Back to Journals » Infection and Drug Resistance » Volume 18
Nanobubble Ozone Stored in Hyaluronic Acid-Decorated Liposome Solutions: Inactivating Antibiotic-Resistant Bacteria and Genotoxicity, Sub-Acute and Sub-Chronic Toxicity Tests
Authors Erkan Alkan P , Karabiyik T
Received 23 July 2024
Accepted for publication 22 October 2024
Published 16 January 2025 Volume 2025:18 Pages 313—328
DOI https://doi.org/10.2147/IDR.S478643
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandip Patil
Perihan Erkan Alkan,1 Talha Karabiyik2
1Department of Medical Microbiology, Faculty of Medicine, Bandırma Onyedi Eylül University, Bandırma,/Balıkesir, Turkey; 2Department of Medical Biochemistry, Faculty of Medicine, Bandırma Onyedi Eylül University, Bandırma/Balıkesir, Turkey
Correspondence: Perihan Erkan Alkan, Bandırma Onyedi Eylül University, Faculty of Medicine, Department of Medical Microbiology, Bandırma/Balıkesir, Türkiye, Tel +905331683073, Email [email protected]
Introduction: Nanobubble ozone stored in hyaluronic acid-decorated liposomes (patent application PCT/TR2022/050177) was used, and the Minimum Inhibitory Concentration (MIC) was found to be 1562 ppm. Pseudomonas aeruginosa (patient isolate), Acinetobacter baumannii (patient isolate), Methicillin-Resistant Staphylococcus aureus (MRSA) (ATCC12493), and Escherichia coli (ATCC25922) bacteria, which are hospital-acquired and healthcare-associated infections, were used. A time-dependent efficacy study was conducted at 1600 ppm. Our study aimed to determine whether the newly developed solution maintains long-term effectiveness and can be used as an antibacterial agent, especially in intensive care units.
Methods: Antibacterial tests of the nanobubble liposome solution, developed with a different technique than the standard ozonation procedures, were performed with the CLSI M07 A9 (Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard) standard test method, and the solution was tested at Minimal Inhibitory Concentration (MIC) value and time-dependent effects were determined. For the stability test of the nanobubble liposome solution, according to the ASTM F 1980 standard, it was kept at 55 °C for 74 days as two-year stability.
Results: The MIC of the nanobubble ozone solution was 1.562 ppm for MRSA and E. coli (ATCC 25922) standard test method using CLSI M07 A9 (Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard). P. aeruginosa, A. baumannii, Methicillin-Resistant Staphylococcus aureus (MRSA) (ATCC12493), and E. coli (ATCC 25922). No activity was observed at 2 min, but 1600 ppm nanobubble liposomes at 10 min were found to be effective. In terms of effectiveness, the solution would still be effective after 2 years according to the ASTM F 1980 standard, contrary to expectations.
Conclusion: It is thought that nanobubble ozone stored in hyaluronic acid-decorated liposome solutions will play an important role in the fight against infections because of its non-toxic effect, effectiveness against resistant bacteria, and stability for at least two years. In the following process, it would be appropriate to support the product through clinical studies.
Keywords: nanobubble liposomes, ozone, NOHAL, antibacterial agents, genotoxicity, sub-acute toxicity, sub-chronic toxicity
Introduction
Nosocomial infections caused by resistant bacteria have emerged as a significant global health challenge, particularly in hospital settings where vulnerable populations are treated. The selection and effectiveness of treatment options for these infections are complicated by the increasing prevalence of antibiotic-resistant strains, especially gram-negative bacteria. This trend is alarming because gram-negative bacteria are often associated with severe infections in critically ill patients.1,2 Surveillance studies have consistently demonstrated that the incidence of resistance in gram-negative bacteria is notably higher in patients with severe underlying conditions, complicating treatment protocols, and increasing morbidity and mortality rates.3
Several risk factors contribute to the development of nosocomial infections, including disruption of the normal bacterial flora, immunosuppression, and the use of invasive medical devices. Extended hospital stays, particularly in intensive care units (ICUs), further exacerbate the risk of infection.4
Given these challenges, the treatment of infections caused by resistant bacteria is complicated by the limited availability of new antibiotics. The inappropriate and widespread use of antibiotics in hospital settings, particularly in ICUs, has led to the emergence of multidrug-resistant organisms.5,6 This situation necessitates a multifaceted approach to infection control, including stringent antimicrobial stewardship programs and the exploration of novel therapeutic strategies.
