Back to Journals » Advances in Medical Education and Practice » Volume 16
Stress and Interpersonal Relationships in Medical Students During Public Health Emergencies: A Network Analysis
Authors Cui Y , Guo Z, Yang T, Zhang M, Mu H, Li J , Fang J , Du T, Yang X
Received 9 October 2024
Accepted for publication 19 January 2025
Published 28 January 2025 Volume 2025:16 Pages 123—133
DOI https://doi.org/10.2147/AMEP.S495472
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Balakrishnan Nair
Yi Cui,1,* Zhihua Guo,2,* Tianqi Yang,2,3,* Man Zhang,4 Hezi Mu,5 Jiayao Li,1 Jiaxin Fang,6 Tianshu Du,1,2 Xiaomei Yang7
1Department of Nursing, Air Force Medical University, Xi’an, People’s Republic of China; 2Department of Military Medical Psychology, Air Force Medical University, Xi’an, People’s Republic of China; 3 93575 Unit of the Chinese People’s Liberation Army, Chengde, People’s Republic of China; 4Department of Nursing, Shaanxi Provincial People’s Hospital, Xi’an, People’s Republic of China; 5Department of Orthopedics, The Second Affiliated Hospital of Air Force Medical University, Xi’an, People’s Republic of China; 6Department of Nursing, Beijing University of Chinese Medicine, Beijing, People’s Republic of China; 7Department of Gynecology, Shaanxi Provincial People’s Hospital, Xi’an, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tianshu Du, Department of Nursing, Air Force Medical University, Xi’an, 710000, People’s Republic of China, Email [email protected] Xiaomei Yang, Department of Gynecology, Shaanxi Provincial People’s Hospital, Xi’an, 710000, People’s Republic of China, Email [email protected]
Background: With the growing demand for medical services worldwide, especially during public health emergencies, medical students, as a special group of future medical workers, are important for the development of health services, and they therefore experience more stress than ordinary college students do. The mental health of medical students plays a vital role in their training, and interpersonal relationships are an important factor affecting their stress levels.
Purpose: This study aims to investigate the network structure of stress and interpersonal relationships among Chinese medical students and identify bridge variables to prevent and relieve this stress.
Patients and Methods: A self-report measurement taken from the Sociodemographic Questionnaire, Stress Scale for College Students and Interpersonal Relationship Synthetic Diagnosis Test was administered to 322 Chinese medical students from January to April 2022. Network analysis was used to determine the network structure, and the bridge expected influence (BEI) was identified as the bridge variable.
Results: A total of 6.83% of the medical students experienced high levels of stress, and 31.06% of the medical students experienced various degrees of interpersonal distress. The edges across the community associated with stress and interpersonal relationships were all positive. The edges between S1 “personal hassle” and R3 “dealing with people”, S2 “academic hassle” and R2 “socializing”, and S3 “negative life event” and R4 “dating someone of the opposite sex” were the strongest. S1 “personal hassle” had the greatest BEI of the stress community (0.44), and R3 “dealing with people” had the greatest BEI of the interpersonal relationship community (0.19).
Conclusion: This study used network analysis to investigate the relationship between stress and interpersonal relationships in Chinese medical students at the component level for the first time and highlight that the critical bridge variables “personal hassle” and “dealing with people” may contribute to preventing and relieving stress in Chinese medical students.
Keywords: medical students, stress, interpersonal relationship, network analysis, public health emergency
Introduction
As society progresses, the demand for medical services is growing. In particular, in recent years, the coronavirus disease 2019 (COVID-19) pandemic has become a global public health emergency endangering countries worldwide, and many countries are facing a shortage of medical personnel.1,2 Medical students, as a special group of future medical workers, shoulder the responsibility of promoting human health and have become vital to the development of national health services.3 However, owing to the strong professionalism of the curriculum, the wide range of learning subjects, and the length of their academic cycles, medical students face increasingly severe competition in medical environments, tense doctor-patient relationships and other challenges, and they face more mental health problems than ordinary college students do.4,5 Under public health emergencies, the harmfulness and severity of infectious diseases also have a strong impact on the psychology of medical students.6 In severely affected areas, due to the limited number of official medical staff, many medical students must participate in various voluntary activities. However, as students, they still lack certain professional skills, have not been exposed to real medical environments, lack experience in addressing infectious disease emergencies, and lack an adequate understanding of the role of protective measures; consequently, they have many doubts about their immunity and health status.7 Therefore, they experience a high level of psychological stress.8 To train medical students better and compensate for the shortage of medical personnel, there is an urgent need to reduce stress in medical students and prevent mental health problems.
