Back to Journals » Advances in Medical Education and Practice » Volume 15
Medical Students’ Knowledge and Perceptions of Herbal Medicine in Saudi Arabia: Should Medical Schools Take Immediate Action?
Authors Almech M , Alissa A, Baghdadi RA , Abujamai JZ, Hafiz W , Alwafi H , Shaikhomer M, Alshanberi AM, Alshareef MH , Alsanosi SM
Received 24 September 2024
Accepted for publication 11 December 2024
Published 18 December 2024 Volume 2024:15 Pages 1243—1253
DOI https://doi.org/10.2147/AMEP.S497642
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Majd Almech,1 Abdulrahim Alissa,1 Ragad Adel Baghdadi,2 Jakleen Z Abujamai,1 Waleed Hafiz,3 Hassan Alwafi,4 Mohammed Shaikhomer,5 Asim M Alshanberi,1,6 Maram H Alshareef,6 Safaa M Alsanosi4
1General Medicine Program, Batterjee Medical College, Jeddah, 21442, Saudi Arabia; 2Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia; 3Department of Medicine, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia; 4Department of Pharmacology and Toxicology, Faculty of Medicine, Umm Al Qura University, Makkah, Saudi Arabia; 5Department of Internal Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 6Department of Community Medicine and Pilgrims Health Care, Faculty of Medicine, Umm Al Qura University, Makkah, Saudi Arabia
Correspondence: Safaa M Alsanosi, Email [email protected]
Background: Herbal medicine is integral to Saudi Arabia’s Vision 2030, which seeks to improve the healthcare system and promote alternative practices while ensuring safety through education and research. This study aims to evaluate medical students’ knowledge and perceptions regarding herbal medicine in Saudi Arabia.
Methods: A cross-sectional study was conducted among medical students in three medical colleges in Saudi Arabia over a six-month period from 1 February to 31 July 2024. Descriptive statistics were used to describe the participants’ characteristics, and categorical variables were reported as frequencies and percentages. A chi-square test was used to test the relationships between variables. A p-value of < 0.05 was taken to indicate statistical significance.
Results: In total, 592 participants were included in the study. Females represented 65.7% of the participants. While 72.6% of the students agreed that medical students lack proper knowledge about the use of herbal medicines, 64.9% preferred having an elective course in complementary medicine (including herbal medicine). Also, 40.9% of students use herbal medicine believing they do not require expert knowledge and can safely experiment with various herbs, and 22.3% use it because they perceive it as having no side effects due to its natural ingredients. The most reported sources of information included family and friends (53.2%), whereas traditional herbalists (Attar) were the most reported sources of herbs (49.3%). The most used herbs among medical students were ginger (83%), turmeric (48.1%), chamomile (46.3%), and myrrh (26.5%). Only 37.7% of students who used herbs had an overall good knowledge and perception of them (P = 0.001). Gender showed a significant relationship with herb use among the students: 95.4% of female students used herbs, compared with 92.6% of male students (P = 0.049).
Conclusion: A considerable proportion of medical students demonstrated insufficient knowledge and perception regarding the use of herbal medicine. To improve their understanding, it is essential to integrate comprehensive courses, organize workshops led by experts, promote research and clinical experiences, and establish patient education initiatives.