A promising area of research involves the use of nanobubble ozone liposomes, which have demonstrated antibacterial properties in preliminary studies.7–10 When combined with liposomes, these nanobubbles may enhance the delivery of antimicrobial agents and improve their efficacy against resistant bacterial strains.11–13 Moreover, aging tests performed according to the ASTM F1980 standard indicate that these nanobubble formulations maintain their effectiveness for at least two years, suggesting a viable option for long-term infection control strategies.14 As the healthcare community continues to grapple with the implications of antibiotic resistance, the integration of innovative technologies, such as nanobubble ozone liposomes, may provide a critical tool in the fight against nosocomial infections.
In light of this, our study aimed to comprehensively evaluate nanobubble ozone liposomes as a novel antimicrobial strategy against resistant bacterial infections. Specifically, we assessed their stability, subacute toxicity, subchronic toxicity, and genotoxicity. By investigating these key parameters, we hope to establish the safety and efficacy of nanobubble ozone liposomes, and contribute to the development of effective solutions for combating nosocomial infections in healthcare settings.
Materials and Methods
Animals
The experimental animals used in this study were obtained from Burdur Mehmet Akif Ersoy University, Experimental Animal Production, and Experimental Research Center. Salmonella typhimurium strains TA1535, TA97a, TA98, TA100, and TA102 used for genotoxicity testing were obtained from Isparta Süleyman Demirel University. All experimental procedures involving the use of animals were approved by the Akdeniz University Committee for Animal Care and Use (B.30.2. AKD.0.05.07.00/141), carried out according to the Animal Experiments Local Ethics Committee (Akhadyek) Establishment and Procedure Guidelines.
All experimental procedures involving the use of animals were approved by Medicert Laboratories. The Medicert Test Laboratory is accredited by IAKS, a notified body based in the United States of America. The accreditation number was IAKS-TL-1018. The necessary conditions for animal welfare were fulfilled according to TS EN ISO 10993–2. Guide for The Care and Use of Laboratory Animals Eighth Edition National Research Council of The National Academies.
All Methods in Our Study are Reported in Accordance with the ARRIVE Guidelines
The clinical isolates used in our study were bacterial strains used for educational purposes at Bursa Uludağ University, Faculty of Medicine. These strains are registered in the Antimicrobial Efficacy Testing Laboratory of the Department of Medical Microbiology and do not require ethical approval.
Preparation of the Antimicrobial Solution
The ozone dosage was prepared using vegetable oil. While only the ozone amount in ozonated oil could be given in previous ozone oil products accepted in the literature, the dosage into our product is clearly defined. Therefore, the advantage of obtaining a more active nanobubble liposome solution is that smaller ozone dosages ensure stability and activity.
In this study, the ozonation levels of vegetable oils were assessed by the weight of ozone in the oil structures, and are indicated in terms of mg/g. The scope of the previous literature in the field is limited only to the specification of the amount of ozone bubbles in solutions. What sets this study apart is its extended scope and ability to clearly indicate the ozonation levels of vegetable oils, as well as the percentage and weight of ozone particles in the solutions. Homogenized nanobubble liposome suspension was obtained using high-speed ultrasonic cavitation and cold fusion technique of distilled water containing ozonized medicinal vegetable oil, 0.9% NaCl. The amount of ozone in these solutions was recorded in terms of mg/L.9–12
Antibacterial Activity of Nanobubble Liposome Solution
Microorganisms indicate different ways of increasing awareness of antimicrobial products. This situation may vary depending on both the nature of the antibacterial product and the type of microorganism. In this respect, it is necessary to determine the static and/or biocidal effect of antimicrobial products to be used for preventive purposes and, most importantly, for treatment against a specific disease agent, and such a product should be selected and used within a program in a sufficient time and dose.
Determination of the Minimal Inhibitory Concentration (MIC) of the Nanobubble Ozone Solution
Antibacterial tests were performed using the standard test method CLSI M07 A9 (Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard), and the Minimal Inhibitory Concentration value of nanobubble ozone solution was determined. The MIC value was determined using S. aureus (ATCC 25923) and E. coli (ATCC 25922). Following the recommendations of CLSI (The Clinical & Laboratory Standards Institute), a bacterial suspension was prepared from 24-h bacterial culture colonies equal to 0.5 McFarland turbidity and placed in U-bottom tubes with a final concentration of 3×106 colony forming units (CFU)/mL. A stock solution containing 50,000 ppm ozone was prepared and serially diluted to final ozone concentrations of 50,000, 25,000, …, 97 ppm. Afterward, the samples taken from the tubes using standard loops were inoculated on blood agar medium (Becton Dickinson, Germany), and the lowest concentration of nanobubble ozone solution, in which no visible growth was observed, was accepted as the MIC after 24 h incubation at 37 °C. E. coli (ATCC 25922) suspension was used for positive control, and nanobubble liposome solution without bacterial suspension was used for negative control.
