury in HUVECs. Biol Pharm Bull. 2020;43(5):801–809. doi:10.1248/bpb.b19-00878
24. Kikuchi K, Tancharoen S, Takeshige N, et al. The efficacy of edaravone (radicut), a free radical scavenger, for cardiovascular disease. Int J Mol Sci. 2013;14(7):13909–13930. doi:10.3390/ijms140713909
25. Zong L, Yu QH, Du YX, Deng XM. Edaravone protects endotoxin-induced liver injury by inhibiting apoptosis and reducing proinflammatory cytokines. Braz J Med Biol Res. 2014;47(3):231–236. doi:10.1590/1414-431x20133186
26. Ito K, Ozasa H, Noda Y, Arii S, Horikawa S. Effects of free radical scavenger on acute liver injury induced by d -galactosamine and lipopolysaccharide in rats. Hepatol Res. 2008;38(2):194–201. doi:10.1111/j.1872-034X.2007.00252.x
27. Tsuji K, Kwon AH, Yoshida H, et al. Free radical scavenger (edaravone) prevents endotoxin-induced liver injury after partial hepatectomy in rats. J Hepatol. 2005;42(1):94–101. doi:10.1016/j.jhep.2004.09.018
28. Yi R, Zhizhou Y, Zhaorui S, Wei Z, Xin C, Shinan N. Retrospective study of clinical features and prognosis of edaravone in the treatment of paraquat poisoning. Medicine. 2019;98(19):e15441. doi:10.1097/md.0000000000015441
29. Saibara T, Toda K, Wakatsuki A, Ogawa Y, Ono M, Onishi S. Protective effect of 3-methyl-1-phenyl-2-pyrazolin-5-one, a free radical scavenger, on acute toxicity of paraquat in mice. Toxicol Lett. 2003;143(1):51–54. doi:10.1016/s0378-4274(03)00113-9
30. Hiranuma S, Ito K, Noda Y, Ozasa H, Koike Y, Horikawa S. Amelioration of hepatic ischemia/reperfusion injury in the remnant liver after partial hepatectomy in rats. J Gastroenterol Hepatol. 2007;22(12):2167–2172. doi:10.1111/j.1440-1746.2006.04779.x
31. Taniguchi M, Uchinami M, Doi K, et al. Edaravone reduces ischemia-reperfusion injury mediators in rat liver. J Surg Res. 2007;137(1):69–74. doi:10.1016/j.jss.2006.06.033
32. Ninomiya M, Shimada M, Harada N, et al. Beneficial effect of MCI-186 on hepatic warm ischemia-reperfusion in the rat. Transplantation. 2002;74(10):1470–1472. doi:10.1097/00007890-200211270-00021
33. Abe T, Unno M, Takeuchi H, et al. A new free radical scavenger, edaravone, ameliorates oxidative liver damage due to ischemia-reperfusion in vitro and in vivo. J Gastrointest Surg. 2004;8(5):604–615. doi:10.1016/j.gassur.2004.02.011
34. Okatani Y, Wakatsuki A, Enzan H, Miyahara Y. Edaravone protects against ischemia/reperfusion-induced oxidative damage to mitochondria in rat liver. Eur J Pharmacol. 2003;465(1–2):163–170. doi:10.1016/s0014-2999(03)01463-8
35. Kono H, Woods CG, Maki A, et al. Electron spin resonance and spin trapping technique provide direct evidence that edaravone prevents acute ischemia-reperfusion injury of the liver by limiting free radical-mediated tissue damage. Free Radic Res. 2006;40(6):579–588. doi:10.1080/10715760600606374
36. Nakamoto N, Tada S, Kameyama K, et al. A free radical scavenger, edaravone, attenuates steatosis and cell death via reducing inflammatory cytokine production in rat acute liver injury. Free Radic Res. 2003;37(8):849–859. doi:10.1080/1071576031000136586
37. Huang XG, Bao M, Zhao BF. Study on the Protective Effects of Edaravone on Model Mice with Liver Injury. China Pharm. 2015;26(13):1785–1787.
38. Tada S, Nakamoto N, Kameyama K, et al. Clinical usefulness of edaravone for acute liver injury. J Gastroenterol Hepatol. 2003;18(7):851–857. doi:10.1046/j.1440-1746.2003.03064.x
39. YH Liu, XH Xia, Tang TD, Fu Y. Protective Effect of Edaravone on Hepatocyte Injury Induced by Ethanol. Syst Med. 2018;3(17):20–23. doi:10.19368/j.cnki.2096-1782.2018.17.020
40. Chen FJ, Li J. Role of cytochrome P450 2E1 in edaravone easing oxidative stress in immune liver injury. Chinese Pharmacological Bulletin. 2013;29(02):216–219.
