Back to Journals » Infection and Drug Resistance » Volume 17
Gram-Negative Bloodstream Infections in a Medical Intensive Care Unit: Epidemiology, Antibiotic Susceptibilities, and Risk Factors for in-Hospital Death
Received 27 August 2024
Accepted for publication 12 November 2024
Published 19 November 2024 Volume 2024:17 Pages 5087—5096
DOI https://doi.org/10.2147/IDR.S493267
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Guo Long,1,2 Peng Peng,3 Yuanming Li4
1Department of Respiratory and Critical Care Medicine, The Third Xiangya Hospital of Central South University, Changsha, People’s Republic of China; 2Nursing Department, The Third Xiangya Hospital, Central South University, Changsha, Hunan, People’s Republic of China; 3Clinical Laboratory Medicine Center, The Xiangya Hospital Zhuzhou of Central South University, Zhuzhou, People’s Republic of China; 4Department of Nephrology, The Third Xiangya Hospital of Central South University, Changsha, People’s Republic of China
Correspondence: Yuanming Li, Department of Nephrology, The Third Xiangya Hospital of Central South University, Changsha, 410013, People’s Republic of China, Tel/fax +86 731 8861 8301, Email [email protected]
Purpose: Gram-negative bloodstream infection (GNBI) poses a serious threat to critically ill patients. This retrospective study aimed to uncover drug resistance of pathogens and the GNBI effect on in-hospital death and distinguish death risk factors in a medical intensive care unit (ICU).
Patients and Methods: A retrospective study of all GNBI patients in the medical ICU of the Third Xiangya Hospital over 9 nine years was conducted. Blood samples were performed by a BACTEC 9240 system, MALDI-TOF MS, Bruker and Vitek-2 system. Logistic regression was used for analyzing risk factors for death.
Results: Seventy-five episodes of GNBI developed in 68 (1.4%) out of 4954 patients over a span of 9 years. The most frequently isolated bacterium was Klebsiella pneumoniae, with the lungs as the predominant source of GNBI. The resistance rate of Gram-negative bacteria to polymyxin B was 11.6% after excluding those intrinsically resistant non-fermentative bacteria. All Enterobacter spp. were susceptible to ceftazidime/avibactam. Thirty-three (48.5%) patients underwent inappropriate empirical antibiotic treatment and 48 (70.6%) patients died during the hospitalization. Multivariate logistic regression analysis identified that lymphocyte count at GNBI onset ≤ 0.5× 109/L, invasive mechanical ventilation, and septic shock were related to in-hospital death. Body mass index ≥ 23 and appropriate empirical antibiotic use after GNBI were negatively associated with in-hospital death.
Conclusion: GNBI was a frequent complication among patients in the medical ICU. This study underscored the presence of diverse factors that either heightened or attenuated the risk of in-hospital death.
Keywords: gram-negative bloodstream infections, antimicrobial susceptibility, risk factors, death, medical intensive care unit
Introduction
Despite progress in antibiotic treatment and other supportive care, bloodstream infections remain a significant threat to hospitalized patients, with an annual incidence of 204 cases per 100,000 individuals and a mortality rate ranging from 15% to 60%.1,2 A multi-center study in 162 intensive care units (ICUs) from 24 countries suggested that most episodes of bloodstream infections were caused by multi-drug-resistant (MDR) Gram-negative bacteria.3 An evaluation of Gram-negative bloodstream infections (GNBI) in Qatar highlighted that MDR GNBI was responsible for 13% of all GNBI episodes.4 Patients with bloodstream infections due to Gram-negative bacteria, particularly MDR strains, face limited treatment choices and a significant risk of death, complications, and longer hospital stays.5 A study involved 831 cases of healthcare-associated GNBI from 17 ICUs in Turkey uncovered that the all-cause mortality rate in GNBI patients exceeds 40%.6
The mortality determinants of patients with GNBI have been studied previously in different patients.7–16 Kalam et al conducted a prospective cohort study in Pakistan and found MDR GNBI, multiple positive cultures and a longer stay in ICU (>48 hours) were identified as significant risk factors for 2 week-mortality.9 The predictors for 28 day- or 30 day- mortality included previous hospitalization11 and ICU stay,13 liver cirrhosis,11 pulmonary infection,13 coronary artery disease,7 the incomplete remission status of underlying diseases,14 elevated body mass index (BMI),10 higher lymphocyte,13 lower platelet count,13 hypoproteinemia,14 immune suppression7 and central venous catheter use.15 Charlson comorbidity index,15 high acute physiology and chronic health evaluation II score,11 and higher sequential organ failure assessment score at GNBI onset8,15 also contributed to mortality. MDR bacteremia, including carbapenem-resistant ones,14,15 complicated GNBI,15 positive follow-up blood cultures,15,16 shock,13–15 as well as inappropriate antimicrobial therapy7,11,15 were also risk factors for mortality.