Determination of the Time-Dependent Effect of Nanobubble Ozone Solution
After determining the minimal inhibitory concentration value, P. aeruginosa, A. baumannii, MRSA (ATCC12493), and E. coli (ATCC25922) were adjusted to 0.5 McFarland on the nanobubble ozone solution prepared at a concentration of 1600 ppm higher than the MIC value. E. coli 1600 ppm. Samples were taken from these mixtures at 2, 10, and 30 min, and 1, 2, 3, 4, 5, and 6h, and the samples were inoculated on blood agar medium (Becton Dickinson, Germany) and incubated at 37°C. After 24 h of incubation, the plates were examined for growth. It was examined for growth and the plaques without growth were recorded as the value at which inhibition of growth occurred.
Stability Test of Nanobubble Ozone Solution
For the standard stability test, ozone solution was prepared at the concentration in which the effectiveness was determined as a result of the tests, and it was kept at 55°C for 74 days in lieu of two-year stability according to the ASTM F 1980 standard. At the end of this period, suspensions adjusted to 0.5 McFarland were added to the nanobubble ozone solution, 2, 10, 30 min, and 1.2, 3, 4, 5, and 6h. At the end of the 1-h waiting period, the sample was inoculated on blood agar media (Becton Dickinson, Germany), incubated at 37 °C for 24 h, and evaluated for growth at the end of the period. The effectiveness of the solution at the concentration at which the activity was determined before and at the determined contact time was interpreted as stability. No change in pH was accepted as evidence that the ozone concentration in the product did not change.
Genotoxicity Testing
This study evaluated the genotoxic potential of a ceramic test material following the ISO 10993–12. The test material was sterilized and pulverized. A 2 g sample was incubated in 10 mL of phosphate saline buffer (PBS) at 37 °C for 72 h, creating the test extract. For genotoxicity assays, 0.1 mL of this extract was used per plate.
Salmonella typhimurium strains TA1535, TA97a, TA98, TA100, and TA102 were cultured under specific conditions. TA1535 was grown in Oxoid #2 Nutrient Broth without antibiotics, whereas the other strains were cultured in the same broth but supplemented with ampicillin (25 µg/mL). The TA102 strain additionally required tetracycline (2 µg/mL). Cultures were incubated overnight at 37 °C with 100 rpm shaking until they reached an absorbance of 1–1.2 at 660 nm.
Positive controls (sodium azide, mitomycin C, daunomycin, ICR 191 acridine, 2-aminoanthracene, and benzopyrene) and PBS negative controls were used. The metabolic activation system involved the post-mitochondrial S-9 fraction from Aroclor 1254-induced male Sprague-Dawley rats, supplemented with NADPH RegensysTM A cofactor.
Tests were conducted on each strain with and without S9 metabolic activation. The samples were mixed with histidine/biotin-containing top agar and plated on minimal glucose agar plates. Plates were incubated at 37 °C for 48–72 hours before counting back mutant colonies. Colony counts were averaged over two replicates.
Subacute Systemic Toxicity Testing
The subacute systemic toxicity was evaluated using 20 CD1 mice, aged 8–12 weeks. The study included 10 males and 10 females (5 nulliparous and 5 non-pregnant). Mice were randomly assigned to the control (treated with PBS) and test groups. This test was performed by Medicert Laboratories. The Medicert Test Laboratory is accredited by IAKS, a notified body based in the United States of America. The accreditation number was IAKS-TL-1018. The necessary conditions for animal welfare were fulfilled according to TS EN ISO 10993–2. Guide for The Care and Use of Laboratory Animals Eighth Edition National Research Council of The National Academies.
The dosing followed the ISO 10993–11:2018 standard protocol, considering the animals’ weight, surface area, and physical, chemical, and biological characteristics. Intraperitoneal administration was performed at a rate of 50 mL/kg body weight.
