Back to Journals » Advances in Medical Education and Practice » Volume 16
Have We Made Progress? Interprofessional Diversity Within Faculty and Course Directors of Continuous Professional Development Courses Pre- and Post-Joint Accreditation
Authors Ness B , Herndon J , Hoffmann C , Benysh S , Bowler C, Tan W
Received 6 December 2024
Accepted for publication 3 April 2025
Published 15 April 2025 Volume 2025:16 Pages 607—613
DOI https://doi.org/10.2147/AMEP.S509639
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Becky Ness,1,* Justine Herndon,2,* Chelsey Hoffmann,3,* Susan Benysh,4 Carrie Bowler,4 Winston Tan5
1Department of Nephrology and Hypertension, Mayo Clinic Health System Southwest Minnesota, Mankato, MN, USA; 2Department of Medicine, Division of Endocrinology, Mayo Clinic, Rochester, MN, USA; 3Department of Anesthesiology, Division of Pain Medicine, Mayo Clinic, Rochester, MN, USA; 4Mayo Clinic School of Continuous Professional Development, Mayo Clinic, Rochester, MN, USA; 5Department of Hematology and Oncology, Mayo Clinic, Jacksonville, FL, USA
*These authors contributed equally to this work
Correspondence: Becky Ness, Department of Nephrology and Hypertension Mayo Clinic Health System Southwest Minnesota, 1025 Marsh Street, Mankato, MN, 56001, USA, Email [email protected]
Objective: This study aimed to quantify the impact of joint accreditation on the prevalence of physician and non-physician continuous professional development (CPD) course directors(CDs) and faculty.
Methods: CPD CDs and faculty credentials were collected in 2017 (one-year pre-joint accreditation) and 2022 (one-year post-joint accreditation), using electronic and manual data extraction. CPD CDs and faculty were grouped into physician and non-physician cohorts for the quantitative analysis.
Results: A significant increase in the number of non-physician CDs was observed from 2017 (11.3%) to 2022 (22.5%). There were significantly more non-physician faculty at non-physician-focused courses (8.7 ± 8.1 faculty compared to 2.6 ± 4.1 at physician-focused conferences, p = 0.003) with a large effect size, Cohen’s d = − 1.32 [95% CI − 1.8, − 0.9]. Finally, while physicians had statistically higher faculty scores for all three measurements (p < 0.001), the effect sizes were small (Cohen’s d ranging 0.18– 0.20).
Conclusion: Increased diversity in CDs and faculty was noted when comparing pre- and post-joint accreditation suggesting compliance with joint accreditation standards and the growing emphasis on team-based healthcare. Future research is needed to investigate barriers to CPD participation as CDs and faculty for both physician and non-physician healthcare team members. Additional research will continue to help expand diverse professional representation among CDs and faculty within CPD courses.
Keywords: continuing medical education, professional development, leadership, faculty, professional education
Introduction
Research has previously highlighted the lack of diversity in the gender and race of faculty for continuous professional development (CPD) courses.1–10 This problem is prevalent across a wide variety of medical CPD courses targeting both primary care clinicians and subspecialists. While more recently published research has emphasized improvements in the female-to-male faculty ratio within CPD courses, there have been fewer significant strides in improving the racial and ethnic diversity of faculty.2–4
As research builds on the topics of gender, racial, and ethnic diversity of faculty within medical CPD courses, there remains a paucity of available evidence on interprofessional diversity of course directors (CDs) or faculty within CPD courses. Interprofessional diversity, in the context of medical CPD courses, refers to the variety of potential degrees or credentials of participating healthcare providers. All healthcare providers, both physicians and non-physicians, are required to maintain their credentials and licensure by attending CPD courses to receive continuing education credits. As such, interprofessional diversity within CPD courses is extremely important because it allows allcomers to build professional networks, share unique perspectives, collaborate, and disseminate research, work towards academic promotion, and contribute towards innovation.