Stress is an individual’s subjective feeling in response to changes in the external environment and the internal state of the body. It is a type of tension caused by biological, spiritual and social environmental stimulus factors.9 Numerous studies have shown that chronic and excessive stress not only has a tremendous effect on the physical health of medical students but also poses a risk to their mental health.10 For example, stress is a risk factor for depression, sleep disturbance, burnout, and reduced well-being.11,12 For medical students, excessive stress can also affect their academic performance, clinical skills and even their future medical careers.13 In the context of a clinical internship or practice, stress may lead to errors in medical care.14 The stress experienced by medical students mainly arises from complex aspects. Under the public health emergency, to control the spread of COVID-19 as quickly as possible, many areas have taken measures to close communities and schools, forcing many students to pursue their studies through online courses and while placing various constraints on their academic life. Research has shown that 34% of medical students experience psychological stress during this process.15 Owing to their profession, many medical students accept the risk of infection to volunteer in hospitals, nucleic acid testing labs or college support services, which then triggers stress.16 More importantly, studies have shown that interpersonal relationships are an important factor influencing the generation of stress among medical students.17 Therefore, alleviating the stress of medical students in a more targeted way from the perspective of interpersonal relationships is essential.
Interpersonal relationships are complex social phenomena and refer to the psychological relationships formed by people through communication and interaction, fulfilling the psychological need for socialization between people.18 Interpersonal relationship problems negatively affect not only life and academics but also physical and mental health.19 Some studies have shown that medical students have more sensitive and complicated interpersonal relationship problems than other students do, and the proportion of problems is as high as 48.2%.20 The stress generated by poor interpersonal relationships is a great source of stress for medical students. On the one hand, college students are in emotionally rich youthful periods and have a strong need for interpersonal interactions, but interpersonal interactions during college are relatively complex, and it is difficult to establish harmonious interpersonal relationships in a short period of time. Moreover, for medical students, doctor-patient relationship issues are inevitable and need to be properly addressed in the context of health care; the stress caused by this type of interpersonal relationship is more obvious.21 On the other hand, the lockdown measures resulting from the pandemic led to a lack of communication, which blocked emotional communication between people. Online meetings and chats are prone to misinterpretations and misunderstandings, exacerbating interpersonal distress and increasing stress.22 Hence, it is important to explore the close relationship between stress and interpersonal relationships to alleviate stress caused by interpersonal relationships.
Previous studies on the relationship between stress and interpersonal relationships are based on the latent variable model, which performs its analysis on the basis of the total score of the scale.18 This approach may overlook the fact that stress and interpersonal relationships are composed of complex components. Stress in medical students is composed of personal hassle, academic hassle and negative life events, as well as interpersonal relationships such as talking, dating someone of the opposite sex, socializing and dealing with people (the way one gets along with others).23,24 Although previous studies have also revealed a strong relationship between stress and interpersonal relationships, it has not been possible to specify a finer-grained pattern of associations among each component. For example, the identification of which key factor of stress or interpersonal relationship that plays the most important role in reducing stress among medical students remains elusive. Consequently, developing targeted plans has become an insurmountable challenge. Therefore, a finer-grained analysis is necessary to understand the potential association correlation paths between the two variables in more detail.
Network analysis is an innovative statistical method that uses a data-driven approach and plays an important role in exploring the finer-grained association paths between two complex related variables. The network is made up of nodes and edges, where nodes represent variables and edges represent the relationships between variables, which makes the results more intuitive and visual.25 In recent years, network analysis has been used in research to help understand such psychological constructs as decision-making, stigma, and resilience.26,27 Therefore, it is both scientific and necessary to apply network analysis in this study. First, stress and interpersonal relationships are two complex psychological constructs with interrelated components, and they can therefore be regarded as an interconnected system. Network analysis allows for a better understanding of both the mental structures and the nodes and edges that are important to the overall system. Second, network analysis compensates for the limitation of analyzing only the whole level on the basis of the latent variable model by exploring the interaction between stress and interpersonal relationships at the component level. Third, network analysis can explain the relationship between stress and interpersonal relationships through a process of partial correlation and regularization, which can effectively prevent the occurrence of related false positives.28 Fourth, compared with the simple correlation method, the network model can reveal the corresponding centrality of each node to test its importance in the whole network. The bridge expected influence (BEI) serves as a crucial indicator in network analysis, representing the cumulative absolute values of all edges connecting this particular node with other nodes within the cluster. A higher BEI value signifies an increased risk of transmission to other nodes within the cluster.29 This centrality index also provides an important potential target for the development of subsequent intervention programs to reduce stress among medical students.30 In conclusion, the application of network analysis can provide not only a more detailed understanding of these relationships at the component level but also a new guiding direction for identifying important targets for intervention.