Keywords: medical students’, herbal medicine, Saudi Arabia, medical schools
Introduction
Herbal medicine encompasses the therapeutic application of plants and plant extracts, a practice with extensive historical foundations across various cultural traditions worldwide.1,2 The core principle of herbal medicine suggests that naturally occurring plant compounds can effectively address many health conditions.3 The recent resurgence of interest in herbal medicine can be attributed to escalating costs of conventional healthcare, the rise of antibiotic-resistant pathogens, and an increasing inclination towards natural and holistic treatment modalities.4,5 This renewed focus is corroborated by scientific investigations progressively affirming the efficacy of traditional herbal remedies.5
In Saudi Arabia, herbal medicine is deeply integrated into traditional healthcare, with many families utilising herbal treatments passed down through generations, often in conjunction with conventional medical practices.6 Commonly used herbs in this context include Ajwa dates, celebrated for their nutritional properties; black seed (Nigella sativa), recognised for its immune-enhancing and anti-inflammatory effects; and ginger and garlic, which are frequently employed for their medicinal benefits.7,8 These remedies are commonly used to treat conditions that include digestive disorders, respiratory ailments, and skin issues and for diabetes management.9
The growing interest in herbal medicine has been accompanied by enhanced scientific scrutiny of the safety and efficacy of traditional remedies, prompting various research institutions to explore their potential benefits.4 Furthermore, the Saudi Food and Drug Authority has initiated regulatory measures to ensure the quality and safety of herbal products for consumers.10,11 Despite the significance of herbal medicine within the Saudi healthcare framework, medical education on this topic remains limited, with considerable variability across institutions.9,12 While certain medical schools offer specialized courses in complementary and alternative medicine (CAM), including herbal remedies, others do not include this subject. When herbal medicine is part of the curriculum, it usually focuses on essential topics like potential benefits, associated risks, side effects, and interactions with conventional treatments.13–15
Students are often trained to counsel patients regarding herbal products in clinical settings, and some programmes promote engagement with current research to support evidence-based practices. However, the depth of knowledge acquired in this domain is generally less comprehensive than that in conventional pharmacology, leading students interested in herbal medicine to seek additional resources or elective courses.16,17 The methods of preparation and administration of herbal remedies are diverse, encompassing teas, tinctures, capsules, and topical applications tailored to specific conditions and desired outcomes. Despite its holistic approach aimed at restoring balance and enhancing overall well-being, herbal medicine faces challenges such as variability in product quality and efficacy, influenced by factors like plant species and preparation techniques.18,19 Additionally, differing regulatory standards for herbal products across countries can result in inconsistencies in quality and safety. While many herbs are safe when used appropriately, the potential for adverse effects and interactions with conventional medications underscores the importance of consulting healthcare professionals before using herbal remedies, particularly for individuals undergoing conventional treatments.3,20
The safety of herbal medicine has emerged as a critical concern for clinicians and healthcare systems in Saudi Arabia and globally, given that its improper use can produce adverse effects and increased healthcare costs. However, there is limited research focusing specifically on Saudi Arabia.21 Therefore, this study seeks to evaluate medical students’ knowledge and perceptions regarding herbal medicine in Saudi Arabia, a topic of significant relevance and importance.
Materials and Methods
Ethical Approval
The study was approved by the Biomedical Research Ethics Committee, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia, under the Declaration of Helsinki. The approval number is HAPO-02-K-012-2023-06-1640. At the beginning of the questionnaire, we informed the participants that they were invited to participate in a research study on herbal medicine in Saudi Arabia. This research study aims to evaluate medical students’ knowledge and perceptions regarding herbal medicine in Saudi Arabia. This research is conducted by the Department of Pharmacology and Toxicology, Faculty of Medicine, Umm Al-Qura University, Saudi Arabia. Participation is voluntary and anonymous. If they agree to participate in this study, they can start answering the questionnaire. Participation may not benefit them directly, but it will help us learn about herbal medicine in Saudi Arabia.
Study Design
A cross-sectional study was conducted among medical students in three medical colleges in Saudi Arabia: Umm Al Qura Medical College, King Abdulaziz Medical College and Batterjee Medical College. They were randomly approached by sending an electronic questionnaire over a six-month period from 1 February to 31 July 2024. They were contacted through social media channels such as Twitter, Instagram, WhatsApp, Telegram, and email. The purpose of the research was explained to participants in the questionnaire, and they were informed that participation was voluntary.