However, in order to investigate the risk factors for late mortality in GNBI patients, Baltas et al conducted a retrospective study of 789 patients with bacteremia due to Escherichia coli, Klebsiella spp. or Pseudomonas aeruginosa from the United Kingdom and revealed that factors correlated with death between one month and one year after detection of GNBI were an adverse antimicrobial resistance profile and infection with P. aeruginosa.12
For the purpose of achieving improved clinical outcomes, it is essential to understand the local epidemiology and antimicrobial resistance patterns in GNBI and explore mortality-related indicators. To our best knowledge, no previous studies focused on antibiotic susceptibility of bacteria causing GNBI and the risk factors for death among patients with GNBI in a medical ICU context. These patients often tend to be older, exhibit more comorbidities, and have compromised immune function compared to those in a general ICU setting, thus potentially facing higher morbidity and mortality rates. Therefore, in this retrospective study performed in a medical ICU setting, the objective was to identify antibiotic resistance profiles and delineate predictors related to death in a cohort of 68 GNBI patients.
Materials and Methods
Study Population
A retrospective study of all GNBI patients in the medical ICU from January 1, 2015, through March 31, 2024, at the Third Xiangya Hospital, which is affiliated to Central South University, was conducted. The patients of aged <18 years and those lost to follow-up were excluded. Among 4954 eligible patients, 68 (1.4%) adult GNBI patients from the medical ICU were analyzed.
Definitions
GNBI was defined as isolating Gram-negative bacilli from equal to or more than one blood culture, and its clinical characteristics were according to systemic inflammatory response syndrome.17 Septic shock was established as sepsis related to hyperlactatemia, persistent hypotension and organ dysfunction, requiring the use of a vasopressor despite adequate fluid resuscitation.18 The source of GNBI was considered after clinical analysis on the basis of clinical records and laboratory findings, conformed with the Centers for Disease Control and Prevention protocol.19 Gram-negative bacterium was considered carbapenem-resistant when nonsusceptible to at least one carbapenem (imipenem, meropenem, or doripenem).20 Appropriate antibiotic therapy was defined when antimicrobial treatment regimens included at least 1 drug displaying in vitro activity within 2 days following the collection of blood culture samples and when the route and dosage of the antibiotics given consistent with current medical criteria.11
Microbiologic Studies
The blood samples were carried out for clinical bacteria culture. All patients received blood cultures when an abnormal body temperature occurred. A 10-mL blood sample was drawn, processed using culture bottles with aerobic and anaerobic medium, and cultured in the BACTEC 9240 system (Becton Dickinson, Cockeysville, MD, USA). MALDI-TOF MS, Bruker and Vitek-2 system (bioMérieux, Marcyl’Etoile, France) were used for the identification and resistance tests of culture-positive cases. To test the antibiotic resistant of bacteria, the minimum inhibitory concentration and Kerby-Bauer disk diffusion method were performed. The results were evaluated according to the CLSI standards.21 Intermediate antimicrobial susceptibility was considered resistance. For multiple GNBI patients with the same bacterium, only the first GNBI episode was analyzed.
The Data Collection
From the computerized microbiology laboratory database and the patient’s medical records, we retrieved demographics, comorbid conditions, antimicrobial use, laboratory and radiographic results, clinic management, and all other prespecified data possibly related to death for all GNBI patients over 9 years. All patients with GNBI were followed up during hospitalization.