In 2018, joint accreditation for interprofessional continuing education was introduced to streamline the process of offering continuing education credits to CPD course attendees from various professional backgrounds, while encouraging the team-based healthcare model. This change within CPD courses allowed for a single application process, fee structure, and set of accreditation standards. CPD CDs may seek joint accreditation if the curriculum and course planning committee meet a variety of eligibility requirements, including the demonstration of an integrated planning process involving healthcare professionals from various backgrounds, compliance with the required criteria from any accrediting association, and other requirements.11 Joint accreditation has a specific set of twelve criteria which must be achieved as part of the accreditation process. Each of these criteria emphasizes both the support and education of the healthcare team.11 For example, at least 25% of the educational activities delivered by the organization during the prior 18 months must comprise education designed by and for the healthcare team.11 Additionally, the education must promote active and team-based learning.
No studies have researched the potential impact of joint accreditation on the interprofessional diversity of faculty and CDs within medical CPD courses. More specifically, there is no existing research on the representation of physician and non-physician CDs and faculty within medical CPD courses. Therefore, the authors of this study aimed to accomplish the following objectives:
Methods
This was a retrospective, cross-sectional, quantitative database study with subject information de- identified and presented in aggregate. Prior to study initiation, the study was reviewed by the Mayo Clinic Institutional Review Board (IRB) and determined to be exempt, in accordance with the Code of Federal Regulations, 45 CFR 46.102, thus informed consent was waived.
This quantitative study utilized EthosCE and the Administrative Management Tool (AMT) as the primary data sources. Data were compiled via electronic reports and, where gaps existed, manually extracted by the study authors. The data extraction period included data from 2017 (one-year pre-joint accreditation) and 2022 (one-year post-joint accreditation). These time points were intentionally chosen to investigate the effects of the implementation of joint accreditation on interprofessional diversity within CPD CDs and faculty.
Mayo Clinic CPD courses were eligible to be included in data extraction if they were fully supported by CPD and with live or livestream format. Courses were excluded from the data extraction if they were deployed in any of the following formats: webinars and podcasts.
Extracted data included Mayo Clinic School of Continuous Professional Development (MCSCPD) course co-directors and faculty credentials. No specific sample size goal was set prior to data extraction, as all available data was extracted.
Variables
To address study aims #1 and #2, the dependent variable is the two time periods chosen for the study (2017 and 2022). Independent variables collected included CPD course specialty (nominal data), and CD and faculty profession (nominal data). CD and faculty profession were grouped into the physician group if they had obtained one of the following degrees, which were considered equivalent at the Mayo Clinic: Doctor of Medicine (MD), Doctor of Osteopathic Medicine (DO), Bachelor of Medicine (MBBS), or Bachelor of Medicine-Bachelor of Surgery (MBBCh). Individuals were grouped into the non-physician group if they had obtained one of the following degrees: Doctor of Philosophy (PhD) without other physician degrees, Doctor of Psychology (PsyD), Doctor of Pharmacy (PharmD), Doctor of Nursing Practice (DNP), Certified Nurse Practitioner (CNP), Certified Registered Nurse Anesthetist (CRNA), Physician Assistant (PA), Doctor of Physical Therapy (DPT), Occupational Therapist (OT), Doctor of Occupational Therapy (OTD), Registered Nurse (RN), Master of Science Nursing (MSN), Clinical Nurse Specialist (CNS), and Registered Dietitian Nutritionist (RDN).
To address study, aim #3, the dependent variable was faculty profession (physician vs non-physician), and the independent variables were faculty speaker scores. Faculty speaker scores included three different scores (presentation skills score, presentation practicality score, and overall presentation score). Presentation skills and presentation practicality are rated on a five-point scale (1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent) as rated by attendees of the CPD courses. Overall presentation score is an average of the skills and practicality score. As this data is shared and analyzed in CPD as a mean score, these variables were analyzed as a continuous variable.