To the best of our knowledge, no studies have explored the relationship between medical students’ stress and their interpersonal relationships through network analysis. Therefore, the present study aimed to leverage network analysis to fill this research gap by identifying the complex interaction between stress and interpersonal relationships at the component level for the development of more targeted interventions. The above analysis highlights the two primary aims of our study. First, we explore the potential pathways between the various components of medical students’ stress and their interpersonal relationships. Second, the BEI is used to investigate the most influential node, which has the strongest connection within the community of stress and interpersonal relationships. Our findings may provide important guidance for the development of healthy interpersonal relationships among medical students, stress relief and the maintenance of their mental health.
Materials and Methods
Design, Participants and Procedure
This cross-sectional survey was conducted from January to April 2022 during the COVID-19 pandemic in China. We randomly selected the study subjects by school number for each grade level via a convenience sampling method. The sample size was estimated according to Kendall’s31,32 principle, which specifies that the final sample size should be 5–10 times the variable. In this study, the sociodemographic questionnaire contained 8 items, the Stress Scale for College Students contained 3 dimensions, and the Interpersonal Relation Synthetic Diagnosis Test contained 4 dimensions. Hence, the sample size was 75–150 because a total of 15 variables needed to be analyzed. Considering that there may be invalid questionnaires, we increased the sample size by 20%. Finally, 330 questionnaires were sent out in this study, and 322 valid questionnaires were received, with a valid recovery rate of 97.58%.
This study was conducted under the Declaration of Helsinki and approved by the Ethics Committee of the First Affiliated Hospital of Air Force Medical University. Researchers explained the purpose and significance of the study to the participants face-to-face, and the participants signed an informed consent form before completing the questionnaires. There were six participants aged 17 years old (with IDs 2, 9, 20, 25, 36, and 61), and we have also obtained written informed consent from their parents. Every participant completed the questionnaire anonymously and voluntarily. They could withdraw from the study at any time.
Measurement
Sociodemographic Questionnaire
In accordance with the purpose of the study and the literature review, the research team developed a questionnaire to gather sociodemographic information, including gender, age, grade, residence, relationship status, family structure, sibling status and family economic situation.
Stress Scale for College Students
The Stress Scale for College Students (SSCS) is a reliable self-reported scale that measures the stress level of Chinese college students.33 It comprises 30 items that span three subscales, namely, academic hassle, personal hassle, and negative life events. Each item is rated on a scale ranging from 0 = none to 3 = severe. The higher the score is, the higher the stress level is. A score higher than 45 is considered to indicate a high stress level, and a score lower than 45 represents a low stress level. We used Cronbach’s α to assess the internal consistency of personal hassle, academic hassle, negative life events and the total scale in our sample.
Interpersonal Relation Synthetic Diagnosis Test
The Interpersonal Relation Synthetic Diagnosis Test (IRSDT) is a 28-item self-reported measure that assesses interpersonal distress.24,34 It includes four dimensions: talking, socializing, dealing with people, and dating someone of the opposite sex. Each item is rated as 1 = yes or 0 = no, with higher scores indicating higher levels of interpersonal distress. We used Cronbach’s α to assess the internal consistency of talking, socializing, dealing with people, dating someone of the opposite sex, and total scale.