41. Zhang ZJ. Protective effect of edaravone on hepatic injury with severe acute pancreatitis in rats. Jinan University; 2013:1–44.
42. Tanaka H, Ueda H, Fukuchi H, Ichinose M. Antifibrotic effect of edaravone in rat liver cirrhosis induced by dimethylnitrosamine. Clin Exp Med. 2009;9(3):229–233. doi:10.1007/s10238-009-0034-4
43. Zhao R, Zhao H, Guo Q, et al. Edaravone protects against liver fibrosis progression via decreasing the IL-1β secretion of macrophages. Chem Biol Interact. 2022;368:110251. doi:10.1016/j.cbi.2022.110251
44. Zhao RR, Zhang J. The differentiation and maintenance of RORγt+ Tregs respectivelyrequire integrin β8 expression by dendritic cells and commensal microbiota.
45. Li L, Min RQ, Zhan YT, Ma J. Effect of edaravone on lipid peroxidati on in rats with CCl4-induced liver fibrosis. J Pract Hepatol. 2013;16(01):63–65.
46. Li CY, CS Chu, Xu Y, Wang BL. Effect of edaravone on cyclooxygenase-2 expression of pancreatic tissues in severe acute pancreatitis rats. Jiangsu Med J. 2011;37(19):2248–2250+2228. doi:10.19460/j.cnki.0253-3685.2011.19.006
47. Zhang ML. Observation on the Therapeutic Effect of Edaravone in 31 Cases of Acute Pancreatitis. J Changchun Univ Chin Med. 2009;25(03):417. doi:10.13463/j.cnki.cczyy.2009.03.086
48. He JF. Application of edaravone combined with octreotide in patients with pancreatitis and its influence on prognosisHe Jinfang. J Imagi Res Med Appl. 2017;1(17):243–244.
49. Wang B, Lin W. Edaravone Protects against Pancreatic and Intestinal Injury after Acute Pancreatitis via Nuclear Factor-κB Signaling in Mice. Biol Pharm Bull. 2020;43(3):509–515. doi:10.1248/bpb.b19-00944
50. Araki Y, Andoh A, Yokono T, et al. The free radical scavenger edaravone suppresses experimental closed duodenal loop-induced acute pancreatitis in rats. Int J Mol Med. 2003;12(1):121–124.
51. Yang T, Mao YF, Liu SQ, et al. Protective effects of the free radical scavenger edaravone on acute pancreatitis-associated lung injury. Eur J Pharmacol. 2010;630(1–3):152–157. doi:10.1016/j.ejphar.2009.12.025
52. Zhou CH, Lin L, Zhu XY, et al. Protective effects of edaravone on experimental chronic pancreatitis induced by dibutyltin dichloride in rats. Pancreatology. 2013;13(2):125–132. doi:10.1016/j.pan.2013.01.007
53. Tomatsuri N, Yoshida N, Takagi T, et al. Edaravone, a newly developed radical scavenger, protects against ischemia-reperfusion injury of the small intestine in rats. Int J Mol Med. 2004;13(1):105–109.
54. Liao QL, Wang JJ, Li WQ, Ai JN, Wang JL. Therapeutic efficacy of Edaravone on oxygen/glucose deprivation induced rat intestinal epithelial cells damage in vitro. J Dalian Med Univ. 2012;34(04):348–351.
55. Gu SG. Studies on Protective Effects of Edaravone on Intestinal Ischemia-reperfusion Injury in Rats. Shantou University; 2006:1–46.
56. Kang YH. Experimental Study of Edaravone Protects Against Small Intestinal Ischemia-Reperfusion Injury In Rats. Kunming University Of Medical Sciences; 2010:1–40.
