Back to Journals » Clinical Ophthalmology » Volume 19
Intravitreal Plungerless Injector Device (IPLID): An Innovative Intravitreal Injector Device
Authors Yepez JB, Murati FA, Petitto M, Kozak I, Arevalo JF
Received 5 September 2024
Accepted for publication 24 January 2025
Published 14 February 2025 Volume 2025:19 Pages 535—541
DOI https://doi.org/10.2147/OPTH.S494755
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Juan B Yepez,1 Felipe A Murati,2 Michele Petitto,3 Igor Kozak,4 J Fernando Arevalo5
1Vitreoretinal Surgery Department, Clinica de Ojos, Maracaibo, Venezuela; 2Sotero del Rio, Hospital, Santiago, Chile; 3Glaucoma Department, Clinica de Ojos, Maracaibo, Venezuela; 4Department of Ophthalmology and Vision Science, University of Arizona, Tucson, AZ, USA; 5Retina Division, Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore, MD, USA
Correspondence: J Fernando Arevalo, Retina Division The Wilmer Eye Institute, Johns Hopkins University School of Medicine, 600 N. Wolfe Street, Maumenee 713, Baltimore, MD, 21287, USA, Tel +1 443 287 9554, Fax +1 443 287 5492, Email [email protected]
Purpose: To share our early experience with the novel intravitreal plungerless injector device (IPLID) for application in patients with various retinal diseases.
Patients and Methods: This study enrolled 300 eyes (300 patients) who had undergone at least 1 previous conventional intravitreal injection, for various indications, such as diabetic macular edema, venous occlusions, active choroidal neovascular membrane, wet AMD and neovascular glaucoma. Patients with systemic conditions that could affect pain tolerance were excluded. All patients underwent intravitreal injection with the IPLID. After the procedure the patients were asked to grade pain compared to conventional injections. Immediately after the procedure, surgeons completed a simple survey on various aspects of the device, including safety of the procedure. Data were also collected on the duration of the procedure.
Results: The study sample was comprised of 210 males and 90 females. The mean duration of the injection was 17.51 minutes (range, 15 minutes to 20 minutes). Post-IPLID injection, 155 (51.7%) patients reported less pain compared to previous injections, 128 (42.7) patients reported pain similar to previous injections and 5.7% (17) of patients reported more pain than previous procedures. The physician survey indicated that there was no difference between IPLID and conventional technique in 13.33% (40) of injections, and 86.67% (260) of the injections were comfortable to perform with the IPLID and size was not an issue in 91.67% (275) of injections. In all cases, the surgeons were comfortable with the delivery of medication with IPLID and there were no adverse events during or after IPLID injection.
Conclusion: The IPLID is a simple device for delivering intravitreal injection and may offer greater ergonomic advantages and that address the issue of musculoskeletal disorders in healthcare personnel due to repetitive procedures over time.
Keywords: intravitreal injections, IPLID, hand ergonomics, musculoskeletal disorders
Introduction
The increasing importance of intravitreal injections in ophthalmology has led to an unmet need for effective and safe training methods for healthcare professionals. Delivery of therapeutic agents via intravitreal injections is well established as the mainstay of treatment for many retinal diseases such as diabetic macular edema or macular edema secondary to retinal vein occlusions, polypoidal choroidal vasculopathy, and choroidal neovascularization due to diseases such as age-related macular degeneration (AMD), pathologic myopia, and infectious and inflammatory conditions.1,2 Intravitreal injection is the most common eye procedure worldwide and, in the United States is increasing at 6% per year.3 In the UK, the Royal College of Ophthalmologists predicts a 53% increase from 2015 to 2035.4
With an increasing number of indications, intensive long-term treatment comprised of recurring injections is currently needed to improve visual outcomes. The volume of intravitreal injections is projected to increase due to novel indications and innovative intravitreal agents for retinal diseases.5 Additionally, the exponential increase in disease such as AMD and diabetes globally will further add to the burden of patients requiring injections.5 As a result, the injections are increasingly being delivered either by ophthalmic nurse practitioners, residents or by ophthalmologists in a clinical office-based setting.6 Hence, there is a need to make the procedure more comfortable and safer for both patients and providers. One way to achieve this is via simple drug delivery, sparing stress on the musculoskeletal system.