Data Analysis
Network Estimation
The stress‒interpersonal relationship network was constructed and visualized via the qgraph R package.35 We used the Gaussian graphical model (GGM) to estimate the network.36 Within the network, nodes represent a set of items or variables, and edges are undirected and represent the partial correlations between nodes after controlling all other nodes.37 The Spearman correlation test was used in the network construction in this study. The extended Bayesian information criterion (EBIC) combined with the graphical least absolute shrinkage and selector operator (LASSO) method was used to regularize the network. The graphical LASSO eliminates spurious and small between-node partial correlations by shrinking them to zero, which helps to obtain a sparse and easy-to-interpret network.28,38 The hyperparameter of EBIC, which determines the degree of shrinkage, was set to 0.5 to balance the sensitivity and the specificity.39 The network layout was constructed via the Fruchterman-Reingold algorithm.40
Bridge Centrality Estimation
The BEI of a node, which refers to the sum of the edge weights that connect it with all the nodes in the other community, was calculated to determine the dominant bridge nodes. A higher BEI value indicates a greater impact of a node on the other community and a greater likelihood of activating nodes from the other community.29,41 Prior to the analysis, we defined two communities on the basis of theory (ie, the stress and interpersonal relationship communities) rather than on the basis of any specific methods of network analysis, such as community detection.42 We estimated this index via the R package network tools.
Accuracy and Stability Estimation
We used the R package bootnet to estimate the robustness of the network, which ensured the accuracy and replicability of the network analysis.43 The accuracy of the estimated edge was evaluated via a nonparametric bootstrap method (1,000 bootstrap samples) to compute the 95% confidence interval (CI) of the edge weights. The narrower the 95% CI was, the more accurate the edge weights were.44 The stability of the BEI was evaluated via a case-dropping bootstrap approach (1,000 bootstrap samples) to calculate the correlation stability coefficient (CS coefficient). To be considered stable, the CS coefficient needs to be at least 0.25 and preferably above 0.5.43 Furthermore, we used bootstrapped difference tests (1000 bootstrap samples, α = 0.05) to examine the significant differences between edge weights and between BEIs.
Results
Descriptive Statistics
Among the 322 medical college students, 261 were male (81.06%), and 61 were female (18.94%); 84 were freshmen (26.09%), 82 were sophomores (25.47%), 78 were juniors (24.22%), and 78 were seniors (24.22%); 222 students (68.94%) lived in urban areas, and 100 students (31.06%) lived in rural areas. The students ranged from 17 to 23 years old, with an average age of 19.77 years (SD: 1.39). High levels of stress accounted for 6.83%, and 31.06% of medical students experienced various degrees of interpersonal distress. With respect to internal consistency, the Cronbach’s α coefficients were 0.894, 0.925, 0.825 and 0.943 for the dimensions of personal hassle, academic hassle, negative life events and the total stress scale, respectively. The Cronbach’s α coefficients were 0.602, 0.738, 0.612, 0.719 and 0.877 for the dimensions of talking, socializing, dealing with people, dating someone of the opposite sex, and the total interpersonal relationship scale, respectively. The means, standard deviations and BEIs of the nodes in the stress‒interpersonal relationship network are presented in Table 1.
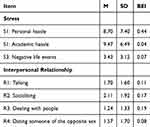 |
Table 1 Means, Standard Deviations and BEIs of Nodes in the stress‒interpersonal Relationship Network (N=322) |
The Stress‒Interpersonal Relationship Network Model
The stress‒interpersonal relationship network model is displayed in Figure 1a. There were 17 edges in the network (with edge weights ranging from 0.01 to 0.42), among which 8 edges crossed the stress and interpersonal relationship communities. Among these intercommunity edges, S1 “personal hassle” was correlated with R1 “talking” (r=0.10), R2 “socializing” (r=0.11), R3 “dealing with people” (r=0.19) and R4 “dating someone of the opposite sex” (r=0.04); S2 “academic hassle” was correlated with R1 “talking” (r=0.01) and R2 “socializing” (r=0.02); and S3 “negative life event” was correlated with R2 “socializing” (r=0.03) and R4 “dating someone of the opposite sex” (r=0.04). In addition, as shown in Figure S1 of the supplementary material, the edge weight of S1 “personal hassle”-R3 “dealing with people” was significantly greater than that of most other intercommunity edges in the network (P<0.05). All the edge weights in the network can be found in Table S1 of the supplementary material.