57. Zhu XM. Efficacy of edaravone combined with octreotide in treatment of acute pancreatitis and its effect on intestinal mucosal barrier function. Chin J Clin Pharm. 2020;29(03):165–168. doi:10.19577/j.1007-4406.2020.03.002
58. Sonoda A, Nitta N, Seko A, et al. Does the concomitant intra-arterial injection of asialoerythropoietin and edaravone mitigate ischaemic mucosal damage after acute superior mesenteric artery thromboembolism in a rabbit autologous fibrin clot model? Br J Radiol. 2010;83(986):129–132. doi:10.1259/bjr/68683316
59. Sonoda A, Nitta N, Seko A, et al. Edaravone prevents bowel infarction after acute superior mesenteric artery thromboembolism using autologous fibrin clots in a rabbit model. Br J Radiol. 2009;82(981):711–715. doi:10.1259/bjr/13797020
60. Araki Y, Sugihara H, Hattori T. The free radical scavengers edaravone and tempol suppress experimental dextran sulfate sodium-induced colitis in mice. Int J Mol Med. 2006;17(2):331–334.
61. Araki Y, Andoh A, Fujiyama Y. The free radical scavenger edaravone suppresses experimental dextran sulfate sodium-induced colitis in rats. Int J Mol Med. 2003;12(1):125–129.
62. Zhang X, Xu F, Liu L, et al. (+)-Borneol improves the efficacy of edaravone against DSS-induced colitis by promoting M2 macrophages polarization via JAK2-STAT3 signaling pathway. Int Immunopharmacol. 2017;53:1–10. doi:10.1016/j.intimp.2017.10.002
63. Shimizu K, Koga H, Iida M, Haruma K. Microcirculatory changes in experimental mesenteric longitudinal ulcers of the small intestine in rats. Dig Dis Sci. 2007;52(11):3019–3028. doi:10.1007/s10620-007-9804-6
64. Suzuki R, Gopalrao RK, Maeda H, et al. MCI-186 inhibits tumor growth through suppression of EGFR phosphorylation and cell cycle arrest. Anticancer Res. 2005;25(2a):1131–1138.
65. Kokura S, Yoshida N, Sakamoto N, et al. The radical scavenger edaravone enhances the anti-tumor effects of CPT-11 in murine colon cancer by increasing apoptosis via inhibition of NF-kappaB. Cancer Lett. 2005;229(2):223–233. doi:10.1016/j.canlet.2005.06.039
66. Bailly C. Potential use of edaravone to reduce specific side effects of chemo-, radio- and immuno-therapy of cancers. Int Immunopharmacol. 2019;77:105967. doi:10.1016/j.intimp.2019.105967
67. Xin Y, Zhang S, Gu L, et al. Electrocardiographic and biochemical evidence for the cardioprotective effect of antioxidants in acute doxorubicin-induced cardiotoxicity in the beagle dogs. Biol Pharm Bull. 2011;34(10):1523–1526. doi:10.1248/bpb.34.1523
68. Koike N, Sasaki A, Murakami T, Suzuki K. Effect of edaravone against cisplatin-induced chronic renal injury. Drug Chem Toxicol. 2021;44(4):437–446. doi:10.1080/01480545.2019.1604740
69. Williams RM, Shah J, Mercer E, et al. Kidney-Targeted Redox Scavenger Therapy Prevents Cisplatin-Induced Acute Kidney Injury. Front Pharmacol. 2021;12:790913. doi:10.3389/fphar.2021.790913
70. Jangra A, Kwatra M, Singh T, et al. Edaravone alleviates cisplatin-induced neurobehavioral deficits via modulation of oxidative stress and inflammatory mediators in the rat hippocampus. Eur J Pharmacol. 2016;791:51–61. doi:10.1016/j.ejphar.2016.08.003
71. Singh S, Kumar A. Protective Effect of Edaravone on Cyclophosphamide Induced Oxidative Stress and Neurotoxicity in Rats. Curr Drug Safety. 2019;14(3):209–216. doi:10.2174/1574886314666190506100717
72. Im GJ, Chang J, Lee S, et al. Protective role of edaravone against cisplatin-induced ototoxicity in an auditory cell line. Hearing Res. 2015;330(Pt A):113–118. doi:10.1016/j.heares.2015.08.004