Innovation in devices for intravitreal injection has been published.4,7–12 However, these mainly refer to improving the injection process, such as making it more efficient in terms of time, safety of the injection position, reducing the risk of infections and pain for the patient. However, little consideration has been given to what is the most ergonomic hand position to perform the procedure.
Occupational injuries such as musculoskeletal disorders (MSD) occur more regularly in healthcare workers than any other careers. MSD commonly occur due to repetitive movements, static or limited body positions, intense force on small parts of the body (eg a hand or wrist). The muscular burden for healthcare personnel executing an intravenous push procedure and other tasks requiring hand force, extended duration, thumb force, and lack of muscular rest, are all repetitive movements related to MSD of the hand.13–18 Ergonomics and hand positioning are crucial in preventing and managing hand strength injuries.19
In other words, exponentially more force would be applied to perform the task with the thumb hyperextended compared to when it is not hyperextended. Ergonomically, during intravitreal procedures a thumb that is not hyperextended results in a lower load for the muscles that perform this task in the hand repetitively and for long periods of time.
In this paper we introduce the intravitreal plungerless injector device (IPLID) that is a small, single-use disposable device, specifically designed for intravitreal injections through a small needle to assist healthcare personnel in the administration of intravitreal injections. We propose that IPLID’s design, which allows a more physiologically neutral hand position and reduces thumb hyperextension, may reduce muscle strain due to repetitive use. The improved ergonomics have the potential to mitigate the risk of MSDs commonly seen among healthcare providers performing high volumes of intravitreal injections. By enabling a pinch-like motion with reduced force requirements, IPLID may help sustain hand comfort and reduce cumulative stress on the musculoskeletal system.
Materials and Methods
As this was an evaluation of a new device, this study adhered to ethical guidelines, including IRB approval and written informed consent from all participants. This study adhered to the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act of 1966. In this trial 300 eyes of 300 patients were enrolled, who had received at least 1 previous intravitreal injection for various indications, such as diabetic macular edema, venous occlusions, active choroidal neovascular membrane, wet AMD and neovascular glaucoma. Patients with systemic conditions that might affect degree of pain were excluded. All patients underwent the procedure at Clinica de Ojos, Maracaibo, Venezuela between January 2019 to July 2023 by 10 different retina specialists, fellows, and residents. All 10 physicians were approached at the outset of the study and were provided with a standardized training session on the IPLID device to ensure familiarity with its design, operation, and proper usage. This training included a demonstration of the device’s features, practical guidance for performing injections, and a review of safety protocols. The goal was to ensure that all participants, regardless of their level of expertise or prior experience with intravitreal injections, could perform the procedure consistently and comfortably using the IPLID device. Feedback from the injection personnel was then systematically collected through a structured survey to evaluate their satisfaction, comfort, and any challenges encountered during the procedure.
Device Description
The IPLID is a small, single-use disposable device, calibrated, pre-filled and sealed disposable collapsible tube, without a rigid tube and piston, that is 8 cm long, especially designed for intravitreal injections through a small needle for aiding healthcare personnel with the procedure (Figure 1).
 |
Figure 1 Schematic of the intravitreal plungerless injector device design. |
The IPLID is akin to a super-glue tube. After breaking the seal, a small needle is connected to the collapsible tube and after penetrating the scleral wall with the needle (30G-030 x 4 mm), the drug (eg antiangiogenic, antibiotic, triamcinolone, etc) is released slowly by flattening the collapsible tube between the thumb, the index, and the middle fingers. This hand position is likely optimal for this function and should be considered, as it may help reduce the risk of MSDs while potentially enhancing the efficiency, safety, and speed of the injection process. By maintaining a neutral wrist position and appropriately hyperextending the thumb, maximum pinch force can be achieved, which is essential for precise and controlled movements during injections. Conversely, improper thumb positioning and increased pinch width may decrease pinch force, potentially leading to strain and repetitive hand injuries.