Questionnaire Tool
The questionnaire was adapted from a previous study by Ameade EP et al.22 Experts offered their insights and recommendations for enhancing the questionnaire, and their suggestions were integrated into the final version, which comprised 29 questions and was created using online cloud-based software (Google Forms). The questionnaire was initially designed in English and then translated into Arabic, the local language, by proficient bilingual translators, with revisions to ensure its suitability for medical students. It was divided into three main parts. The first part included sociodemographic information. The second part was about medical students’ knowledge of herbal medicine. The third part was about medical students’ perceptions of herbal medicine.
Sample Size and Data Collection
The sample size was calculated using Slovin’s formula, with a population size of 458 medical students in Saudi Arabia from a recently published study by Bin KA et al with a confidence interval of 95% and a margin of error of 5%.23 Social media channels were used to distribute the questionnaire. All responses were downloaded from the Google Forms platform and stored on a secure server. A complete case analysis was performed on the answers from participants who fully completed all 29 questions across the three-part survey, while those with incomplete responses were excluded. The data collected from Google Forms spreadsheets were then transferred to Microsoft Excel for analysis.
Statistical Analysis
After data were extracted, they were revised, coded, and fed into the statistical software IBM SPSS version 22 (SPSS, Inc., Chicago, IL). All statistical analyses were conducted using two-tailed tests. A p-value of less than 0.05 was statistically significant. With regard to knowledge and perception regarding herbal medicine, the overall score was obtained by summing up all discrete item scores. Students with an overall score of less than 60% of the maximum score were considered to have poor knowledge and perception levels, while those with an overall score of 60% or more were considered to have overall good levels.
Descriptive analysis based on frequency and percentage distribution was done for all variables: participants’ biodemographic data, academic data and medical history, and their source and history of using herbs. Also, students’ knowledge and perceptions regarding herbal medicine was tabulated with their overall knowledge level and used herbs. Cross-tabulation was used to assess factors associated with participants’ knowledge and perception level about herbal medicine, and factors associated with their use of herbs were tested using Pearson’s chi-square test and an exact probability test for small frequency distributions.
Results
A total of 600 questionnaires were collected, of which eight were excluded because of incomplete responses, giving a response rate of 98%. A total of 592 eligible medical students completed the study questionnaire. The students’ ages ranged from 18 to 30 years, with a mean age of 21.6 ± 4.8 years old. A total of 389 (65.7%) students were female. As for academic grade, 335 (56.6%) were in the pre-clinical years (1st to 3rd years), and 257 (43.4) were in their clinical years (4th to 6th years). Only 64 (10.8%) had a chronic health problem. As for monthly income, it ranged from 1000 to 5000 SR among most of the students (73%; 432), and 90 (15.2%) had monthly income exceeding 10000 SR, as shown in Table 1.
 |
Table 1 Bio-Demographic Data of the Study Medical Students (N=592) |
A total of 76.7% of the students said that people trust herbal medicine because it is an inherited practice and has its origins in ancient cultures, and 72.6% of the students agreed that medical students lack proper knowledge about the use of herbal medicines, as shown in Table 2. Also, 69.8% reported that the use of complementary and herbal medicine needs to be taught to medical students, 67.2% agreed that the safety of herbal products is essential because the majority of these products are self-prescribed and used to treat chronic diseases, and 64.9% preferred having an elective course in complementary medicine (including herbal medicine). On the other hand, 62.3% disagreed with the proposition that herbal medicines do not have a toxicity level, 59% disagreed with the proposition that herbal medicines do not have side effects because they are from natural ingredients, and 54.6% responded “No” when asked if they use herbal medicine because the cost of visiting a conventional medicine physician is too high.
 |
Table 2 Medical Students’ Knowledge and Perception Towards Herbal Medicine |
As shown in Table 3, the most reported sources of information included family and friends (53.2%), the internet/social media (25.2%), traditional herbalists (Attar) (9.6%), physician/pharmacist specialised in herbal medicine (9.3%), and complementary medicine course/workshop (2.7%). As for the source of herbs, traditional herbalist (Attar) was the most reported (49.3%), followed by online (23.6%), herbal medicine pharmacy (15%), and travelling (12%). Most of the students (94.4%; 559) use herbs to treat their conditions.