73. Domarecka E, Skarzynska M, Szczepek AJ, Hatzopoulos S. Use of zebrafish larvae lateral line to study protection against cisplatin-induced ototoxicity: a scoping review. Int J Immuno Pharmacol. 2020;34:2058738420959554. doi:10.1177/2058738420959554
74. Yoneda K, Fujii M, Imaoka A, et al. Preventive effect of edaravone ointment on cyclophosphamide-chemotherapy induced alopecia. Support Care Cancer. 2021;29(10):6127–6134. doi:10.1007/s00520-021-06189-7
75. Sasano N, Enomoto A, Hosoi Y, et al. Free radical scavenger edaravone suppresses x-ray-induced apoptosis through p53 inhibition in MOLT-4 cells. J Radiat Res. 2007;48(6):495–503. doi:10.1269/jrr.07061
76. Hong Z, Kase Y, Moritake T, et al. Lineal energy-based evaluation of oxidative DNA damage induced by proton beams and X-rays. Int J Radiat Biol. 2013;89(1):36–43. doi:10.3109/09553002.2012.715791
77. Tang Y, Rong X, Hu W, et al. Effect of edaravone on radiation-induced brain necrosis in patients with nasopharyngeal carcinoma after radiotherapy: a randomized controlled trial. J Neuro-oncol. 2014;120(2):441–447. doi:10.1007/s11060-014-1573-4
78. Nakajima N, Watanabe S, Kiyoi T, Tanaka A, Suemaru K, Araki H. Evaluation of edaravone against radiation-induced oral mucositis in mice. J Pharmacol Sci. 2015;127(3):339–343. doi:10.1016/j.jphs.2015.02.001
79. Yasuda K, Maeda H, Kinoshita R, et al. Encapsulation of an Antioxidant in Redox-Sensitive Self-Assembled Albumin Nanoparticles for the Treatment of Hepatitis. ACS Nano. 2023;17(17):16668–16681. doi:10.1021/acsnano.3c02877
80. Miyasou T, Kwon AH, Tsuji K, Qiu Z, Okumura T, Kamiyama Y. Edaravone prevents Fas-induced fulminant hepatic failure in mice by regulating mitochondrial Bcl-xL and Bax. Shock. 2008;30(2):212–216. doi:10.1097/shk.0b013e31816171f4
81. Hayashi C, Ito M, Ito R, et al. Effects of edaravone, a radical scavenger, on hepatocyte transplantation. J Hepatobiliary Pancreat Sci. 2014;21(12):919–924. doi:10.1002/jhbp.164
82. Gunderson A, Said A. Liver disease in kidney transplant recipients. Transplant Rev. 2015;29(1):1–7. doi:10.1016/j.trre.2014.08.002
83. Navarro VJ, Khan I, Björnsson E, Seeff LB, Serrano J, Hoofnagle JH. Liver injury from herbal and dietary supplements. Hepatology. 2017;65(1):363–373. doi:10.1002/hep.28813
84. Okada K, Marubayashi S, Fukuma K, Yamada K, Dohi K. Effect of the 21-aminosteroid on nuclear factor-kappa B activation of Kupffer cells in endotoxin shock. Surgery. 2000;127(1):79–86. doi:10.1067/msy.2000.102425
85. Cassar M, Issa AR, Riemensperger T, et al. A dopamine receptor contributes to paraquat-induced neurotoxicity in Drosophila. Hum Mol Genet. 2015;24(1):197–212. doi:10.1093/hmg/ddu430
86. He F, Zhou A, Feng S, Li Y, Liu T, Papaccio G. Mesenchymal stem cell therapy for paraquat poisoning: a systematic review and meta-analysis of preclinical studies. PLoS One. 2018;13(3):e0194748. doi:10.1371/journal.pone.0194748
87. Pang YW, Jiang XL, Wang YC, et al. Melatonin protects against paraquat-induced damage during in vitro maturation of bovine oocytes. J Pineal Res. 2019;66(1):e12532. doi:10.1111/jpi.12532
88. Huang M, Liu X, Ren Y, et al. Quercetin: a Flavonoid with Potential for Treating Acute Lung Injury. Drug Des Devel Ther. 2024;18:5709–5728. doi:10.2147/dddt.S499037
89. de Oliveira MR, de Souza ICC, Fürstenau CR. Carnosic Acid Induces Anti-Inflammatory Effects in Paraquat-Treated SH-SY5Y Cells Through a Mechanism Involving a Crosstalk Between the Nrf2/HO-1 Axis and NF-κB. Mol Neurobiol. 2018;55(1):890–897. doi:10.1007/s12035-017-0389-6
