Back to Journals » Infection and Drug Resistance » Volume 18
Sequential Therapy of Linezolid and Contezolid to Treat Hematogenous Lung Abscess Caused by Staphylococcus aureus in a Congenital Cerebral Hypoplasia Patient: A Case Report
Received 26 October 2024
Accepted for publication 1 January 2025
Published 13 January 2025 Volume 2025:18 Pages 253—260
DOI https://doi.org/10.2147/IDR.S502839
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Shuang Zhou,1 Chengqi Xin,2– 5 Wenjuan Liu1
1Department of Respiratory and Critical Care Medicine, The First Affiliated Hospital of Dalian Medical University, Dalian, Liaoning, People’s Republic of China; 2Stem Cell Clinical Research Center, The First Affiliated Hospital of Dalian Medical University, Dalian, Liaoning, People’s Republic of China; 3National Local Joint Engineering Laboratory, The First Affiliated Hospital of Dalian Medical University, Dalian, Liaoning, People’s Republic of China; 4National Genetic Test Center, The First Affiliated Hospital of Dalian Medical University, Dalian, Liaoning, People’s Republic of China; 5Liaoning Key Laboratory of Frontier Technology of Stem Cell and Precision Medicine, Dalian Innovation Institute of Stem Cell and Precision Medicine, Dalian, Liaoning, People’s Republic of China
Correspondence: Wenjuan Liu; Chengqi Xin, Email [email protected]; [email protected]
Abstract: Staphylococcus aureus is a common pathogen of hematogenous lung abscesses. The increased resistance of S. aureus to antibiotics makes infections difficult to treat, often resulting in a poor prognosis. Therefore, it is important to identify S. aureus infections as early as possible and evaluate its sensitivity and resistance to antibiotics, to formulate an appropriate treatment plan. Oxazolidinone antibiotics exhibit potent antibacterial activity against multidrug-resistant (MDR) S. aureus; however, the adverse effects of linezolid, particularly thrombocytopenia, limit its application. Contezolid may ameliorate the hematologic toxicity associated with linezolid. Here, we report the case of a patient with congenital cerebral hypoplasia who was hospitalized due to fever and multiple abscesses in both lungs. In the context of negative blood culture results, the final diagnosis of MDR S. aureus as the causative agent of hematogenous lung abscess was confirmed using macrogenomic next-generation sequencing (mNGS) and targeted next-generation sequencing (tNGS). The patient was treated with linezolid but developed significant thrombocytopenia, so switching to sequential therapy with contezolid, the patient’s platelet counts returned to normal and his condition improved significantly.
Keywords: hematogenous lung abscess, Staphylococcus aureus, linezolid, contezolid, next-generation sequencing, congenital cerebral hypoplasia
Introduction
Hematogenous lung abscesses are primarily caused by pathogens from extrapulmonary sources that spread to the lungs through the bloodstream, leading to small vessel embolism, inflammation, and necrosis, which ultimately result in the formation of lung abscesses. These abscesses often present as multiple lesions in the peripheral regions of both lungs. Common causative pathogens include Staphylococcus aureus, S. epidermidis, and Streptococcus. Diagnosis primarily relies on blood cultures to detect pathogenic bacteria, in conjunction with clinical symptoms and characteristic imaging findings. However, the sensitivity and positive detection rate of conventional blood cultures are not ideal. In this case, we utilized metagenomic next-generation sequencing (mNGS) and targeted next-generation sequencing (tNGS) to identify the pathogenic bacteria causing hematogenous lung abscesses in the patient as multidrug-resistant (MDR) S. aureus, which was sensitive to vancomycin. Consequently, vancomycin was administered via intravenous drip for anti-infective therapy during hospitalization, and the patient was switched to oral linezolid after discharge. Not unexpectedly, the patient developed thrombocytopenia after half a month, prompting the discontinuation of linezolid and the use of oral contezolid as an alternative treatment. Subsequently, the patient’s platelet count returned to normal levels, and his symptoms improved. Multiple studies have reported that contezolid can be an appropriate alternative for patients who are intolerant to linezolid.1–4
Case Presentation
A 45-year-old male was admitted to the First Affiliated Hospital of Dalian Medical University with the chief complaint of fever, cough, and productive sputum, followed by respiratory distress and shortness of breath for 10 days. He had previously received treatments aimed at alleviating his symptoms, such as anti-infective therapy, cough relief, and sputum reduction at a different hospital. However, his symptoms did not show significant improvement, leading to his admission to our hospital through the emergency department on March 2, 2024. Chest computed tomography (CT) (Figure 1A) revealed multiple nodules and patchy areas of increased density in both lungs, with gas density shadows observed within the larger nodules, suggesting the possibility of an Aspergillus infection, as well as pleural effusion on both sides. For further diagnosis and treatment, he was admitted to the Department of Respiratory and Critical Care Medicine. The patient had congenital cerebral hypoplasia for over 40 years and was recently diagnosed with type 2 diabetes. Physical examination upon admission revealed a body temperature of 37.9°C, a heart rate of 120 beats/min, a respiratory rate of 20 times/min, and blood pressure of 134/77 mmHg. The patient appeared generally unwell, with lethargy, thick breathing sounds in both lungs, and audible dry and moist rales. His heart rate was regular, with no abnormal sounds detected during the auscultation of the heart valves. The abdomen was flat and soft, with no tenderness, rebound pain, or muscle rigidity. Scattered bleeding spots were noted on both lower limbs, and the dorsum of the right foot exhibited an ulcer (Figure 2).
 |
Figure 2 The patient’s dorsalis skin of the right foot was ulcerated. |
Results of relevant auxiliary tests after admission were as follows: C-reactive protein (CRP): 63.31 mg/L (normal range ≤ 0.8 mg/L); blood routine examination: white blood cell (WBC) count 12.97×109/L (normal range 3.5–9.5×109/L), red blood cell (RBC) count 3.33×1012/L (normal range 4.3–5.8×1012/L), hemoglobin (HB) 92.00 g/L (normal range 130–175 g/L), platelet (PLT) count 198×109/L (normal range 125–350×109/L), neutrophil percentage 87.40% (normal range 40–75%); procalcitonin (PCT): 0.52 ng/mL (normal range ≤ 0.5 ng/mL); erythrocyte sedimentation rate (ESR): 69.00 mm/h (normal range ≤ 20 mm/h); interleukin-6 (IL-6): 47.10 pg/mL (normal range ≤ 5.3 pg/mL); ferritin: 1247.00 µg/L (normal range 30 µg/L–400 µg/L); and arterial blood gas analysis: pH 7.521 (normal range 7.35–7.45), partial pressure of carbon dioxide 28.7 mmHg (normal range 35–45 mmHg), partial pressure of oxygen 100 mmHg (normal range 80–100 mmHg), and sulfur dioxide 97.6%. Nucleic acid detection for respiratory pathogens showed positive results for influenza B virus, whereas tests for novel coronavirus nucleic acid, Cryptococcus neoformans capsular polysaccharide antigen, galactomannan, tumor markers, tubercle bacillus polymerase chain reaction (TB-PCR), blood culture, and sputum smear were negative. Cardiac ultrasound and abdominal ultrasound showed no significant abnormalities.