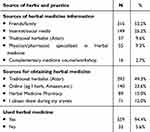 |
Table 3 Source of Herbs Information, Source of Having Herbs and Frequency of Having Herbs Among Students |
Figure 1 shows the types of herbs used by medical students in Saudi Arabia. The most used herbs were ginger (83%), turmeric (48.1%), chamomile (46.3%), myrrh (26.5%), ginseng (20.8%), and habba al-barakah (Nigella sativa) (18.4%). Other herbs include (cumin, nutmeg, cloves, date palm, arak and oregano). As shown in Table 4, A total of 69.2% of students aged 27–30 years had an overall good knowledge and perception level versus 33.3% of others aged 22–26 years old, with a recorded statistical significance (P = 0.041). In addition, 45.1% of students who obtained herbs during their travels had an overall good knowledge and perception compared with 27% of others who obtained them from an herbal medicine pharmacy (P = 0.048). Likewise, 37.7% of students who used herbs had an overall good knowledge and perception, compared with 3% of others who did not (P = 0.001).
 |
Table 4 Factors Associated with Medical Students’ Knowledge and Perception Towards Herbal Medicine |
 |
Figure 1 Types of herbs used by medical students. |
As shown in Table 5, only gender showed a significant relationship with herb use among the students: 95.4% of female students used herbs, compared with 92.6% of male students (P = 0.049). Other factors showed insignificant reactions to students’ use of herbs.
 |
Table 5 Factors Associated with Medical Students’ Use of Herbs |
Discussion
This research aimed to evaluate the knowledge and perception of herbal medicine among medical students in Saudi Arabia. A significant portion of the participants (55.4%) were under the age of 22, indicating that most were still in the early phases of their medical education. Similarly, a study in Malaysia revealed that younger medical students (with a mean age of 21.2 years) demonstrated considerable interest in CAM, including herbal medicine. This enthusiasm among younger students may stem from their receptiveness to various medical practices and integrative healthcare approaches.24
The gender distribution indicates a higher percentage of female students (65.7%) than male students. Female medical students were found to be more inclined to use and support herbal medicine. This trend may influence the student body’s overall perception and acceptance of herbal remedies.25 It is important to note that both male and female students utilised herbal products; however, the proportion of female users (95.4%) was slightly higher than that of male users (92.6%) (P = 0.0049). This finding aligns with research from the United States, which indicates that women are more likely to use CAM than men. Studies suggest that women commonly use herbs to address hormonal imbalances and menstrual cramps. Such practices are often passed down through generations, especially among women.26,27
A substantial majority of medical students (69.8%) supported the inclusion of complementary and herbal medicine in medical school curricula, with 64.9% favouring an elective course in this area, reflecting a strong interest in integrating herbal medicine education. Similar findings have been reported in other countries, such as Malaysia, where 62% of medical students advocated for the inclusion of CAM in their curriculum and 74.8% believe that a lack of scientific evidence is one of the most important barriers obstructing their use of CAM.28 This highlights a significant knowledge gap that poses risks to patient care. Another US study found that only 39% of medical students felt sufficiently knowledgeable about herbal medicine, suggesting a critical need for educational interventions.29
While 76.7% expressed their trust in herbal medicine due to its cultural significance, misconceptions persist, as 22.3% of students wrongly believe that herbal medicines lack side effects and 20.8% think they can safely be taken with pharmaceuticals. These misconceptions highlight the urgent need for enhanced education regarding the risks and interactions related to herbal medicine.4,30 They may also overrate the effectiveness of herbal products and fail to recognise the importance of scientific validation. Furthermore, confusion surrounding proper dosage, preparation methods, and quality variability can result in inappropriate use, emphasising the necessity for better educational initiatives in these areas.31,32