Statistical Analyses
For categorical variables, data are expressed in absolute numbers (proportions); For continuous variables that are not normally distributed, data are expressed as the median (interquartile range [IQR]); For continuous variables of the normal distribution, data are expressed as the mean ± standard deviation. χ2 or Fisher exact tests were used to identify associations between death and clinical findings when appropriate. Predictors for death were investigated using multivariate logistic regression analyses on the basis of forward stepwise selection of variables of P value less than 0.1 in the univariate analysis with an odds ratio (OR) value and a 95% confidence interval (CI). The SPSS software, version 26.0 statistical (SPSS, Inc., Chicago, IL), was used to perform all analyses. The significance for all statistical analyses was set at a two-tailed P-value less than 0.05.
Patient Informed Consent
The committee determined that as this study was retrospective and all included patients remain anonymous, written informed consent from patients was not required for this study.
Results
General Features and Outcomes of Patients with GNBI
From January 1, 2015, to March 31, 2024, 4954 patients were admitted to the medical ICU. Seventy-five episodes of GNBI developed in 68 patients, leading to a total infection rate of 13.7 per 1000 ICU hospitalized patients. The studied population comprised 46 males (67.6%) and 22 females (32.4%), with the mean age and median BMI of 64.6 (±17.6) years and 23.0 (IQR: 21.0–23.0), respectively. Pulmonary infection was the most common comorbidity (91.2%), followed by type 2 diabetes (41.2%), malignancy (20.6%), chronic obstructive pulmonary disease (17.6%), COVID-19 infection (11.8%) and Pneumorrhagia (4.4%). The most common source of GNBI was the lungs (69.1%). Septic shock at the GNBI onset occurred in 56 (82.4%) patients. Appropriate empirical antibiotic treatment after GNBI onset was prescribed in 51.5% of all GNBI patients. A total of 57 patients required invasive mechanical ventilation support, and 18 needed blood purification therapy. The median postoperative duration of hospital and ICU stay was 14.0 (IQR: 7.0–22.8) and 9.5 (IQR: 4.0–16.8) days, respectively. Forty-eight (70.6%) patients died during hospitalization after the GNBI onset. The baseline demographic, clinical, and laboratory variables of these 68 patients with GNBI were detailed in Table 1.
 |
Table 1 Demographic, Laboratory, and Clinical Variables of 68 Patients with GNB in Medical ICU |
Among 75 organisms isolated, the most frequently documented genus was Klebsiella pneumoniae (n = 31), followed by Acinetobacter baumannii (n = 21) (Table 2).
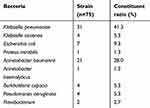 |
Table 2 Classification and Constituent Ratio of Pathogens |
Drug Resistance of Pathogens
High resistance rates of isolates causing GNBI were observed to all antibiotics. The drug resistance rates of cefuroxime, levofloxacin, cefepime, ceftazidime, aztreonam, meropenem, piperacillin/tazobactam, amikacin, cefoperazone/sulbactam, trimethoprim/sulfamethoxazole, and tigecycline ranged from high to low. Among Enterobacter spp., 6 (14.0%) and 21 (48.8%) of 43 bacteria were non-susceptible to polymyxin B and meropenem, respectively, and none to ceftazidime/avibactam. Among non-fermentative bacteria, 8 (25%) and 13 (40.6%) of 32 were resistant to polymyxin B and tigecycline, respectively (Table 3). Six isolates of non-fermentative bacteria, including 4 Burkholderia cepacia and 2 Flavobacterium spp., were intrinsically resistant to polymyxin B. So the resistance rate of Gram-negative bacteria to polymyxin B was 11.6% after excluding those intrinsically resistant non-fermentative bacteria.