The patient was temporarily treated with an intravenous drip of levofloxacin hydrochloride and sodium chloride injection (500 mg qd), oral baloxavir marboxil (40 mg) as antiviral therapy, and an intravenous drip of voriconazole (0.2 g q12h) as antifungal therapy. After 5 days, the patient’s fever persisted, accompanied by shivering, and blood culture results remained negative, so antibiotic treatment was subsequently upgraded to an intravenous drip of vancomycin (1000 mg q12h) combined with voriconazole. The patient continued to experience intermittent fever, and a chest CT performed on March 12, 2024 (Figure 1B), yielded results similar to those previously observed. On March 13, bronchoalveolar lavage fluid (BALF) collected by bronchoscopy was subjected to mNGS testing, according to a previous study.5 Ultimately, the mNGS result indicated that the sequence number of S. aureus was 411817, with coverage of S. aureus detected in the BALF sample as shown in Figure 3. The drug-resistant genes identified via mNGS are presented in Table 1. The mNGS results were subsequently confirmed by tNGS testing using the same BALF sample. Based on the patient’s clinical presentation of high fever with shivering, abnormal laboratory results, a recent diagnosis of diabetes with ulcerated skin, and characteristic imaging findings of multiple abscesses in both lungs, a diagnosis of hematogenous lung abscesses caused by multidrug-resistant S. aureus was made. Based on drug-resistant phenotype testing by mNGS, we continued treating the patient with vancomycin as anti-infective therapy, and an intravenous drip of methylprednisolone sodium succinate (40 mg qd) was administered for 3 days to inhibit the inflammatory response. The patient’s temperature returned to normal, his symptoms improved significantly, and he was discharged on March 18, 2024. The patient was prescribed 600 mg of oral linezolid every 12 hours after discharge and instructed to undergo weekly testing for routine blood parameters. Following more than half a month of treatment with oral linezolid, the patient’s clinical symptoms improved. Furthermore, a chest CT performed on April 7, 2024 (Figure 1C) showed that the previously observed multiple nodules and patchy areas of increased density in both lungs, along with gas density shadows and pleural effusion, had significantly reduced relative to those seen on March 12, 2024. However, routine blood results indicated a significant decrease in platelets (from 198×109/L to 99×109/L). Consequently, linezolid was discontinued, and 800 mg of oral contezolid was administered every 12 hours as an alternative treatment. After 14 days, the patient’s clinical condition and imaging findings (Figure 1D) improved, and platelet counts returned to normal (176×109/L). Figure 4 summarizes the timeline of the patient’s diagnosis, treatment, and follow-up.
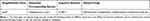 |
Table 1 List of Drug-Resistant Genes Detected by mNGS |
 |
Figure 3 Coverage of Staphylococcus aureus detected by mNGS in BALF sample. |
 |
Figure 4 Timeline of the patient’s diagnosis, treatment, and follow-up. |
Discussion
Hematogenous lung abscesses typically present with systemic symptoms of sepsis, such as chills and hyperpyrexia, due to primary lesions. Lung symptoms such as cough and expectoration usually appear after a few days to 2 weeks, whereas pulmonary signs are often negative. Imaging examinations often show multiple scattered small patchy foci of inflammation or well-defined spherical lesions at the edges of one or both lungs, with visible pus cavities and fluid levels inside. The pathogenic bacteria commonly implicated are S. aureus, S. epidermidis, and Streptococcus. For initial empiric antibiotic therapy, β-lactamase–resistant penicillin or cephalosporin can be selected. For methicillin-resistant S. aureus (MRSA), vancomycin or linezolid are preferred. Given the high risk of relapse with short-term treatment, the antibiotic course for lung abscesses is generally around 4–6 weeks and should continue until chest imaging shows resolution of the abscess or stable small lesions.6 Treatment should be adjusted based on the clinical and radiographic response of the patient.7 Although the patient’s condition improved after the use of linezolid, severe thrombocytopenia occurred, prompting a switch to contezolid, and until. By April 21, 2024, the medication was discontinued based on the patient’s follow-up results. The most common cause