Clinical observations were conducted in accordance with the ISO 10993–1 and ISO 10993–12. The systemic effects were documented and analyzed. Statistical analysis was performed using the Mann–Whitney U-test on IBM SPSS 29, setting the significance level at α = 0.05.
Subchronic Systemic Toxicity Testing
For the subchronic toxicity assessment, 25 Sprague-Dawley rats were divided into a test group (20 rats, equally split between sexes) and a control group (5 rats, 2 females and 3 males). Intraperitoneal ketamine (80 mg/kg) and xylazine (5 mg/kg) were administered to induce anesthesia in rats. The gluteal muscle region was anesthetized, and intramuscular administration of the test or control drug was ensued. For five days, postoperative treatment comprised twice-daily wound dressings. Euthanasia was performed via cervical dislocation on day 40.
Histopathological examinations were conducted on organ sections stained with hematoxylin-eosin, periodic acid-Schiff, and Trichrome-Masson techniques. These staining methods aid in differentiating tissue components and identifying lesions. Each organ was evaluated under a light microscope using specific parameters and scoring.
Statistical comparison between the test and control groups was performed using the Mann–Whitney U-test, conducted using IBM SPSS 29 with an alpha level of 0.05.
Results
The MIC of the nanobubble ozone solution was determined to be 1.562 ppm for S. aureus (ATCC 25923) and E. coli (ATCC 25922) strains using the standard test method CLSI M07 A9. The results are presented in Table 1.
The time-dependent effect of the nanobubble ozone solution and the effectiveness of the nanobubble liposome solutions on P. aeruginosa, A. baumannii MRSA (ATCC12493), and E. coli (ATCC25922) bacteria at 1600 ppm concentration and at different times are presented in Table 2. As a result of the test, it was seen that the activity started after 2 min for all bacteria, and the product was effective from the 10th minute.
The tested solution was kept at 55 °C for 74 days, and a standard stability test corresponding to two years was applied. After 74 days, P. aeruginosa, A. baumannii, Methicillin-Resistant S. aureus (MRSA) (ATCC12493), and E. coli (ATCC25922) strains were added to the nanobubble ozone solution. Its effectiveness was determined at the end of 2 min,10 min,30 min,1h, 2h, 3h,4h, 5h, and 6h contact times, as presented in Table 3. The data obtained are comparable with the data of fresh nanobubble liposome solution, and the solution would still be effective after 2 y according to the ASTM F 1980 standard.
 |
Table 3 NOHAL Solution Stability Test Results. Product Efficacy Study After Aging Test at 55 C for 74 Days According to ASTM F 1980 Standard |
A summary of the genotoxicity test results is provided in Tables 4 and 5. The spontaneous back mutant colony counts for the strains used in this study are displayed in Table 4. The back mutant colony counts for strains TA1535, TA97a, TA98, TA100, and TA102 in the genotoxicity assay are shown in Table 5. The findings presented herein offer a detailed synopsis of the genotoxic potential of the test material.
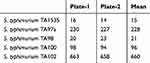 |
Table 4 Spontaneous Back Mutant Colony Numbers |
 |
Table 5 Back Mutant Colony Numbers |
During the course of subacute systemic toxicity testing, none of the individuals in either group exhibited any clinical symptoms of toxicity. The consumption of food and drink in the control and test groups was identical. Body weight measurements in both groups, as presented in Table 6, did not reveal any statistically significant alterations, except for mouse number 17. Similarly, liver index data for all animals, except animal number 16, did not disclose any significant differences between the test and control groups (Table 6).
 |
Table 6 Change in Body Weight of Animals in Subacute Systemic Toxicity Testing |
Pathological examinations conducted after the 28-day observation period revealed specific findings. Notably, emphysema was detected in two lobes of the right lung and a smaller area in the left lung of Female Test 2. Additionally, necrosis was observed in the small lobe of the liver of Female Test 5 mice.
Hematologic and clinical chemistry analyses showed no statistically significant differences between the test and control groups, as indicated by p-values greater than 0.05 (Tables 7–8).
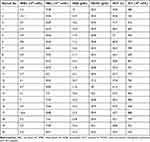 |
Table 7 Hematological Values in Subacute Systemic Toxicity Testing |
 |
Table 8 Clinical Chemistry Values in in Subacute Systemic Toxicity Testing |
In the subchronic systemic toxicity testing, extensive clinical observations were recorded for both the test and control groups. All animals exhibited normal respiration, motor movements, reflexes, and eye function. Cardiovascular and parasympathetic functions, such as salivation levels, were within normal ranges. No instances of piloerection, analgesia, or abnormal muscle tone were observed. Gastrointestinal and skin examinations revealed no abnormalities. Notably, there were no cases of mortality or severe morbidity during the study period.