90. Sabet Sarvestani F, Azarpira N, Al-Abdullah IH, Tamaddon A-M. Tamaddon AM. microRNAs in liver and kidney ischemia reperfusion injury: insight to improve transplantation outcome. Biomed Pharmacother. 2021;133:110944. doi:10.1016/j.biopha.2020.110944
91. Riveros S, Marino C, Ochoa G, et al. Customized normothermic machine perfusion decreases ischemia-reperfusion injury compared with static cold storage in a porcine model of liver transplantation. Artif Organs. 2023;47(1):148–159. doi:10.1111/aor.14390
92. Wang ZH. A Case Analysis of Acute Drug-Induced Liver Injury Caused by Edaravone. J Mudanjiang Med Univ. 2019;40(01):91–92. doi:10.13799/j.cnki.mdjyxyxb.2019.01.032
93. Heslin KC, Elixhauser A, Steiner CA. Identifying in-patient costs attributable to the clinical sequelae and comorbidities of alcoholic liver disease in a national hospital database. Addiction. 2017;112(5):782–791. doi:10.1111/add.13702
94. Ceni E, Mello T, Galli A. Pathogenesis of alcoholic liver disease: role of oxidative metabolism. World J Gastroenterol. 2014;20(47):17756–17772. doi:10.3748/wjg.v20.i47.17756
95. Fernández A, Colell A, Garcia-Ruiz C, Fernandez-Checa JC. Cholesterol and sphingolipids in alcohol-induced liver injury. J Gastroenterol Hepatol. 2008;23(Suppl 1):S9–15. doi:10.1111/j.1440-1746.2007.05280.x
96. Zakaria S, Abass SA, Abdelatty M, Said S, Elsebaey S. Aescin ameliorates alcohol-induced liver injury. A possible implication of ROS / TNF-alpha / p38MAPK / caspase-3 signaling. Food Chem Toxicol. 2025;197:115270. doi:10.1016/j.fct.2025.115270
97. Ni HM, Chen X, Ding WX, Schuchmann M, Yin XM. Differential roles of JNK in ConA/GalN and ConA-induced liver injury in mice. Am J Pathol. 2008;173(4):962–972. doi:10.2353/ajpath.2008.080358
98. Ji HJ, Zhou L, Chen NH. Neuroprotective effects of edaravone against oxidative stress on sodium nitroprusside-induced PC12 cells. Chinese Pharmacological Bulletin. 2011;27:1201–1204. doi:10.3969/j.issn.1001-1978.2011.09.005
99. Llacuna L, Marí M, Lluis JM, García-Ruiz C, Fernández-Checa JC, Morales A. Reactive oxygen species mediate liver injury through parenchymal nuclear factor-kappaB inactivation in prolonged ischemia/reperfusion. Am J Pathol. 2009;174(5):1776–1785. doi:10.2353/ajpath.2009.080857
100. Sha H, Ma Q, Jha RK. Trypsin is the culprit of multiple organ injury with severe acute pancreatitis. Med Hypotheses. 2009;72(2):180–182. doi:10.1016/j.mehy.2008.09.007
101. Gloor B, Müller CA, Worni M, Martignoni ME, Uhl W, Büchler MW. Late mortality in patients with severe acute pancreatitis. Br J Surg. 2001;88(7):975–979. doi:10.1046/j.0007-1323.2001.01813.x
102. Grewal HP, Kotb M, El Din AM, et al. Induction of tumor necrosis factor in severe acute pancreatitis and its subsequent reduction after hepatic passage. Surgery. 1994;115(2):213–221.
103. Caligiuri A, Gentilini A, Pastore M, Gitto S, Marra F. Cellular and Molecular Mechanisms Underlying Liver Fibrosis Regression. Cells. 2021;10(10):2759. doi:10.3390/cells10102759
104. Tomita K, Teratani T, Suzuki T, et al. Free cholesterol accumulation in hepatic stellate cells: mechanism of liver fibrosis aggravation in nonalcoholic steatohepatitis in mice. Hepatology. 2014;59(1):154–169. doi:10.1002/hep.26604
105. Carroll JK, Herrick B, Gipson T, Lee SP. Acute pancreatitis: diagnosis, prognosis, and treatment. Am Fam Physician. 2007;75(10):1513–1520.