The most innovative aspect of the IPLID resides in its ergonomic design, a collapsible delivery (without the rigid tube and piston) that brings the index finger closer to the thumb and the middle finger.
Intravitreal Injection
Once the patient was supine, 2–3 drops of topical anesthetic (proparacaine chlorinate 0.5%; Alcon, New York, NY, USA) were instilled in the eye. Five minutes later the patient’s eyelids and periorbital skin were cleansed with 10% povidone iodine solution and a 5% povidone iodine solution was applied to the ocular surface. Following the application of sterile surgical drapes, a standard lid speculum was placed for globe exposure. After 10 minutes topical anesthetics and 5% povidone-iodine were administered into the ocular surface. The withdrawal process of the anti-VEGF agent (bevacizumab 0.05 mL; Genentech, San Francisco, CA, USA) into the IPLID device began with the use of a sterile, 19-gauge filter needle to draw the medication from the vial. This filtration step was critical for the removal of any potential particulate matter, thereby ensuring the purity of the withdrawn solution. Following this step, the filter needle was replaced with a 30-gauge needle suitable for the IPLID injection procedure. The entire process was performed under strict aseptic conditions to maintain drug integrity and patient safety. A pars plana injection was administered at 3.5 mm from the limbus for pseudophakic patients or 4 mm for phakic patients. Distances were marked via scleral indentation with the IPLID marker tip. Following the injection push, the pressure was maintained until the device was removed from the sclera, then a sterile cotton-tip applicator was used to tamponade the injection site to minimize vitreous reflux and hemorrhage (Figure 2). The duration of the procedure was recorded from the time the patient was supine until the needle was removed. Patients were asked to use specific descriptive terms to rate any differences in pain intensity compared to their previous injections as follows: increased, unchanged, or decreased. After each intravitreal injection session, the doctor filled out a simple four-question survey to evaluate: experience using the device, size of the device, safety of the procedure, and the way the medication was delivered, with the options “comfortable”, “uncomfortable”, or “no difference”. Follow up was performed at 1, 14 and 30 days after injection. The evaluation included clinical examination findings, IOP measurements using tonometry, and slit-lamp biomicroscopy to assess anterior chamber inflammation. Fundoscopy was performed to identify signs of retinal detachment or vitreous hemorrhage and patency of central retinal artery.
 |
Figure 2 The sequence shows the application of intravitreal injection with the intravitreal plungerless injector device, using clamp pressure with the fingers to deliver the medication. |
Safety of the procedure was assessed by monitoring for adverse events commonly associated with intravitreal injections, including intraocular pressure (IOP) changes, subconjunctival hemorrhage, retinal detachment, anterior chamber cells/uveitis, and vitreous hemorrhage. Data on these parameters were collected at specified time points, including immediately after the injection, at the 1-hour mark, and during follow-up visits at 1 day, 1 week, and 1 month post-injection.
Results
The mean age of the study sample was 57.19 years (range, 25 years to 87 years). There were 210 males. The mean number of previous injections was 6.46 (range, 2 to 11 injections). The mean duration of the injection was 17.51 minutes (range, 15 minutes to 20 minutes). Figure 3 summarizes the outcomes of patient perception of pain. Following IPLID injections, 155 patients (51.7%) reported experiencing less pain compared to previous procedures, while 128 patients (42.7%) described pain or sensation as being similar to their prior injections. A smaller proportion, 17 patients (5.7%), indicated experiencing more pain than in previous procedures (Figure 3). While these findings offer initial insights into patient-reported outcomes, the lack of a control group and reliance on subjective comparisons to prior injections highlight the need for more rigorous methodologies in future studies to validate these results. The outcomes of the physician survey indicated that in 13.33% (40) of injections there was no difference between conventional and IPLID injections and 86.67% (260) of the injections were comfortable to perform with the IPLID (Table 1). The physicians noted that the IPLID device’s size was not a source of discomfort in 91.67% (275) of injections. Furthermore, the physician consistently found the device’s design and functionality conducive to smooth medication delivery, highlighting its practicality and ease of use during the procedure (Table 1).