Misconceptions by 21.3% of students that herbal medicines do not expire and by 15.7% that they lack toxicity can lead to unsafe practices. Educational programmes should aim to correct these wrong beliefs to promote safe usage. Interestingly, 56.6% of the students acknowledged that herbal medicine lacks full evidence-based validation, demonstrating an awareness of the need for scientific support in integrating herbal remedies into mainstream healthcare. The primary source of information for 53.2% of students was friends and family, consistent with findings from studies in Turkey, India, and the U.S. 33–35 This reliance on informal sources underscores the importance of promoting evidence-based education within medical curricula. For instance, a clinical study indicated that 55.59% of medical students preferred to seek knowledge from the internet or social media.36
Medical schools could benefit from establishing exclusive online resources where experts share the latest information on herbal medicine, specifically for students.37 Additionally, hosting certified herbalists in virtual sessions could enhance communication and learning opportunities.38 It is crucial for medical students to gain a comprehensive understanding of the uses, interactions, and potential side effects of herbs as they prepare for clinical practice.17 Currently, only 2.7% of students reported learning about herbs through complementary medicine workshops, likely due to a lack of academic staff specialising in evidence-based herbal therapy. Employing professionals with expertise in herbal medicine could improve students’ knowledge in this area.39
Ginger is widely used by 83% of medical students, aligning with findings from a Saudi study that identified it as a common traditional remedy.21 Ginger is extensively used in Saudi Arabia for several reasons. It has a deep-rooted presence in traditional medicine and cuisine, appreciated for its flavour and health benefits. Known for its medicinal qualities—such as anti-inflammatory, antioxidant, and digestive properties—it acts as a remedy for various ailments.40,41 Its easy availability in local markets makes it accessible to many, and its widespread acceptance encourages its use in home remedies and healthcare. Moreover, ginger’s versatility in forms like fresh, dried, or powdered allows for various culinary and herbal uses, reinforcing its status as a staple in Saudi homes.21 Additionally, gingerol, the active component of ginger, offers antioxidant benefits that may enhance gastrointestinal health and alleviate stress-related pain in medical students, who experience varying stress levels, particularly during their clinical years.42 Ginger is also effective for menstrual cramps, supports immune function, and is both affordable and accessible for students.36
The assessment of medical students’ knowledge of herbal medicine primarily emphasizes their foundational understanding rather than their advanced or specialized expertise. This distinction is important as it reveals a potential gap in the students’ educational preparation. The evaluation focused on their general awareness and basic information about herbal medicine, rather than their ability to apply professional concepts or practices in this area. This highlights that the current training may not sufficiently equip students for the professional application of herbal medicine, which necessitates a more profound understanding and critical analytical skills.
To improve herbal medicine knowledge and perception among medical students, it is important to incorporate thorough courses into the curriculum and host workshops with experts. Promoting research projects and interdisciplinary collaboration can enhance understanding. Clinical exposure and access to online resources will support practical learning and independent study. Additionally, engaging students in patient education initiatives and establishing feedback mechanisms can help identify knowledge gaps and enhance their educational experiences. However, our study has a limitation: its reliance on an online survey may not fully capture the perspectives of all medical students, particularly those who are not active on social media. Despite this, the research offers valuable insights into the knowledge of herbal medicine among medical students in Saudi Arabia, a field that remains underexplored.
Conclusion
To enhance medical students’ knowledge and perception of herbal medicine, it is essential to integrate comprehensive courses and workshops led by experts into the curriculum. The primary sources of information for these students were family and friends, while traditional herbalists (Attar) served as the primary suppliers of herbs. Notably, only 37.7% of students who used herbs demonstrated a strong understanding and perception of these remedies. Promoting research and interdisciplinary collaboration can also encourage critical thinking and ensure students remain informed about recent developments. Furthermore, incorporating clinical exposure, online resources, patient education initiatives, and feedback mechanisms can effectively identify knowledge gaps and enrich the educational experience.
Disclosure
The authors report on conflicts of interest in this work.