of lung abscesses is aspiration of oral secretions by patients with reduced consciousness;8 however, the patient did not have a history of aspiration. In the case of negative blood cultures, mNGS and tNGS were utilized to detect pathogenic microorganisms. The patient presented with high fever and shivering, abnormal laboratory results, recently diagnosed diabetes with ulcerated skin, and characteristic imaging findings of multiple abscesses in both lungs. This led to the diagnosis of hematogenous lung abscesses caused by multidrug-resistant S. aureus, an opportunistic pathogen and one of the leading causes of life-threatening bloodstream infections that colonizes the human anterior nares, skin, and throat under normal physiological conditions.9 S. aureus is implicated in various clinical syndromes, ranging from acute sepsis to more persistent chronic infections of the endocardium, lungs, marrow, skin, and soft tissues.10 The main risk factors for the development of S. aureus sepsis include age, additional comorbidities (such as heart diseases, diabetes, renal disease, and HIV infection), the presence of indwelling medical devices, intravenous drug use, and low socioeconomic status.11 The influenza virus has been identified as a potential predisposing factor for staphylococcal community-acquired pneumonia.12 Additionally, diabetes can increase the risk of S. aureus infection.13 In this case, the infection with S. aureus may have been associated with the recently diagnosed diabetes with ulcerated skin and influenza B virus infection. A study found that in the diabetic lung, normal lung architecture is disrupted, and upregulated expression of TNF-α and IL-6 exerts a pro-inflammatory effect on the lungs, leading to increased apoptosis of lung tissue,14 which may promote the development of lung abscesses. Another possible cause of the lung abscess is aspiration of oral secretions by patients with cerebral hypoplasia. The increasing tolerance of S. aureus to antibiotics makes infections difficult to treat, and morbidity and mortality remain high.15 Therefore, early and rapid diagnosis of pathogenic microorganisms and drug sensitivity tests for infected patients are crucial for guiding clinicians in adjusting antibiotic treatment, which is essential for improving patient outcomes.
Conventional culture-based detection remains the “gold standard” for identifying respiratory pathogens; for instance, blood cultures in patients with hematogenous lung abscesses can reveal pathogenic bacteria, but the sensitivity of blood cultures is suboptimal. Just over one-third of patients with sepsis have positive blood cultures, and it usually takes 3–7 days or longer to identify the potential pathogen.16 Recently, molecular biology detection techniques have gained favor due to their shorter turnaround time and greater sensitivity. Respiratory infections can be diagnosed accurately and early during hospitalization using mNGS and tNGS. mNGS is a microbial identification technique based on high-throughput nucleic acid detection, involving reverse transcription and amplification of pathogenic microbial genomic nucleic acid extracted from clinical samples, followed by comparative analysis using databases. mNGS can detect all pathogens in samples without bias, identify new or rare pathogens,17 and reveal virulence and drug-resistant genes of pathogenic bacteria while being less affected by antimicrobial exposure. However, this technique requires large amounts of sequencing data and analysis, involves high detection costs, and can be influenced by the presence of environmental microorganisms and engineered bacteria.18 tNGS, on the other hand, is a targeted enrichment sequencing technology that combines multiple PCR amplifications with sequencing and has a clear range of target pathogens,19 enabling the detection of low-abundance pathogens with high sensitivity, reducing analysis workload and interference from host genes, shortening measurement time, improving detection efficiency, and lowering costs. However, tNGS can only detect pre-designed pathogens and cannot identify novel or rare pathogens or perform whole-genome analysis.17 Based on this case, next-generation sequencing can help clinicians rapidly identify the pathogenic bacteria and drug-resistant genes, guiding the anti-infective treatment plan. In cases of unknown origin or severe infections, it is recommended to promptly and appropriately apply next-generation sequencing.