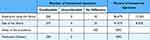 |
Table 1 Physician Experience on Intravitreal Injection With the Intravitreal Plungerless Injector Device |
 |
Figure 3 Patient-reported pain compared to previous standard injection without the intravitreal plungerless injector device. noPx denotes the number of patients; % denotes the percent of patients. |
No adverse events were reported such as awkward posture, high force in the provider’s hand or in the patients’ eyes. There were no reports of endophthalmitis, inflammation, high intraocular pressure. Pressure applied by the surgeon during the injection process was gentle enough and patients had no discomfort or pain immediately after the injection, and most of them did not notice the needle used for the injection.
Discussion
This investigation of intravitreal injection with a novel device indicated that injection times were similar to those reported in previous publications with conventional injections.5 However we believe that intravitreal injections may be delivered faster with the IPLID and here we are reporting our early experience that includes our learning curve with the device. The features of IPLID that may decrease injection times with greater experience include, the marking time with the caliper and the form of delivery of the medication with only digital pressure (without a plunger) can make the procedure more expeditious and possibly optimize the time in the placement of intravitreal injections.
Based on our initial observations, we propose that the IPLID may exhibit novel characteristics, such as shorter medication delivery times, lower patient-reported pain levels measured on the Visual Analog Scale (VAS), and improved satisfaction and safety for healthcare providers. These preliminary insights highlighted the potential of IPLID to address challenges commonly associated with intravitreal injection procedures and demonstrated its feasibility in various clinical scenarios.
In our experience, most patients reported less pain with the IPLID immediately after injection than with previous injections. We believe this is due to the needle size as described above.5 We also found that patients who received more injections reported the same or less pain.
Physician feedback from this study suggests the IPLID was both safe and ergonomically favorable to use, regardless of the injector’s level of experience. However, this assessment is based on subjective evaluations from a single center. Further studies employing validated ergonomic assessment tools (eg standardized MSD questionnaires) are needed to confirm these preliminary observations and quantify ergonomic benefits. One of the key limitations of our study is the absence of a matched control group using conventional injection techniques. Instead, patient-reported outcomes were based on subjective comparisons to their prior injection experiences, which introduces potential recall bias and limits the scientific robustness of the findings. While this method provides valuable real-world insights into patient perceptions, it does not replace the rigor of a randomized, controlled study. Despite these limitations, the consistency in the reported reduction of pain (51.7%) and physician feedback regarding ease of use (86.67%) suggests promising benefits of the IPLID device. These preliminary results provide a foundation for further investigation and highlight the potential of IPLID to improve patient comfort and procedural efficiency in clinical practice.
Our primary goal in this study was to provide preliminary, real-world insights into patient-reported pain perception following IPLID injections. While these findings suggest that 51.7% of patients reported less pain and 42.7% reported similar levels compared to previous procedures, we recognize that subjective self-reports lack the rigor of objective assessments.
The IPLID device’s design likely contributes to a smoother and more controlled injection process, reducing variability in pressure and patient discomfort during medication delivery. Additionally, the stabilization and ergonomic benefits of the IPLID may enhance the surgeon’s control, resulting in a gentler and more consistent experience for the patient. These factors, though not directly related to the needle size, could have influenced the overall perception of pain. These results should be interpreted cautiously and that future studies will require a prospective, randomized design incorporating validated pain assessment tools (eg, Visual Analog Scale) and direct comparisons with conventional injection techniques to ensure scientifically rigorous conclusions.