 |
Table 3 Rate of Drug-Resistance of Gram-Negative Bacteria to 13 Commonly Used Antibiotics [n(%)] |
Risk Factors Analysis of Patients’ in-Hospital Death
To reveal those potential risk factors for in-hospital death after GNBI onset, the univariate analyse was performed and the results were presented in Table 4. In the univariate analysis, the non-survival group showed a higher prevalence of several factors than that in the survival group. These factors included: Age ≥75 years (P = 0.088), carbapenem-resistant GNBI (P = 0.002), respiratory rates at GNBI onset ≥30 bpm (P = 0.046), white blood cell count at GNBI onset >10×109/L (P = 0.005), lymphocyte count at GNBI onset ≤0.5×109/L (P = 0.001), immune globulin level at GNBI onset <25 g/L (P = 0.014), septic shock at GNBI onset (P = 0.001), methylprednisolone use (P = 0.002), and the requirement for invasive mechanical ventilation (P < 0.001). Conversely, the survival group exhibited a higher ratio of patients with BMI ≥ 23 (P = 0.054) and those receiving appropriate empirical antibiotic treatment after GNBI onset (P = 0.048) than that in the non-survival group.
 |
Table 4 Univariate Analysis of Risk Factors for in-Hospital Mortality After GNB |
Finally, the multivariate analysis identified that lymphocyte count at GNBI onset ≤0.5×109/L [OR = 9.643, 95% CI: 1.685–55.177, P = 0.011], the need for invasive mechanical ventilation support [OR = 19.272, 95% CI: 1.754–211.803, P = 0.016], and septic shock at GNBI onset [OR = 17.476, 95% CI: 1.746–174.911, P = 0.015] were associated with increased odds of in-hospital death. However, BMI ≥ 23 [OR = 0.054, 95% CI: 0.006–0.455, P = 0.007] and appropriate empirical antibiotic treatment after GNBI onset [OR = 0.100, 95% CI: 0.015–0.656, P = 0.016] were related to decreased risk of in-hospital death (see Table 5).
 |
Table 5 Multivariate Logistic Regression Analysis of Risk Factors for in-Hospital Mortality After GNB |
Discussion
CHINET (China Antimicrobial Surveillance Network) and a 20-year study from 45 nations have shown that the most frequent bacteria cultured from blood in major Chinese hospitals were Gram-negative.22,23 E.coli, Acinetobacter spp. and Klebsiella spp. were the most frequent bacteria causing GNBI.24 In the present study, the incidence of GNBI was 1.4%, and the most commonly isolated bacteria causing GNBI were A. baumannii, K. pneumoniae, and E. coli, the same as a previous study from Southern Italy.25
We observed a concerning level of drug resistance among bacteria responsible for GNBI, with notable proportions of A. baumannii and K. pneumoniae exhibiting resistance to commonly used antibiotics. Specifically, 90.5% of A. baumannii and 61.3% of K. pneumoniae were confirmed as carbapenem-resistant, while 12.9% of K. pneumoniae demonstrated resistance to polymyxin B. These findings aligned closely with those reported by Ergönül et al in 2017 (the corresponding rates were 40.0%, 94.0%, and 6.0%, respectively) and Di Carlo et al in 2021 (the corresponding rates were 70.8%, 83.3%, and 15.9%, respectively).6,25
Of note, we found an extremely high in-hospital death (70.6%), similar to a previous case-control study in patients with breakthrough GNBI when carbapenem was being prescribed in Korea with a 70.3% 30-day death rate.26 The elevated death rate identified in our present study can be attributed to several factors. Primarily, our patient cohort exhibited a higher median age (64.6 years), a greater prevalence of comorbidities (91.2% with pulmonary infection, 41.2% with type 2 diabetes), and a predominance of respiratory origin cases (accounting for 69.1% of all GNBI cases). Additionally, a substantial proportion of patients presented with severe drug-resistant conditions (64.4% with carbapenem-resistant GNBI) and received inappropriate empirical antibiotic treatment (accounting for 48.5% of all patients with GNBI). Moreover, a significant majority of patients experienced severe disease manifestations, including the need for invasive mechanical ventilation (83.8%) and septic shock at GNBI onset (82.4%). Furthermore, considering the lower economic status of patients in Hunan Province, China, where our study was conducted, compared to previous studies, socioeconomic factors may have contributed to the observed mortality discrepancy. Importantly, all these aforementioned factors related to increased death rate have been well-established in previous literature among GNBI patients.6,7,11,24,27–29 This present study also differs from some previous studies in that patients in this study were a homogeneous group from a medical ICU; this could have accounted for, at least partially, higher in-hospital mortality in our studied population.