Bridge Centrality Estimation
The BEIs of nodes in the stress‒interpersonal relationship network are presented in Figure 1b. S1 “personal hassle” had the largest BEI value in the stress community, whereas R3 “dealing with people” had the largest BEI value in the interpersonal relationship community. In addition, the BEI value of S1 “personal hassle” was significantly larger than that of all the other nodes in the network (see Figure S2 in the supplementary material for the results of the difference test of node BEIs).
The results of the accuracy test of edge weights are shown in Figure 2, and a relatively narrow 95% CI revealed accurate calculations of the edge weights in the stress‒interpersonal relationship network. The stability of the BEI in this study was ideal, as shown in Figure 3. With a reduced sampling proportion, there was a slight downward trend in the average correction in the original sample. The CS coefficient of BEI was 0.752, which is greater than 0.5.
 |
Figure 2 Accuracy test of edge weights. |
 |
Figure 3 The stability results of BEI. |
Discussion
In the present study, we examined a complex network of stress and interpersonal relationships in Chinese medical students during the COVID-19 pandemic at the component level. There were several edges that connected nodes between the communities, which suggested that the different dimensions of interpersonal relationships had different potential pathways through which to influence stress. Our study also examined the central nodes that play crucial roles in the stress‒interpersonal relationship network, which can provide insights for more targeted prevention and intervention to reduce stress.
Within the stress and interpersonal relationship network, all edges were positive, which means that the correlation between the dimensions of stress and interpersonal relationships was positive. This finding is consistent with the results of previous studies that explored the relationship between stress and interpersonal relationships.17 The edge between S1 “personal hassle” of the stress community and R3 “dealing with people” of the interpersonal relationships community was the strongest. This finding was similar to that of Totenhagen.45 Personal hassle includes a wide range of life aspects, such as family conditions, the living environment, personal image, and various daily stresses arising from getting along with classmates and teachers. This is also aligned with “dealing with people” in interpersonal relationships. Medical students come from different regions, and because of their different temperaments and personality traits coupled with their different family environments and growth experiences and different living habits and cognitive levels, they adopt different ways of dealing with problems in their academic pursuits and in their lives.46 Moreover, medical students also need to visit the clinic to address doctors, nurses, patients and patients’ families and to handle various medical events, which greatly increases the scope of their interpersonal relationships.47 Especially during the COVID-19 pandemic, the amount of time that medical students spend with classmates has increased significantly, and conflicts often arise in the process of communication.48 Therefore, to alleviate medical students’ personal hassle, schools should carefully consider students’ daily interpersonal interactions, address interpersonal cognitive deficits caused by family background, improve the construction of cognitive concepts regarding the self and others, and enhance interpersonal cognition. The doctor‒patient relationship can be integrated into the curriculum to help students change by adapting their personal perceptions and overcoming their cognitive biases and psychological barriers.49
The BEIs can better reflect the importance of the bridge nodes that play the most central role in activating the whole network. Bridge nodes are the most effective targets for prevention or intervention. In this study, S1 “personal hassle” of the stress community and R3 “dealing with people” of the interpersonal relationship community had the strongest BEI; that is, interventions corresponding to personal hassle and dealing with people are the most effective ways to relieve stress. Personal hassle places the greatest stress on medical students as a whole. Dyrbye50 reported that personal life events have a great impact on medical students, which can easily lead to burnout. In addition, Tang51 reported that various aspects of personal life can even lead to suicidal ideation in medical students. Especially because of containment owing to the pandemic, medical students have become limited in their learning methods, interpersonal relationships and scope of activities and cannot fully express themselves. Personal hassle cannot be understood and alleviated in a timely manner, so it gradually accumulates and leads to an amplification of stress.52 These findings also suggest that medical schools should not limit themselves to supervising medical students to help them master solid professional knowledge and skills but should also focus on their daily living conditions and give full play to the role of college counsellors and life teachers.53 In the event that face-to-face communication becomes impossible due to the pandemic, psychological mailboxes and hotlines should be opened promptly to ensure timely communication between students and teachers. Teachers should also take the initiative to communicate with students’ parents and grasp students’ psychological dynamics from multiple perspectives. In addition, schools can establish psychological profiles for medical students, record their mental history, and conduct screenings in high-stress populations. These strategies can not only relieve stress by helping students address their personal hassle but also provide a reference for ensuring the professional sustainability of future medical students.