While the safety profile of the IPLID device was favorable, with no adverse events reported, we recognize that introducing a new device in clinical practice requires thorough safety verification. Future studies with rigorous, controlled designs and long-term follow-up are necessary to confirm the safety and efficacy of this device in larger patient populations.
This novel injector device was designed to simplify, facilitate, decrease operator discomfort, and reduce adverse outcomes by providing a more ergonomic technique for intravitreal injections. Table 2 presents a comparison of the features of conventional intravitreal injection versus IPLID.
 |
Table 2 Characteristics of Intravitreal Plungerless Injector Device and Traditional Syringe Device for Delivering Intravitreal Injection |
Conclusion
The use of the IPLID device is straightforward and shows promise in offering ergonomic advantages and safety during intravitreal injections. Intravitreal injections can be time-intensive and physically demanding for healthcare personnel, raising concerns about musculoskeletal strain as the volume of injections continues to increase. The IPLID device enables a physiologically ergonomic hand position, which could mitigate these risks.
While the IPLID device demonstrates promise in reducing perceived patient discomfort and improving ergonomic positioning during intravitreal injections, these findings are preliminary. Future studies employing objective assessments and prospective, comparative methodologies are needed to validate these observations and confirm its benefits for both patients and healthcare providers.
To the best of our knowledge, this is the first study to explore the ergonomic positioning of the hand during intravitreal injections. While our findings are preliminary and limited by the absence of direct comparative data or objective ergonomic assessments, they provide a foundation for future research. Further studies employing validated tools and robust methodologies are necessary to clarify the potential ergonomic and safety benefits of this device for both healthcare providers and patients.
Funding
There is no funding to report.
Disclosure
Dr. Yepez has financial and proprietary interest in the IPLID. In addition, Dr Yepez reports patents (18/645,488 and 29/939,115) for “syringe design and syringe fo intraocular injection” pending. The other authors do not have any financial or proprietary interest to report for this paper.
References
1. Panos GD, Lakshmanan A, Panagiotis D, Ripa M, Motta L, Amoaku WM. Faricimab: transforming the future of macular diseases treatment - a comprehensive review of clinical studies. Drug Des Devel Ther. 2023;17:2861–2873. doi:10.2147/DDDT.S427416
2. Mushtaq Y, Mushtaq MM, Gatzioufas Z, Ripa M, Motta L, Panos G. Intravitreal Fluocinolone Acetonide Implant (ILUVIEN®) for the treatment of retinal conditions. A review of clinical studies. Drug Des Devel Ther. 2023;17:961–975. doi:10.2147/DDDT.S403259
3. Lam LA, Mehta S, Lad EM, Emerson GG, Jumper JM, Awh CC. Task force on intravitreal injection supplemental services. Intravitreal injection therapy: current techniques and supplemental services. J Vitreoretin Dis. 2021;5(5):438–447. doi:10.1177/24741264211028441
4. Uy HS, Artiaga JCM. Comparison of two different intravitreal injection techniques. Clin Ophthalmol. 2021;15:2383–2389. doi:10.2147/OPTH.S309501
5. Soh YQ, Chiam NPY, Tsai ASH, et al. Intravitreal injection with a conjunctival injection device: a single-center experience. Transl Vis Sci Technol. 2020;9(8):28. doi:10.1167/tvst.9.8.28