The association of carbapenem-resistant GNBI or COVID-19 infection and mortality has been established.2,14,15,24 However, in our study, we did not observe substantial evidence to support these associations, despite carbapenem-resistant GNBI showing a relationship to in-hospital death in the univariate analysis. The disparities between the current findings and results of previous studies may be owing to variations in the characteristics of the included population and the relatively small sample size of our study cohort.
Septic shock was significantly related to mortality of GNBI patients, which was a finding consistent with the evidence from numerous studies, including our present study.14,15,27 This underscores the severity of illness associated with septic shock, emphasizing the crucial role of early intervention. Clinicians should keep in mind that early treatment, including resuscitation with intravenous fluids and early empiric antibiotic therapy, is necessary to reduce the mortality caused by septic shock.
Sligl et al also found that immune suppression was independently related to 30-day death in patients who suffered from ICU-acquired GNBI.7 In this study, lower lymphocyte count at GNBI onset was found to be linked to in-hospital death. This aligns with the well-established understanding that a lower lymphocyte count reflects compromised cellular immune function. However, it is noteworthy that a higher lymphocyte count was recently identified as an independent predictor of overall survival in GNBI patients with a tumor in another Chinese study conducted by Ni et al.13 To date, there is no data on the association between low lymphocyte counts and mortality in patients with GNBI, and further research is needed.
Our findings are consistent with those published by other authors who observed that a higher BMI is beneficial for survival in critically ill adult patients with sepsis, a phenomenon known as the “obesity paradox”.30,31 Conversely, Lizza et al concluded that a higher BMI in GNBI patients was a risk factors for both organ failure and all-cause death.10 Differences in the study populations between these studies may provide a partial explanation for this disparate finding.
Invasive mechanical ventilation was confirmed to increase the mortality of patients with carbapenem-resistant GNBI or bloodstream infections mainly consisting of GNBI.28,32 Our study also identified an association between invasive mechanical ventilation and mortality among GNBI patients.
Early and appropriate antibiotic administration is essential to the treatment of GNBI patients. Previous studies revealed that inappropriate antimicrobial therapy is a significant risk factor for 30-day death following GNBI.7,11 Likewise, early appropriate therapy was shown to be protective predictors of mortality among patients suffering from A. baumannii- associated bacteremia or carbapenem-resistant GNBI.27,33 Our finding aligns with the results of other studies, indicating that appropriate empirical antibiotic treatment after GNBI onset was related to decreased in-hospital death rate. Thus, the timely use of appropriate antibiotics is critical to minimize patients’ death rate.
Rapid and accurate diagnosis of GNBI is critical because inappropriate initial antibiotic treatment can adversely affect a patient’s prognosis. Therefore, there is a pressing need for swift and precise diagnostic methods to facilitate early antimicrobial therapy guidance and reduce mortality associated with GNBI.34 Clinical diagnosis combined with metagenomic next-generation sequencing (mNGS) was recently recommended to clarify the diagnosis of bloodstream infections and contributed to optimizing antibiotic treatment.35 Zhan et al claimed that routine microbiologic testing frequently falls short of detecting all neuroinvasive pathogens and suggested that mNGS offers an alternative means of detecting nosocomial CNS infections.36 MNGS is a useful complement to conventional diagnostic methods. However, whether mNGS as a diagnostic method is a suitable alternative in routine diagnostics (especially in terms of finances) need more well-designed studies.
Investigating local bacterial epidemiology and drug sensitivity is critical in empirically selecting the right antibiotic. Administration through prolonged infusion is also a pivotal management strategy for optimizing beta-lactam drugs and improving clinical outcomes in patients with GNBI.37 In addition, a system of multidisciplinary management teams was considered to be protective against antibiotic failure in critically ill GNBI patients.38
Similar to other reports, we found that BMI, lymphocyte count, mechanical ventilation, septic shock, and inappropriate antibiotic administration were the significant predictors of in-hospital death in GNBI patients. Therefore, the prognosis of GNBI chiefly rely on patient variables, consisting of the baseline status (normal or lower BMI, lower lymphocyte count), severity of diseases (invasive mechanical ventilation, septic shock at GNBI onset), and management factors (inappropriate antibiotic therapy, the only one that is potentially modifiable).