Oxazolidinones are a class of synthetic antibiotics characterized by a basic 2-oxazolidinone nucleus, which binds to the 50S ribosomal subunit to inhibit bacterial protein biosynthesis.1 Oxazolidinones are used to treat infections caused by a wide range of multidrug-resistant gram-positive bacteria. Currently, only two oxazolidinone antibiotics are clinically approved: linezolid, which was approved by the US Food and Drug Administration in 2000, and contezolid, which was approved by the China National Medical Products Administration in 2021. The clinical use of linezolid is associated with thrombocytopenia as a common but serious adverse effect, with underlying mechanisms including myelosuppression, immune-mediated platelet destruction20 and abnormal cellular pathway regulation of megakaryocytes, which side effects limit the clinical use of linezolid.21,22 Wang et al4 reported that patients receiving long-term (>3 months) treatment with linezolid often develop intolerable adverse effects, such as peripheral neuropathy, anemia, and pancytopenia due to myelosuppression. Contezolid, as a novel oxazolidinone antibiotic, comprises a 2.3-dihydropyridin-4-one (DHPO) ring in its scaffold, enhancing its antibacterial efficacy while significantly reducing myelosuppression and monoamine oxidase (MAO) inhibition.23 Contezolid has demonstrated strong antibacterial activity against drug-resistant gram-positive pathogens,24 including, but not limited to, methicillin-resistant S. aureus, S. pyogenes, S. agalactiae, and Enterococcus. Its common adverse effects are gastrointestinal diseases.25 Multiple studies have reported1–4 that contezolid can ameliorate the decrease in platelet levels caused by linezolid. Wang K et al reported that a 44-year-old woman with high blood pressure and diabetes was diagnosed with community-acquired pneumonia caused by Staphylococcus aureus and received anti-infective therapy including meropenem, linezolid, teicoplanin and tazocin, but the platelets (PLT) of patient decreased to 54×109/L, finally, contezolid obtained excellent result, with platelet recovery to normal levels and significant improvement in pulmonary imaging.26 Consistent with these findings, we demonstrated that contezolid is a suitable alternative for patients who are intolerant to linezolid. In animal experiments, contezolid has shown antibacterial activity comparable to or slightly superior to that of linezolid.27 Furthermore, contezolid has a lower tendency for spontaneous drug resistance28 and a low potential to trigger drug resistance in S. aureus.29 Therefore, contezolid holds good prospects for clinical application in treating gram-positive bacteria. In clinical practice, due to the high cost of contezolid, clinicians must select drugs based on the patient’s prognosis, medication safety considerations, and economic status while closely monitoring relevant indicators.
Conclusion
Currently, there are no published reports on the potential correlation between congenital cerebral hypoplasia and the occurrence of hematogenous lung abscesses. This is the first case report of a patient with congenital cerebral hypoplasia diagnosed with hematogenous lung abscesses. In this article, by using mNGS and tNGS to detect pathogenic microorganisms, we have achieved early and rapid diagnosis, accurately adjusted antibiotic treatment regimens and improved the patients’ prognosis. This case also demonstrated that contezolid exhibited good tolerance and effective antibacterial activity and ameliorated the symptoms of linezolid-induced thrombocytopenia. However, large-scale randomised controlled trials still need to be conducted to validate the efficacy and safety of contezolid in the treatment of MDR S. aureus-associated lung infections. We also hope this case report provides valuable insights for the diagnosis and treatment of infection-related conditions.
Data Sharing Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.ncbi.nlm.nih.gov/, PRJNA1167654.
Ethics Approval and Informed Consent