References
1. Rojas P, Jung-Cook H, Ruiz-Sánchez E, et al. Historical aspects of herbal use and comparison of current regulations of herbal products between Mexico, Canada and the United States of America. Int J Environ Res Public Health. 2022;19(23):15690. doi:10.3390/ijerph192315690
2. Saad B, Azaizeh H, Said O. Tradition and perspectives of Arab herbal medicine: a review. Evid Based Complement Alternat Med. 2005;2(4):475–479. doi:10.1093/ecam/neh133
3. Wang H, Chen Y, Wang L, Liu Q, Yang S, Wang C. Advancing herbal medicine: enhancing product quality and safety through robust quality control practices. Front Pharmacol. 2023;14:1265178. doi:10.3389/fphar.2023.1265178
4. Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 2014;4:177. doi:10.3389/fphar.2013.00177
5. Ernst E. Herbal medicines: where is the evidence? BMJ. 2000;321(7258):395–396. doi:10.1136/bmj.321.7258.395
6. Abdelmola AO, Bahri A, Abuallut I, et al. Prevalence, knowledge, and perception about the use of herbal medicines jazan - Saudi Arabia. J Family Med Prim Care. 2021;10(6):2386–2393. doi:10.4103/jfmpc.jfmpc_2475_20
7. Ahmad A, Husain A, Mujeeb M, et al. A review on therapeutic potential of Nigella sativa: a miracle herb. Asian Pac J Trop Biomed. 2013;3(5):337–352. doi:10.1016/S2221-1691(13)60075-1
8. Ali HH, Alharbi SF, Iskandar RA, Mira GB, Yanogue AS, Alboualy EA. Perception and use of herbal medicine in general practice patients: a cross-sectional study in Saudi Arabia. Cureus. 2024;16(3):e56806. doi:10.7759/cureus.56806
9. Al Akeel MM, Al Ghamdi WM, Al Habib S, Koshm M, Al Otaibi F. Herbal medicines: Saudi population knowledge, attitude, and practice at a glance. J Family Med Prim Care. 2018;7(5):865–875. doi:10.4103/jfmpc.jfmpc_315_17
10. Zaidi SF, Saeed SA, Khan MA, et al. Public knowledge, attitudes, and practices towards herbal medicines; a cross-sectional study in Western Saudi Arabia. BMC Complement Med Ther. 2022;22(1):326. doi:10.1186/s12906-022-03783-y
11. Al-Arifi MN. Availability and needs of herbal medicinal information resources at community pharmacy, Riyadh region, Saudi Arabia. Saudi Pharm J. 2013;21(4):351–360. doi:10.1016/j.jsps.2012.11.004
12. Alasiri AA, Mohammed V. Healthcare Transformation in Saudi Arabia: an overview since the launch of vision 2030. Health Serv Insights. 2022;15:11786329221121214. doi:10.1177/11786329221121214
13. Complementary CotUo, Public AMbtA. Complementary and Alternative Medicine in the United States. United States: National Academies Press; 2005.
14. Cowen VS, Cyr V. Complementary and alternative medicine in US medical schools. Adv Med Educ Pract. 2015;113–117. doi:10.2147/AMEP.S69761
15. Alzahrani SH, Bashawri J, Salawati EM, Bakarman MA. Knowledge and attitudes towards complementary and alternative medicine among senior medical students in King Abdulaziz University, Saudi Arabia. Evidence-Based Complement Alternat Med. 2016;2016(1):9370721. doi:10.1155/2016/9370721
16. Büntzel SK, Ritschel ML, Wurm-Kuczera R, Büntzel J. Indications of medical plants: what do medical students in Germany know? A cross-sectional study. J Cancer Res Clin Oncol. 2022;148(11):3175–3182. doi:10.1007/s00432-022-03921-6
17. Alsanosi SM. A new vision of teaching clinical pharmacology and therapeutics for undergraduate medical students. Adv Med Educ Pract. 2022;13:567–575. doi:10.2147/AMEP.S359704
18. Hassen G, Belete G, Carrera KG, et al. Clinical Implications of herbal supplements in conventional medical practice: a US perspective. Cureus. 2022;14(7):e26893.