6. Simcock P, Kingett B, Mann N, et al. A safety audit of the first 10 000 intravitreal ranibizumab injections performed by nurse practitioners. Eye. 2014;28(10):1161–1164. doi:10.1038/eye.2014.153
7. Ratnarajan G, Nath R, Appaswamy S, Watson SL. Intravitreal injections using a novel conjunctival mould: a comparison with a conventional technique. Br J Ophthalmol. 2013;97(4):395–397. doi:10.1136/bjophthalmol-2012-302155
8. Michelotti MM, Abugreen S, Kelly SP, et al. Transformational change: nurses substituting for ophthalmologists for intravitreal injections - a quality-improvement report. Clin Ophthalmol. 2014;8:755–761. doi:10.2147/OPTH.S59982
9. Han DP, Mckenney KC, Kim JE, Weinberg DV, Musch DC, Singh RS. Clinical evaluation of the rapid access vitreal injection guide: a handheld instrument for assisting intravitreal injections. Retina. 2017;37(4):778–781. doi:10.1097/IAE.0000000000001229
10. Watanabe K, Masafumi U, Mohamed YH, et al. Safety of intravitreal injection guide. J Vitreoretin Dis. 2017;2(1):26–31. doi:10.1177/2474126417728622
11. Eaton AM, Gordon GM, Wafapoor H, Sgarlata A, Avery RL. Assessment of novel guarded needle to increase patient comfort and decrease injection time during intravitreal injection. Ophthalmic Surg Lasers Imaging Retina. 2013;44(6):561–568. doi:10.3928/23258160-20131105-06
12. De Luna D, Netzel A, Dietze J, Begley BA, Ndulue JK, Suh DW. A comparison in precision and accuracy of the conventional syringe to the Suh precision syringe. Clin Ophthalmol. 2019;13:1833–1839. doi:10.2147/OPTH.S211485
13. Gyer G, Michael J, Inklebarger J. Occupational hand injuries: a current review of the prevalence and proposed prevention strategies for physical therapists and similar healthcare professionals. J Integr Med. 2018;16(2):84–89. doi:10.1016/j.joim.2018.02.003
14. Gallagher S, Heberger JR. Examining the interaction of force and repetition on musculoskeletal disorder risk: a systematic literature review. Hum Fact. 2013;55(1):108–124. PMID: 23516797; PMCID: PMC4495348. doi:10.1177/0018720812449648
15. Simonsen JG, Arvidsson I, Nordander C. Ergonomics in the operating room. Work. 2012;41(Suppl 1):5644–5646. doi:10.3233/WOR-2012-0905-5644
16. OSH answers fact sheets work-related musculoskeletal disorders. Available from: https://www.ccohs.ca/oshanswers/diseases/rmirsi.
17. Macdonald V, Keir P. Assessment of musculoskeletal disorder risk with hand and syringe use in chemotherapy nurses and pharmacy assistants. IISE Trans Occup Ergon Hum Factors. 2018;6(3–4):28–142. doi:10.1080/24725838.2018.1502698
18. Eapen C, Bhaskaranand K, Bhat A. Prevalence of cumulative trauma disorders in cell phone users. J Musculoskelet Res. 2010;13:137–145. doi:10.1142/S0218957710002545
19. Horton S, Doumit M, Rockwell G. The ergonomics of syringe operation during the injection of fluid into tissue expanders.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Expert Panel Consensus for Addressing Anti-VEGF Treatment Challenges of Diabetic Macular Edema in Spain
Fernández-Vigo JI, Contreras I, Crespo MJ, Beckford C, Flores-Moreno I, Cobo-Soriano R, Pareja J, Martín MD, Moreno L, Arrevola-Velasco L
Clinical Ophthalmology 2022, 16:3097-3106
Published Date: 19 September 2022
The Economic Burden of Diabetic Retinopathy in Jordan: Cost Analysis and Associated Factors
Al-Dwairi RA, Aleshawi A, Abu-zreig L, Al-Shorman W, Al Beiruti S, Alshami AO, Allouh MZ
ClinicoEconomics and Outcomes Research 2024, 16:161-171
Published Date: 15 March 2024
Faricimab Outcomes in Chorioretinal Disorders: Indian Real-World Analysis (FOCUS Study)
Agrawal V, Gupta A, Agrawal V, Sheth JU
Clinical Ophthalmology 2025, 19:1855-1862
Published Date: 12 June 2025