The studies involving humans were approved by the ethics committee of the First Affiliated Hospital of Dalian Medical University (Ethics approval number: PJ-KS-BD-2024-12). Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Consent for Publication
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. Additionally, institutional consent for case publication was granted by the First Affiliated Hospital of Dalian Medical University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Almeida D, Li S-Y, Lee J. et al. Contezolid can replace linezolid in a novel combination with bedaquiline and pretomanid in a murine model of tuberculosis. Antimicrob Agents Chemother. 2023;67(12):e0078923. doi:10.1128/aac.00789-23
2. Chen Y, Ren J, Li F, Ye X, Wu Y. The antibiotic therapy containing contezolid successfully treated methicillin-sensitive Staphylococcus aureus infective endocarditis accompanied with cerebrovascular complications. BMC Infect Dis. 2024;24(1):1301. doi:10.1186/s12879-024-10157-x
3. Yang W, Li X, Chen J, et al. Multicentre evaluation of in vitro activity of contezolid against drug-resistant Staphylococcus and Enterococcus. J Antimicrob Chemother. 2024;79(12):3132–3141. doi:10.1093/jac/dkae331
4. Xu Z, Zhang J, Guan T, et al. Case report: successful treatment with contezolid in a patient with tuberculous meningitis who was intolerant to linezolid. Front Med (Lausanne). 2023;10:1224179. doi:10.3389/fmed.2023.1224179
5. Li J, Ge Y, Xin C, Jiang L. Rhino-orbital-cerebral mucormycosis caused by Rhizopus arrhizus diagnosis via metagenomics next-generation sequencing: a case report. Front Cell Infect Microbiol. 2024;14:1375058. doi:10.3389/fcimb.2024.1375058
6. Gonçalves AM, Menezes Falcão L, Ravara L. Pulmonary abcess, a revision. Rev Port Pneumol. 2008;14(1):141–149. doi:10.1016/S0873-2159(15)30223-3
7. Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med. 2015;3(13):183. doi:10.3978/j.issn.2305-5839.2015.07.08
8. Leung CCD, Chan YH, Ho MY, et al. A Single Lung Abscess Caused by Panton-Valentine Leukocidin-Producing Methicillin-Resistant Staphylococcus aureus. Cureus. 2024;16(6):e61845. doi:10.7759/cureus.61845
9. Kwiecinski JM, Horswill AR. Staphylococcus aureus bloodstream infections: pathogenesis and regulatory mechanisms. Curr Opin Microbiol. 2020;53:51–60. doi:10.1016/j.mib.2020.02.005
10. Kahl BC, Becker K, Löffler B. Clinical Significance and Pathogenesis of Staphylococcal Small Colony Variants in Persistent Infections. Clin Microbiol Rev. 2016;29(2):401–427. doi:10.1128/CMR.00069-15
11. Asgeirsson H, Thalme A, Weiland O. Staphylococcus aureus bacteraemia and endocarditis–epidemiology and outcome: a review. Infect Dis (Lond). 2018;50(3):175–192. doi:10.1080/23744235.2017.1392039
12. Hageman JC, Uyeki TM, Francis JS, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003–04 influenza season. Emerg Infect Dis. 2006;12(6):894–899. doi:10.3201/eid1206.051141
13. Zhong J, Wei M, Yang C, et al. Molecular Epidemiology of Community-Acquired Methicillin- Resistant Staphylococcus aureus and Clinical Characteristics of Different Sites of Infection. Infect Drug Resist. 2023;16:1485–1497. doi:10.2147/IDR.S401998
14. Su H, Tian CJ, Wang Y, et al. Ginsenoside Rb1 reduces oxidative/carbonyl stress damage and ameliorates inflammation in the lung of streptozotocin-induced diabetic rats. Pharm Biol. 2022;60(1):2229–2236. doi:10.1080/13880209.2022.2140168
15. Lee J, Zilm PS, Kidd SP. Novel Research Models for Staphylococcus aureus Small Colony Variants (SCV) Development: co-pathogenesis and Growth Rate. Front Microbiol. 2020;11:321. doi:10.3389/fmicb.2020.00321
16. Towns ML, Jarvis WR, Hsueh PR. Guidelines on blood cultures. J Microbiol Immunol Infect. 2010;43(4):347–349. doi:10.1016/S1684-1182(10)60054-0
17. Kuang J, Luo Z, Zhou F. Acute Pulmonary Actinomycosis Induced by Immunotherapy and Chemotherapy Used for SCLC Treatment: a Case Report and Literature Review. Infect Drug Resist. 2023;16:7575–7580. doi:10.2147/IDR.S429699
18. Binghuai L. Basic competence for etiological diagnosis of lower respiratory tract infection after application of metagenomic next-generation sequencing. Chin J Tuberc Respir Dis. 2023;46(4):315–318.