The potential for bias inherent in single-center observations, retrospective studies, and the small sample size of GNBI and deceased patients are limitations of this study. Nevertheless, the strength of this study lies in its inclusion of GNBI patients over a span of 9 years in a medical ICU, an area that has not been extensively studied previously. In an era characterized by an aging population, the study provided important clinical data on patients from a medical ICU where most of the patients are elders and have more comorbidities with more immunocompromised status than patients in wards or general ICU.
Independent predictors for death revealed in this study each may serve as a reminder to alert clinicians to hospitalized GNBI patients at risk for death. And the investigation of the antibiotic susceptibility profile of bacteria causing GNBI may aid in optimizing antibiotic selection in the future. Future validation through large-scale multicenter prospective studies is warranted.
Conclusions
In summary, despite the limitations mentioned above, we confirmed an increased risk of in-hospital death according to lower lymphocyte count, septic shock at GNBI onset, and the requirement for invasive mechanical ventilation support among GNBI patients, even after adjusting for other risk factors. We also identified that higher BMI and appropriate empirical antimicrobial use were significantly related to good clinical outcomes in the present study. Our findings concerning the risk factors for GNBI hold significant implications for clinical decision-making and patient management within medical ICU settings. Specifically, our findings demonstrate the need for timely identification and management of septic shock, optimizing antibiotic management, increasing nutritional support and immune function support, and robust infection control strategies. These measures are crucial given the unfavorable prognosis associated with GNBI among patients from the medical ICU. We believe that the outcomes of the current research will serve as a guiding beacon for future research endeavors in this field. However, further studies are warranted to identify the findings of the present study.
Ethics Statement
This retrospective study was conducted following approval from the ethics committee of the Third Xiangya hospital of Central South University (ethics number: 24397) under the ethical standards outlined in the Declaration of Helsinki.
Patient Consent
All patient data were anonymized and maintained with strict confidentiality throughout the study to protect privacy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
We declare that we have no conflicts of interest.
References
1. Foglia F, Della Rocca MT, Melardo C, et al. Bloodstream infections and antibiotic resistance patterns: a six-year surveillance study from Southern Italy. Pathog Glob Health. 2023;117(4):381–391. doi:10.1080/20477724.2022.2129161
2. Campos AF, Arantes T, Cambiais AMVB, et al. Impact of an antimicrobial stewardship program intervention associated with the rapid identification of microorganisms by MALDI-TOF and detection of resistance genes in ICU patients with gram-negative bacteremia. Antibiotics. 2022;11(9):1226. doi:10.3390/antibiotics11091226
3. Tabah A, Koulenti D, Laupland K, et al. Characteristics and determinants of outcome of hospital-acquired bloodstream infections in intensive care units: the EUROBACT international cohort Study. Intensive Care Med. 2012;38(12):1930–1945. doi:10.1007/s00134-012-2695-9
4. Abdel Hadi H, Dargham SR, Eltayeb F, et al. Epidemiology, clinical, and microbiological characteristics of multidrug-resistant gram-negative bacteremia in Qatar. Antibiotics. 2024;13(4):320. doi:10.3390/antibiotics13040320
5. Perez KK, Olsen RJ, Musick WL, et al. Integrating rapid diagnostics and antimicrobial stewardship improves outcomes in patients with antibiotic-resistant gram-negative bacteremia. J Infect. 2014;69(3):216–225. doi:10.1016/j.jinf.2014.05.005
6. Ergönül Ö, Aydin M, Azap A, et al. Healthcare-associated gram-negative bloodstream infections: antibiotic resistance and predictors of mortality. J Hosp Infect. 2016;94(4):381–385. doi:10.1016/j.jhin.2016.08.012
7. Sligl WI, Dragan T, Smith SW. Nosocomial gram-negative bacteremia in intensive care: epidemiology, antimicrobial susceptibilities, and outcomes. Int J Infect Dis. 2015;37:129–134. doi:10.1016/j.ijid.2015.06.024
8. Karvouniaris M, Poulakou G, Tsiakos K, et al. ICU-associated gram-negative bloodstream infection: risk factors affecting the outcome following the emergence of colistin-resistant isolates in a Regional Greek hospital. Antibiotics. 2022;11(3):405. doi:10.3390/antibiotics11030405
9. Kalam K, Qamar F, Kumar S, Ali S, Baqi S. Risk factors for carbapenem resistant bacteraemia and mortality due to gram negative bacteraemia in a developing country. J Pak Med Assoc. 2014;64(5):530–536.