Statistical Analyses
Statistical analysis was conducted using BlueSky Statistics v.10.3.4 (BlueSky Statistics, LLC). Categorical data are presented as counts (percentage, %), and chi-square analysis was performed to assess differences between categorical data groups. Continuous data are presented as the mean ± standard deviation. Comparisons between physician and non-physician continuous data were analyzed using an independent t-test, whereas non-physician data from 2017 to 2022 were analyzed using a dependent t-test to see if there was an effect of pre- vs post-accreditation. Effect size was measured as Cohen’s d [95% confidence interval].12 If during the t-tests, Levene’s test of equality was significant (indicating non-normally distributed data), the t-test result of “equal variances not assumed” is presented. However, these analyses were cross-checked using a non-parametric Wilcoxon rank-sum test. Statistical significance was defined as a p-value of < 0.05.
Results
Continuous Professional Development Conference Demographics
There were 45 CPD conferences in 2017 and 167 in 2022 in various specialties (Supplemental Table 1). The number of non-physician-focused courses increased post-accreditation, from 6 (13.3%) in 2017, to 14 (8.4%) in 2022. However, this was not significantly different between years (p = 0.34), Table 1.
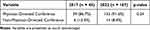 |
Table 1 Comparison of Physician Vs Non-Physician-Focused Continuing Professional Development Courses, Pre- vs Post-Accreditation |
Comparison of Physician vs Non-Physician CDs
A total of 124 CDs were identified for the 2017 CPD courses and 497 for the 2022 CPD courses. The number of non-physician CDs increased significantly post-accreditation, from 14 (11.3%) in 2017 to 112 (22.5%) in 2022 (p = 0.04), Table 2. However, the mean number of non-physician CDs per course was not different between years (mean CD count 1.1 ± 1.7 in 2017 compared to 0.73 ± 1.3 in 2022, p = 0.74).
 |
Table 2 Comparison of Physician Vs Non-Physician Course Directors, Pre- vs Post-Accreditation |
It was more likely that a non-physician CD was part of a non-physician-focused conference, with all (100%) non-physician-focused conferences with a non-physician CD, compared with 35 (20.2%) physician-focused conferences (p<0.001), Table 3.
 |
Table 3 Comparison of Presence of Non-Physician Course Directors, by Continuing Professional Development Course Focus |
Comparison of Physician vs Non-Physician Faculty
In comparing physician- and non-physician-focused courses, there were significantly more non-physician faculty at non-physician-focused conferences (mean faculty count 8.7 ± 8.1 compared to 2.6 ± 4.1 at physician-focused conferences, p = 0.003) with a large effect size (Cohen’s d = −1.32). The Wilcoxon rank-sum test results were also significant (p < 0.001), Table 4.
 |
Table 4 Comparison of Mean Number of Non-Physician Faculty Members, by Continuing Professional Development Course Focus |
The mean number of non-physician faculty per conference per year increased post-accreditation, albeit not significantly (mean non-physician faculty 2.6 ± 4.0 in 2017 vs 3.0 ± 4.1 in 2022, p = 0.45), Table 5. There was also no difference in having non-physician faculties based on the conference specialty (p = 0.09), data not shown.
 |
Table 5 Comparison of Mean Number of Non-Physician Faculty Members, Pre- vs Post-Accreditation |
The faculty scores of the physicians and non-physician faculty were statistically significant in all three scores: average presentation skills score (physician 4.67 ± 0.17 vs non-physician 4.63 ± 0.21, p < 0.001), average presentation practicality score (physician 4.65 ± 0.18 vs non-physician 4.62 ± 0.21, p = 0.001), and average overall presentation score (physician 4.66 ± 0.17 vs non-physician 4.63 ± 0.20, p < 0.001), Table 6. However, the effect size for all these analyses were small (Cohen’s d range 0.18–0.20), Table 6. The Wilcoxon rank-sum test yielded comparable results (Table 6).
 |
Table 6 Comparison of Physician Vs Non-Physician Faculty Scores |
Discussion
Existing research on diversity within healthcare CPD courses has primarily focused on gender, race, and ethnicity within course CDs and faculty.1–10 This study aimed to expand upon existing research by investigating interprofessional diversity, meaning the representation of healthcare team members with varied credentials, within Mayo Clinic CPD courses. Furthermore, the study sought to examine any potential effects on healthcare CPD course CDs and faculty from the 2018 implementation of joint accreditation. Results showed a significant increase in the number of non-physician CDs and faculty within Mayo Clinic CPD courses following the implementation of joint accreditation. Furthermore, there has been a significant increase in the number of CPD courses from 2017 to 2022, suggesting a heightened need for skilled CDs and faculty from varied healthcare disciplines on course planning committees. These findings agree with those published in the Joint Accreditation Data Report of 2021, which showed an increase in both the number of continuing education activities and learner interactions.13 Lastly, this study uncovered a significant difference, though small effect size, in the faculty presenter ratings between physician versus non-physician faculty.