106. Bhatia M, Wong FL, Cao Y, et al. Pathophysiology of acute pancreatitis. Pancreatology. 2005;5(2–3):132–144. doi:10.1159/000085265
107. Warzecha Z, Dembiński A, Ceranowicz P, et al. Inhibition of cyclooxygenase-2 reduces the protective effect of hepatocyte growth factor in experimental pancreatitis. Eur J Pharmacol. 2004;486(1):107–119. doi:10.1016/j.ejphar.2003.12.015
108. Tomas J, Reygner J, Mayeur C, et al. Early colonizing Escherichia coli elicits remodeling of rat colonic epithelium shifting toward a new homeostatic state. Isme J. 2015;9(1):46–58. doi:10.1038/ismej.2014.111
109. Lashgari NA, Roudsari NM, Momtaz S, et al. Targeting Mammalian Target of Rapamycin: prospects for the Treatment of Inflammatory Bowel Diseases. Curr Med Chem. 2021;28(8):1605–1624. doi:10.2174/0929867327666200504081503
110. Jia Y, Cui R, Wang C, et al. Metformin protects against intestinal ischemia-reperfusion injury and cell pyroptosis via TXNIP-NLRP3-GSDMD pathway. Redox Biol. 2020;32:101534. doi:10.1016/j.redox.2020.101534
111. Deng F, Lin ZB, Sun QS, et al. The role of intestinal microbiota and its metabolites in intestinal and extraintestinal organ injury induced by intestinal ischemia reperfusion injury. Int J Biol Sci. 2022;18(10):3981–3992. doi:10.7150/ijbs.71491
112. Sahu KK, Minz S, Kaurav M, Pandey RS. Proteins and peptides: the need to improve them as promising therapeutics for ulcerative colitis. Artif Cells Nanomed Biotechnol. 2016;44(2):642–653. doi:10.3109/21691401.2014.975239
113. Dong K, Dong Y, You C, et al. Assessment of the drug loading, in vitro and in vivo release behavior of novel pH-sensitive hydrogel. Drug Deliv. 2016;23(1):174–184. doi:10.3109/10717544.2014.908329
114. Kamba A, Lee IA, Mizoguchi E. Potential association between TLR4 and chitinase 3-like 1 (CHI3L1/YKL-40) signaling on colonic epithelial cells in inflammatory bowel disease and colitis-associated cancer. Curr Mol Med. 2013;13(7):1110–1121. doi:10.2174/1566524011313070006
115. Nakashima H, Kinoshita M, Nakashima M, et al. Superoxide produced by Kupffer cells is an essential effector in concanavalin A-induced hepatitis in mice. Hepatology. 2008;48(6):1979–1988. doi:10.1002/hep.22561
116. Adachi Y, Bradford BU, Gao W, Bojes HK, Thurman RG. Inactivation of Kupffer cells prevents early alcohol-induced liver injury. Hepatology. 1994;20(2):453–460. doi:10.1002/hep.1840200227
117. Kinoshita M, Uchida T, Sato A, et al. Characterization of two F4/80-positive Kupffer cell subsets by their function and phenotype in mice. J Hepatol. 2010;53(5):903–910. doi:10.1016/j.jhep.2010.04.037
118. Liang LR, Wang QY. Analysis of hepatic damage with edaravone. Chin J Clin Ration Drug Use. 2012;5(20):109. doi:10.15887/j.cnki.13-1389/r.2012.20.114
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Platelet-Activating Factor Promotes the Development of Non-Alcoholic Fatty Liver Disease
Yin H, Shi A, Wu J
Diabetes, Metabolic Syndrome and Obesity 2022, 15:2003-2030
Published Date: 8 July 2022
Sacubitril/Valsartan Improves Progression of Early Diabetic Nephropathy in Rats Through Inhibition of NLRP3 Inflammasome Pathway
Pan Y, Liu L, Yang H, Chen W, Chen Z, Xu J
Diabetes, Metabolic Syndrome and Obesity 2022, 15:2479-2488
Published Date: 13 August 2022
Atractylone Alleviates Ethanol-Induced Gastric Ulcer in Rat with Altered Gut Microbiota and Metabolites
Li L, Du Y, Wang Y, He N, Wang B, Zhang T
Journal of Inflammation Research 2022, 15:4709-4723
Published Date: 16 August 2022
Effects of Semaglutide on Cardiac Protein Expression and Cardiac Function of Obese Mice
Pan X, Yue L, Ban J, Ren L, Chen S
Journal of Inflammation Research 2022, 15:6409-6425
Published Date: 24 November 2022
The Effects and Pathogenesis of PM2.5 and Its Components on Chronic Obstructive Pulmonary Disease

Wang Q, Liu S
International Journal of Chronic Obstructive Pulmonary Disease 2023, 18:493-506
Published Date: 6 April 2023