10. Lizza BD, Rhodes NJ, Esterly JS, Toy C, Lopez J, Scheetz MH. Impact of body mass index on clinical outcomes in patients with gram-negative bacteria bloodstream infections. J Infect Chemother. 2016;22(10):671–676. doi:10.1016/j.jiac.2016.07.006
11. Zeng Q, Xu F, Jiang S. The impact of previous hospitalization in the preceding 90 days on the outcome in critically ill patients with gram-negative bloodstream infection. Diagn Microbiol Infect Dis. 2014;80(2):136–140. doi:10.1016/j.diagmicrobio.2014.06.015
12. Baltas I, Stockdale T, Tausan M, et al. Long-term outcome and risk factors for late mortality in Gram-negative bacteraemia: a retrospective cohort study. J Glob Antimicrob Resist. 2021;25:187–192. doi:10.1016/j.jgar.2021.03.019
13. Ni S, Xu P, Zhang K, et al. A novel prognostic model for malignant patients with Gram-negative bacteremia based on real-world research. Sci Rep. 2022;12(1):11644. doi:10.1038/s41598-022-15126-5
14. Jian X, Du S, Zhou X, et al. Development and validation of nomograms for predicting the risk probability of carbapenem resistance and 28-day all-cause mortality in gram-negative bacteremia among patients with hematological diseases. Front Cell Infect Microbiol. 2023;12:969117. doi:10.3389/fcimb.2022.969117
15. Giannella M, Pascale R, Pancaldi L, et al. Follow-up blood cultures are associated with improved outcome of patients with gram-negative bloodstream infections: retrospective observational cohort study. Clin Microbiol Infect. 2020;26(7):897–903. doi:10.1016/j.cmi.2020.01.023
16. Kim H, Seo H, Chung H, et al. Bedside risk prediction for positive follow-up blood culture in gram-negative bacilli bacteremia: for whom is follow-up blood culture useful? Infection. 2022;50(3):689–697. doi:10.1007/s15010-021-01742-2
17. Jeon HJ, Kang JM, Koh H, Kim MS, Ihn K. Postoperative bloodstream infection is associated with early vascular complications in pediatric liver transplant recipients with biliary atresia. J Clin Med. 2023;12(21):6760. doi:10.3390/jcm12216760
18. Liu Y, Liu Y, Liu Y, Chen X, Jia Y. Epidemiology, drug resistance analysis and mortality risk factor prediction of gram-negative bacteria infections in patients with allogeneic hematopoietic stem cell transplantation. Heliyon. 2023;9(4):e15285. doi:10.1016/j.heliyon.2023.e15285
19. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi:10.1016/j.ajic.2008.03.002
20. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
21. CLSI. M100 performance standards for antimicrobial susceptibility testing, 34th ed. 2024. Available from: http://em100.edaptivedocs.net/dashboard.aspx.