19. Gari A, Yarlagadda R, Wolde-Mariam M. Knowledge, attitude, practice, and management of traditional medicine among people of Burka Jato Kebele, West Ethiopia. J Pharm Bioallied Sci. 2015;7(2):136–144. doi:10.4103/0975-7406.148782
20. Zhang J, Onakpoya IJ, Posadzki P, Eddouks M. The safety of herbal medicine: from prejudice to evidence. Evid Based Complement Alternat Med. 2015;2015:316706. doi:10.1155/2015/316706
21. Syed W, Samarkandi OA, Sadoun AA, Bashatah AS, Al-Rawi MBA, Alharbi MK. Prevalence, beliefs, and the practice of the use of herbal and dietary supplements among adults in Saudi Arabia: an observational study. Inquiry. 2022;59:469580221102202. doi:10.1177/00469580221102202
22. Ameade EP, Amalba A, Helegbe GK, Mohammed BS. Medical students’ knowledge and attitude towards complementary and alternative medicine - A survey in Ghana. J Tradit Complement Med. 2016;6(3):230–236. doi:10.1016/j.jtcme.2015.03.004
23. Bin Abdulrahman KA, Alobaida BA, Alzabadin RA, et al. Future dreams of junior and senior medical students at a public Saudi Medical School. Adv Med Educ Pract. 2022;13:1187–1195. doi:10.2147/AMEP.S375627
24. Hasan SS, Ahmed SI, Bukhari NI, Loon WC. Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement Ther Clin Pract. 2009;15(3):152–157. doi:10.1016/j.ctcp.2009.02.003
25. Alwhaibi M, Sambamoorthi U. Gender differences in the use of complementary and alternative medicine among adults with multiple chronic conditions. Value Health. 2015;18(3):A90–A1. doi:10.1016/j.jval.2015.03.530
26. Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: a systematic review. Ochsner J. 2012;12(1):45–56.
27. Jawahar R, Yang S, Eaton CB, McAlindon T, Lapane KL. Gender-specific correlates of complementary and alternative medicine use for knee osteoarthritis. J Womens Health (Larchmt). 2012;21(10):1091–1099. doi:10.1089/jwh.2011.3434
28. Hasan SS, Yong CS, Babar MG, et al. Understanding, perceptions and self-use of complementary and alternative medicine (CAM) among Malaysian pharmacy students. BMC Complement Altern Med. 2011;11(1):95. doi:10.1186/1472-6882-11-95
29. Wetzel MS, Eisenberg DM, Kaptchuk TJ. Courses involving complementary and alternative medicine at US medical schools. JAMA. 1998;280(9):784–787. doi:10.1001/jama.280.9.784
30. Boshuizen HP, Marambe KN. Misconceptions in medicine, their origin and development in education and working life. Int J Educ Res. 2020;100:101536. doi:10.1016/j.ijer.2020.101536
31. Deng G, Cassileth B. Complementary or alternative medicine in cancer care—myths and realities. Nat Rev Clin Oncol. 2013;10(11):656–664. doi:10.1038/nrclinonc.2013.125
32. Ozdemir H. Truths and misconceptions of the plants used in traditional medicine. Вестник Ошского государственного университета. 2023;3:1–7.
33. Guven H, Kalkan S, Hocaoglu N, Yildiztepe E, Gokalp G. Evaluation of the knowledge level and usage attitudes of the medical students on the medicinal herbs and herbal products: a project of special study module in the first three years of the school of medicine. Int J Basic & Clin Pharmacol. 2019;8(3):394–401. doi:10.18203/2319-2003.ijbcp20190566
34. Sekhri K, Bhanwra S, Nandha R. Herbal products: a survey of students’ perception and knowledge about their medicinal use. Int J Basic Clin Pharmacol. 2013;2(1):71–76. doi:10.5455/2319-2003.ijbcp20130114
35. Ayranci U, Son N, Son O. Prevalence of nonvitamin, nonmineral supplement usage among students in a Turkish university. BMC Public Health. 2005;5(1):1–10. doi:10.1186/1471-2458-5-47
36. Boparai JK, Singh A, Gupta AK, et al. A study to determine the knowledge and level of awareness of medical undergraduates about herbal medicines and herb-drug interactions. Int J Basic & Clin Pharmacol. 2017;6(1):17.