With an increase in both the number of jointly accredited CPD courses and the representation of healthcare credentials amongst CPD course CDs and faculty, there are abundant opportunities for physician and non-physician healthcare team members to collaborate and produce high quality CPD training events. As healthcare teams are expected to deliver optimal care in an increasingly complex, challenging, and uncertain environment, the need for CPD that brings together multiple team members is paramount. Prior to this study, the research highlighting this was conducted primarily by accrediting organizations and participating professional societies.14–17 With the implementation of standardized requirements for joint accreditation of CPD courses, it is necessary that both physicians and non-physicians take on roles as CDs and faculty. Institutions who offer CPD should be aware of the representation of variously credentialed healthcare professionals within the CPD course CDs and faculty. When it is noted that there is inadequate representation from certain healthcare team members, actions should be taken to improve representation.
Supporting and encouraging non-physician team members to participate as CDs and faculty could foster further growth in the interprofessional diversity of CPD courses. To accomplish this, additional research is needed to identify existing barriers to the participation of non-physicians serving as CPD course CDs or faculty. Thereafter, targeted efforts can be made to minimize these hurdles for non-physicians. Potential barriers may include a lack of knowledge regarding CPD or leadership, inadequate mentorship, or a lack of protected administrative time. These barriers could possibly be addressed by adding CPD education or leadership skills training into the didactic portions of educational models, establishing mentorship opportunities within the organizational structure, and offering administration time to allow for participation and contribution as faculty or mentors, or some combination thereof.
Strengths
There is limited data in the current literature on the interprofessional diversity of CPD CDs and faculty. Our study is unique in its review of these data and is an invitation for further investigation in this area. Following the implementation of joint accreditation, there was a significant increase in the number of CPD courses in the comparative model, demonstrating an overall increase in non-physician course deliveries. The concept of team-based care and the integration of non-physicians within the care team create an opportunity for continued growth in the variety and focus of CPD courses. The growth of CPD courses within the Mayo CPD catalog reflects the need to grow and expand CPD educational opportunities directed toward, and inclusive of, all members of the care team.
Limitations
This study was limited by a lack of comparative data in the currently available literature. Our data are limited to one institution for analysis, and only one year before and after joint accreditation.
Future Directions
The limited data surrounding the impact of interprofessional diversity within CPD CDs and faculty creates an abundance of opportunities for further research and review. The inclusion of additional institutions would add to the data landscape and help guide directions for the expansion of reviews. Further investigation could help determine the impact of non-physician CDs in several areas, including course content development, diversity of attendees, attendee satisfaction, and number of conferences offered. Furthermore, the finding of a significant difference in faculty presentation skills between the physician versus non-physician CPD faculty suggests another opportunity for additional research.
Conclusion
This study aimed to investigate the representation of physician and non-physician CPD course CDs and faculty. It additionally aimed to discern whether there were changes in the ratio of physician and non-physician CPD course CDs and faculty with the implementation of joint accreditation in 2018. Findings showed a significant increase in the number of non-physician CDs from 2017 to 2022, following the implementation of joint accreditation. Institutions or organizations offering CPD courses should strive to ensure adequate representation of both physician and non-physician CDs and faculty, in compliance with joint accreditation standards and to continue fostering team-based healthcare. Building off this study, future research should aim to not only uncover existing barriers to healthcare team members participating in CPD courses as CDs and faculty, but to also propose strategies to support these individuals as they work to design highly impactful CPD courses and take on the leadership roles of CPD CDs or faculty. Organizations may consider options such as the implementation of mentorship programs for CPD CDs and faculty or protected administrative time for the planning and execution of CPD courses or events.