22. Hu F, Guo Y, Yang Y, et al. Resistance reported from China antimicrobial surveillance network (CHINET) in 2018. Eur J Clin Microbiol Infect Dis. 2019;38(12):2275–2281. doi:10.1007/s10096-019-03673-1
23. Diekema DJ, Hsueh PR, Mendes RE, et al. The microbiology of bloodstream infection: 20-year trends from the SENTRY antimicrobial surveillance program. Antimicrob Agents Chemother. 2019;63(7):e00355–19. doi:10.1128/AAC.00355-19
24. Tabah A, Buetti N, Staiquly Q, et al. Epidemiology and outcomes of hospital-acquired bloodstream infections in intensive care unit patients: the EUROBACT-2 international cohort study. Intensive Care Med. 2023;49(2):178–190. doi:10.1007/s00134-022-06944-2
25. Di Carlo P, Serra N, Lo Sauro S, et al. Epidemiology and pattern of resistance of gram-negative bacteria isolated from blood samples in hospitalized patients: a single center retrospective analysis from Southern Italy. Antibiotics. 2021;10(11):1402. doi:10.3390/antibiotics10111402
26. Lee JY, Kang CI, Ko JH, et al. Clinical features and risk factors for development of breakthrough gram-negative bacteremia during carbapenem therapy. Antimicrob Agents Chemother. 2016;60(11):6673–6678. doi:10.1128/AAC.00984-16
27. Cogliati Dezza F, Covino S, Petrucci F, et al. Risk factors for carbapenem-resistant Acinetobacter baumannii (CRAB) bloodstream infections and related mortality in critically ill patients with CRAB colonization. JAC Antimicrob Resist. 2023;5(4):dlad096. doi:10.1093/jacamr/dlad096
28. Cortes JA, Valderrama-Rios MC, Nocua-Báez LC, Quitián LM, Lozada FA, Buitrago G. Effect of bloodstream infection on survival in COVID-19 patients admitted to an intensive care unit in Colombia: a matched cohort analysis. Infect Prev Pract. 2023;5(2):100283. doi:10.1016/j.infpip.2023.100283
29. Lye DC, Earnest A, Ling ML, et al. The impact of multidrug resistance in healthcare-associated and nosocomial gram-negative bacteraemia on mortality and length of stay: cohort study. Clin Microbiol Infect. 2012;18(5):502–508. doi:10.1111/j.1469-0691.2011.03606.x
30. Li S, Hu X, Xu J, et al. Increased body mass index linked to greater short- and long-term survival in sepsis patients: a retrospective analysis of a large clinical database. Int J Infect Dis. 2019;87:109–116. doi:10.1016/j.ijid.2019.07.018
31. Pepper DJ, Demirkale CY, Sun J, et al. Does obesity protect against death in sepsis? A retrospective cohort study of 55,038 adult patients. Crit Care Med. 2019;47:643–650. doi:10.1097/CCM.0000000000003692
32. Fatima M, Dodani SK, Babar ZU, et al. Outcome, risk factors and therapeutic strategies in carbapenem-resistant gram-negative bacteraemia from Pakistan. JAC Antimicrob Resist. 2023;5(3):dlad076. doi:10.1093/jacamr/dlad076
33. Qu J, Feng C, Li H, Lv X. Antibiotic strategies and clinical outcomes for patients with carbapenem-resistant gram-negative bacterial bloodstream infection. Int J Antimicrob Agents. 2021;57(3):106284. doi:10.1016/j.ijantimicag.2021.106284
34. Zadka H, Raykhshtat E, Uralev B, Bishouty N, Weiss-Meilik A, Adler A. The implementation of rapid microbial identification via MALDI-ToF reduces mortality in gram-negative but not gram-positive bacteremia. Eur J Clin Microbiol Infect Dis. 2019;38(11):2053–2059. doi:10.1007/s10096-019-03640-w
35. Liu Q, Liu X, Hu B, et al. Diagnostic performance and clinical impact of blood metagenomic next-generation sequencing in ICU patients suspected monomicrobial and polymicrobial bloodstream infections. Front Cell Infect Microbiol. 2023;13:1192931. doi:10.3389/fcimb.2023.1192931
36. Zhan L, Lv Z, Zhang Y, et al. Use of metagenomic next-generation sequencing to identify pathogens involved in central nervous system infections. Infect Drug Resist. 2024;17:3605–3615. doi:10.2147/IDR.S474410
37. Tran NN, Mynatt RP, Kaye KS, Zhao JJ, Pogue JM. Clinical outcomes with extended versus intermittent infusion of anti-pseudomonal beta-lactams in patients with gram-negative bacteremia. Open Forum Infect Dis. 2023;10(4):ofad170. doi:10.1093/ofid/ofad170
38. Rinaldi M, Gatti M, Tonetti T, et al. Impact of a multidisciplinary management team on clinical outcome in ICU patients affected by gram-negative bloodstream infections: a pre-post quasi-experimental study. Ann Intensive Care. 2024;14(1):36. doi:10.1186/s13613-024-01271-9
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