37. Berberoglu I, Tang SYQ, Kozlow JH, Sezgin B, Sandhu G, Cederna PS. Integration of virtual and traditional medical education: scholarship pivots from the COVID-19 pandemic. Plast Reconstr Surg Glob Open. 2024;12(6):e5910. doi:10.1097/GOX.0000000000005910
38. Nalubega S, Kutyabami P, Twimukye A, Mafigiri DK, Sewankambo NK. Practices and attitudes of herbalists regarding informed consent in Uganda: a qualitative study. Res Sq. 2024. doi:10.21203/rs.3.rs-3911823/v1
39. Wachtel-Galor S, Benzie IFF. Herbal Medicine: an Introduction to Its History, Usage, Regulation, Current Trends, and Research Needs. In: Benzie IFF, Wachtel-Galor S, editors. Herbal Medicine: Biomolecular and Clinical Aspects. Chapter 1.
40. Shaukat MN, Nazir A, Fallico B. Ginger bioactives: a comprehensive review of health benefits and potential food applications. Antioxidants (Basel). 2023;12(11). doi:10.3390/antiox12112015
41. Ballester P, Cerdá B, Arcusa R, Marhuenda J, Yamedjeu K, Zafrilla P. Effect of ginger on inflammatory diseases. Molecules. 2022;27(21):7223. doi:10.3390/molecules27217223
42. Anh NH, Kim SJ, Long NP, et al. Ginger on human health: a comprehensive systematic review of 109 randomized controlled trials. Nutrients. 2020;12(1):157. doi:10.3390/nu12010157
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Knowledge and Awareness of Non-Technical Skills Over the Course of an Educational Program in Nursing - A Repeated Cross-Sectional Study
Wevling A, Olsen BF, Nygaard AM, Heiberg T
Advances in Medical Education and Practice 2023, 14:31-41
Published Date: 10 January 2023
Knowledge, Perceptions, and Practices on Risks and Disasters Among Medical Students. A Multicenter Cross-Sectional Study in 9 Latin American and Caribbean Countries
Izquierdo-Condoy JS, Montiel-Alfonso MA, Nati-Castillo HA, Saucedo R, Jaramillo-Aguilar DS, Nanjari-Barrientos C, García-Arévalo C, Rivera-Flores D, Díaz Batista MI, Loaiza-Guevara V, Ortiz-Prado E
Advances in Medical Education and Practice 2023, 14:225-235
Published Date: 14 March 2023
Radiologic Technology Students’ Perceptions on Adoption of Artificial Intelligence Technology in Radiology
Arif WM
International Journal of General Medicine 2024, 17:3129-3136
Published Date: 16 July 2024
Knowledge, Attitudes, and Educational Gaps About Vaccination in Chinese Medical Students and Residents: A Pilot Study from a Single Tertiary Referral Center
Liu X, Chen Y, Dai H, Li R, Ding Y, Wu J, Shi X
Infection and Drug Resistance 2024, 17:5315-5323
Published Date: 29 November 2024
Knowledge, Attitudes, and Perceptions of Chronic Patients in Saudi Arabia Regarding the Use of Artificial Intelligence to Improve Medication Adherence
Alsanosi SM, Aldajani AQ, Gheliwi HA, Alotibi MM, Bokhari GS, Almatrafi OA, Alqawlaq AK, Abujamai JZ, Shaikhomer M, Alhindi YZ, Alshanberi AM
Patient Preference and Adherence 2025, 19:1781-1792
Published Date: 19 June 2025