Body weight changes in both groups remained stable, with no subject experiencing fluctuations exceeding 10% of their original body weight (Table 9).
 |
Table 9 Weight Changes in Rats |
Clinical Chemistry and Complete Blood Count Values are Presented in Table 10 and Table 11, Respectively.
 |
Table 10 Clinical Chemistry Values in in Subchronic Systemic Toxicity Testing |
 |
Table 11 Hematological Values in Subchronic Systemic Toxicity Testing |
No aberrant findings were observed upon morphological assessment of multiple organ systems in either the control or test groups. The brain, heart, kidney, liver, lungs, bronchus, trachea, spleen, muscle, nerve, skin, and several other organs and tissues were assessed during this exhaustive examination. These findings did not reveal any detrimental alterations in the morphology of these structures.
Finally, necropsy of animals from both the test and control groups, which were euthanized via cervical dislocation, revealed no adverse findings.
Discussion
Our study demonstrates that the nanobubble ozone liposome solution, a newly developed antimicrobial agent, maintains remarkable stability and effectiveness over an extended period, challenging the conventional understanding of the rapid degradation of ozone. While gaseous ozone typically has a half-life of approximately 20 min, our findings indicate that when encapsulated within nanobubble liposomes, ozone remains stable and active for at least two years, as confirmed by the accelerated aging test according to the ASTM F1980 standard. This prolonged stability addresses a significant limitation of the therapeutic use of ozone and opens new avenues for its application in infection control.
The antimicrobial efficacy of the nanobubble ozone liposome solution was evident against a spectrum of clinically relevant and resistant bacterial strains, including Pseudomonas aeruginosa, Acinetobacter baumannii, methicillin-resistant Staphylococcus aureus (MRSA), and Escherichia coli. The minimal inhibitory concentration (MIC) was determined to be as low as 1.562 ppm for standard strains of S. aureus and E. coli, and the bactericidal effect was observed within 10 min of exposure at concentrations higher than the MIC. These results underscore the potential of this solution as a potent antimicrobial agent capable of rapidly reducing the bacterial load, which is crucial in preventing and managing nosocomial infections.
Safety is of paramount importance in the development of new antimicrobial agents. Our genotoxicity assessment using the Ames test revealed no mutagenic effects across multiple Salmonella typhimurium strains, both with and without metabolic activation. Additionally, subacute and subchronic toxicity studies in animal models have shown no significant systemic toxicity. Clinical observations, body weight measurements, hematological parameters, and biochemical analyses remained within normal ranges, and histopathological examinations did not indicate any adverse morphological changes in vital organs. These comprehensive safety evaluations suggest that the nanobubble ozone liposome solution is biologically safe for clinical use.
The unique properties of the nanobubble ozone liposome solution, including its natural composition and slow release mechanism, make it a promising candidate for preventive applications. In healthcare settings, especially intensive care units, where patients are highly susceptible to infections due to invasive procedures and immunosuppression, this solution can be used for rinsing the mouth, throat, and nose. Such prophylactic use may help prevent colonization and the establishment of pathogenic bacteria and viruses, thereby reducing the incidence of nosocomial infections.
Our findings align with the urgent need for novel antimicrobial strategies in the face of increasing antibiotic resistance among gram-negative bacteria, as highlighted by Rameshwarnath and Naidoo (2018) and Silvetti et al (2018). By offering an effective solution that maintains stability and exhibits no significant toxicity, the nanobubble ozone liposome formulation could complement existing antimicrobial stewardship programs and contribute to improved infection-control practices.
Future research should focus on clinical trials to evaluate the efficacy and safety of nanobubble ozone liposome solutions in humans. We have planned clinical studies to explore its potential in preventing and treating nosocomial infections, pending the necessary ethical approval. Additionally, investigating the mechanistic aspects of its antimicrobial action could provide deeper insights into optimizing its use in various medical applications.