19. Zhang H, Liao Y, Zhu Z, et al. Assistance of next-generation sequencing for diagnosis of disseminated Bacillus Calmette-Guerin disease with X-SCID in an infant: a case report and literature review. Front Cell Infect Microbiol. 2024;14:1341236. doi:10.3389/fcimb.2024.1341236
20. Danese E, Montagnana M, Favaloro EJ, Lippi G. Drug-Induced Thrombocytopenia: mechanisms and Laboratory Diagnostics. Semin Thromb Hemost. 2020;46(3):264–274. doi:10.1055/s-0039-1697930
21. Nishijo N, Tsuji Y, Matsunaga K, et al. Mechanism Underlying Linezolid-induced Thrombocytopenia in a Chronic Kidney Failure Mouse Model. J Pharmacol Pharmacother. 2017;8(1):8–13. doi:10.4103/jpp.JPP_167_16
22. Tajima M, Kato Y, Matsumoto J, et al. Linezolid-induced thrombocytopenia is caused by suppression of platelet production via phosphorylation of myosin light chain 2. Biol Pharm Bull. 2016;39(11):1846–1851. doi:10.1248/bpb.b16-00427
23. Armentano B, Curcio R, Brindisi M, et al. Cappello AR. 5-(Carbamoylmethylene) -oxazolidin- 2-ones as a Promising Class of Heterocycles Inducing Apoptosis Triggered by Increased ROS Levels and Mitochondrial Dysfunction in Breast and Cervical Cancer. Biomedicines. 2020;8(2):35. doi:10.3390/biomedicines8020035
24. Wu X, Li Y, Zhang J, et al. Short-term Safety, Tolerability, and Pharmacokinetics of MRX-I, an Oxazolidinone Antibacterial Agent, in Healthy Chinese Subjects. Clin Ther. 2018;40(2):322–332.e5. doi:10.1016/j.clinthera.2017.12.017
25. Zhao X, Huang H, Yuan H, Yuan Z, Zhang Y. A Phase III multicentre, randomized, double- blind trial to evaluate the efficacy and safety of oral contezolid versus linezolid in adults with complicated skin and soft tissue infections-authors’ response. J Antimicrob Chemother. 2022;77(11):3210–3211. doi:10.1093/jac/dkac282
26. Wang K, Hu Y, Duan Z, et al. Severe Community-Acquired Pneumonia Caused by Methicillin- Sensitive Staphylococcus aureus: successfully Treated with Contezolid - A Case Report and Literature Review. Infect Drug Resist. 2023;16:3233–3242. doi:10.2147/IDR.S406799
27. Li CR, Zhai QQ, Wang XK, et al. In vivo antibacterial activity of MRX-I, a new oxazolidinone. Antimicrob Agents Chemother. 2014;58(4):2418–2421. doi:10.1128/AAC.01526-13
28. Gordeev MF, Yuan ZY. New potent antibacterial oxazolidinone (MRX-I) with an improved class safety profile. J Med Chem. 2014;57(11):4487–4497. doi:10.1021/jm401931e
29. Huang Y, Xu Y, Liu S, et al. Selection and characterisation of Staphylococcus aureus mutants with reduced susceptibility to the investigational oxazolidinone MRX-I. Int J Antimicrob Agents. 2014;43(5):418–422. doi:10.1016/j.ijantimicag.2014.02.008
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Clinical Utility of Contezolid-Containing Regimens in 25 Cases of Linezolid-Intolerable Tuberculosis Patients
Wang J, Nie W, Ma L, Li Q, Geng R, Shi W, Chu N
Infection and Drug Resistance 2023, 16:6237-6245
Published Date: 19 September 2023
Cerebral Abscess Infected by Nocardia gipuzkoensis
Li X, Feng Y, Li D, Chen L, Shen M, Li H, Li S, Wu X, Lu L
Infection and Drug Resistance 2023, 16:7247-7253
Published Date: 15 November 2023
Contezolid Harbored Equivalent Efficacy to Linezolid in Tuberculosis Treatment in a Prospective and Randomized Early Bactericidal Activity Study
Jiang G, Liu R, Xue Y, Ge Q, Nie L, Lv Z, Kong Z, Shi J, Chen H, Li H, Wu X, Xie L, Song Y, Huang H, Gao M
Infection and Drug Resistance 2025, 18:261-268
Published Date: 13 January 2025