Disclosure
Mrs Chelsey Hoffmann reports personal fees from Nalu Medical Inc, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Segarra VA, Primus C, Unguez GA, et al. Scientific societies fostering inclusivity through speaker diversity in annual meeting programming: a call to action. Mol Biol Cell. 2020;31(23):2495–2501. doi:10.1091/mbc.E20-06-0381
2. Goldowsky A, Singh R, Moss A. Speaker diversity and audience ratings at a national inflammatory bowel diseases conference. Inflamm Bowel Dis. 2024;30(1):78–82. doi:10.1093/ibd/izad042
3. D’Souza RS, Pilitsis JG, Langford BJ, et al. Speaker gender representation at the North American Neuromodulation Society Annual Meeting (2017–2021): have we made progress in closing the gender gap? J Pain Res. 2022;15:3423–3432. doi:10.2147/JPR.S380152
4. Ha G, Benyamein P, Reghunathan M, Vatsia S, Blum J, Gosman AA. Racial and ethnic disparities in selected speakers at plastic surgery conferences. Plast Reconstr Surg Glob Open. 2023;11(7):e5157. doi:10.1097/GOX.0000000000005157
5. Arora A, Kaur Y, Dossa F, Nisenbaum R, Little D, Baxter NN. Proportion of female speakers at academic medical conferences across multiple specialties and regions. JAMA Netw Open. 2020;3(9):e2018127. doi:10.1001/jamanetworkopen.2020.18127
6. Carley S, Carden R, Riley R, et al. Are there too few women presenting at emergency medicine conferences? Emerg Med J. 2016;33(10):681–683. doi:10.1136/emermed-2015-205581
7. Schroeder E, Rochford C, Voss M, Gabrysch S. Beyond representation: women at global health conferences. Lancet. 2019;393(10177):1200–1201. doi:10.1016/S0140-6736(18)32854-X
8. Moeschler SM, Gali B, Goyal S, et al. Speaker gender representation at the American Society of Anesthesiology Annual Meeting: 2011–2016. Anesth Analg. 2019;129(1):301–305. doi:10.1213/ANE.0000000000003944
9. Silva N, Cerasiello S, Semonche A, et al. Gender representation at neurological surgery conferences. World Neurosurg. 2019;129:453–459. doi:10.1016/j.wneu.2019.06.062
10. Vivekanantha P, Dao A, Hiemstra L, et al. Gender representation in major orthopaedic surgery meetings: a quantitative analysis. JB JS Open Access. 2023;8(4):
11. Guide to the Joint Accreditation Process. Revised 2023. Available from: https://jointaccreditation.org/wp-content/uploads/2023/02/1014_20230829_guide_for_providers_to_the_joint_accreditation_process.pdf.
12. Cohen J. Statistical Power Analysis for the Behavioral Sciences.
13. Joint Accreditation for Interprofessional Continuing Education. Joint Accreditation data report: driving improvement through Accredited Continuing Education for Healthcare Teams – 2021; 2022.
14. Regnier K, Travlos DV, Pace D, Powell S, Hunt A. Leading change together: supporting collaborative practice through Joint Accreditation for Interprofessional Continuing Education. J Eur CME. 2022;11(1):2146372. PMID: 36408351; PMCID: PMC9673784. doi:10.1080/21614083.2022.2146372
15. Chappell K, Regnier K, Travlos DV. Leading by example: the role of accreditors in promoting interprofessional collaborative practice. J Interprof Care. 2018;32(4):404–406. doi:10.1080/13561820.2018.1433276
16. Regnier K, Chappell K, Travlos DV. The role and rise of interprofessional continuing education. J Med Regulation. 2019;105(3):6–13. doi:10.30770/2572-1852-105.3.6
17. Graebe J, Richetti DA, Zarembski D. Considerations for faculty and presenters in interprofessional continuing education. J Contin Educ Nurs. 2022;53(10):432–435. doi:10.3928/00220124-20220907-02
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