Conclusion
The nanobubble ozone liposome solution presents a novel and effective antimicrobial approach with significant potential to combat resistant bacterial infections in healthcare settings. Its prolonged stability, rapid and broad-spectrum antimicrobial activity, and favorable safety profile make it a valuable addition to current infection control strategies. Implementing this solution could play a crucial role in addressing the global challenge of antibiotic resistance and improving patient outcomes in hospitals worldwide.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Acknowledgments
We would like to thank SONOFARMA Pharmaceutical Chemicals Industry and Trade Inc.That provided us with the solutions used in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rameshwarnath S, Naidoo S. Risk factors associated with nosocomial infections in the Neonatal Intensive Care Unit at Mahatma Gandhi Memorial hospital between 2014 and 2015. S Afr J Infect Dis. 2018;33(4):93–100. doi:10.1080/23120053.2018.1453641
2. Ploeg J, Davies B, Edwards N, Gifford W, Miller PE. Factors influencing best-practice guideline implementation: lessons learned from administrators, nursing staff, and project leaders. Worldviews Evid Based Nurs. 2007;4(4):210–219. doi:10.1111/j.1741-6787.2007.00106.x
3. Silvetti M, Vassena E, Abrahamse E, Verguts T. Dorsal anterior cingulate-brainstem ensemble as a reinforcement meta-learner. PLoS Comput Biol. 2018;14(8):e1006370. doi:10.1371/journal.pcbi.1006370
4. Koshiyama K, Wada S. Collapse of a lipid-coated nanobubble and subsequent liposome formation. Sci Rep. 2016;6(1):1–8. doi:10.1038/srep28164
5. Ogunyankin MO, Shin JE, Lapotko DO, Ferry VE, Zasadzinski JA. Optimizing the NIR Fluence Threshold for nanobubble generation by controlled synthesis of 10–40 nm hollow gold nanoshells. Adv Funct Mater. 2018;28(10). doi:10.1002/adfm.201705272
6. Brito DVD, Brito C, Resende DS, Moreira DÓJ, Abdallah VOS, Gontijo Filho PP. Nosocomial infections in a Brazilian neonatal intensive care unit: a 4-year surveillance study. Rev Soc Bras Med Trop. 2010;43(6):633–637. doi:10.1590/s0037-86822010000600006
7. Kim GS, Lee KS, Park CK, et al. Nosocomial infection in adult patients undergoing veno-arterial extracorporeal membrane oxygenation. J Korean Med Sci. 2017;32(4):593. doi:10.3346/jkms.2017.32.4.593
8. Wang J, Wang L, Jia M, Du Z, Hou X. Extracorporeal membrane oxygenation-related nosocomial infection after cardiac surgery in adult patients. Braz J Cardiovasc Surg. 2021;36(6). doi:10.21470/1678-9741-2020-0068
9. Alkan PE, Güneş M, Özakin C, Sabanci AÜ. New antibacterial agent: nanobubble ozone stored in liposomes: the antibacterial activity of nanobubble ozone in liposomes and their thymol solutions. Ozone Sci Eng. 2021;43(6):637–641. doi:10.1080/01919512.2021.1904205
10. Cirlini M, Caligiani A, Palla G, De Ascentiis A, Tortini P. Stability studies of ozonized sunflower oil and enriched cosmetics with a dedicated peroxide value determination. Ozone Sci Eng. 2012;34(4):293–299. doi:10.1080/01919512.2012.692992
11. Yu X, Chen M, Liu X, et al. Risk factors of nosocomial infection after cardiac surgery in children with congenital heart disease. BMC Infect Dis. 2020;20(1). doi:10.1186/s12879-020-4769-6
12. Erkan-Alkan P, Günes ME, Özakın C, Sabancı AÜ. nanoparticle liposomes: a new strategy in bacterial infections. Klimik Derg. 2021;34(2):99–102. doi:10.36519/kd.2021.3633
13. Sabancı AU, Erkan Alkan P, Mujde C, et al. Nanobubble ozone stored in hyaluronic acid decorated liposomes: antibacterial, anti-SARS-CoV-2 effect and biocompatibility tests. IJN. 2022;17:351–379. doi:10.2147/IJNS328090
14. Gaynes RP, Culver DH, Horan TC, Edwards JR, Richards C, Tolson JS. Surgical Site Infection (SSI) rates in the United States, 1992–1998: the national nosocomial infections surveillance system basic ssi risk index. Clin Infect Dis. 2001;33(s2):S69–S77. doi:10.1086/321860
15. CLSI M07 A9 (methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard).
16. ASTM F 1980 (standard guide for accelerated aging of sterile barrier systems for medical devices).
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