Dealing with people is the most direct and effective way to relieve stress among medical students from the perspective of interpersonal relationships. It covers all aspects of interpersonal interaction, including communicating with others and handling events. Interacting with people of different personalities and characteristics is also a cause of conflict and stress, which is consistent with the findings of Ooi.54 This result suggests that alongside professional courses, we can also offer skill courses on the best way to relate to people in the curriculum, strengthen interpersonal relationship education, popularize interpersonal relationship skills, and combine knowledge with practice so that the students can obtain more effective and suitable communication methods.55 To form good interpersonal skills on the basis of knowledge and experience, students can experience the joy of relationships, thus forming a virtuous cycle of interaction. It is also possible to simulate clinical scenarios with doctors, nurses, patients and patients’ families so that medical students can advance from the classroom to reality and adapt to society, thus relieving the stress caused by interpersonal conflicts.
Study Strengths and Limitations
There are several limitations in our study. First, the data for this study were collected through a cross-sectional survey; therefore, causality cannot be determined. It is difficult for us to definitively determine the cause of stress and interpersonal relationships. Longitudinal studies should therefore be conducted. Second, this study established a network showing medical students’ stress and interpersonal relationships in the context a unique public health emergency, that is, during the COVID-19 pandemic, without comparison with the general context. The findings moreover apply only to medical students in China, which may differ from the networks of medical students in other countries. Therefore, the network structure generated in different countries or at different times may be different than that in this study. Third, the intervention targets identified by the results of this study are based on the theory of network analysis. In future studies, we need to conduct case‒control studies to verify the effectiveness of the intervention targets. In addition, the assessment of interpersonal relationships in this study includes a dimension of “dating someone of the opposite sex”. Importantly, this dimension may overlook individuals who are dating someone of the same sex or those who identify as gender fluid, potentially impacting the analysis of their relationships. Therefore, future research should thoroughly consider the diverse characteristics of the population to ensure a more comprehensive and rigorous analysis.
Conclusion
This is the first study that leverages network analysis to reconfirm the close relationship between stress and interpersonal relationships in Chinese medical students during public health emergencies at the component level. More importantly, the critical bridge variables “personal hassle” and “dealing with people” may be helpful in preventing and relieving stress in medical students from the perspective of interpersonal relationships.
Abbreviations
COVID-19, Coronavirus disease 2019; BEI, Bridge expected influence; SSCS, Stress Scale for College Students; IRSDT, Interpersonal Relation Synthetic Diagnosis Test; GGM, Gaussian graphical model; EBIC, Extended Bayesian information criterion; LASSO, Least absolute shrinkage and selector operator; CI, Confidence interval; CS, Correlation stability.
Data Sharing Statement
The datasets used during the study are available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
This study was conducted under the Declaration of Helsinki and approved by the Ethics Committee of the First Affiliated Hospital of Air Force Medical University. Researchers explained the purpose and significance of the study to the participants face-to-face, and the participants signed an informed consent form before completing the questionnaires. There were six participants aged 17 years old (with IDs 2, 9, 20, 25, 36, and 61), and we have also obtained written informed consent from their parents. Every participant completed the questionnaire anonymously and voluntarily. They could withdraw from the study at any time.
Acknowledgments
We are thankful to the students who participated in our study and the teachers at the university who helped us with the data collection. We also thank American Journal Experts (www.aje.com) for English language editing and review services.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The author(s) report no conflicts of interest in this work.
References
1. Korneta P, Chmiel M. Medical staff shortages and the performance of outpatient clinics in Poland during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(22):14827. doi:10.3390/ijerph192214827
2. Emergencies: international health regulations and emergency committees. 2021. Available from: https://www.who.int/news-room/q-a-detail/emergencies-international-health-regulations-and-emergency-committees.
3. Tempski P, Arantes-Costa FM, Kobayasi R, et al. Medical students’ perceptions and motivations during the COVID-19 pandemic. PLoS One. 2021;16(3):e0248627. doi:10.1371/journal.pone.0248627
4. Srikhamjak T, Yanawuth K, Sucharittham K, et al. Impact of the COVID-19 pandemic on mental health and lifestyle in Thai occupational therapy students: a mixed method study. Eur J Investig Health Psycho Educ. 2022;12(11):1682–1699. doi:10.3390/ejihpe12110118
5. Pinho R, Costa TF, Silva NM, et al. High prevalence of burnout syndrome among medical and nonmedical residents during the COVID-19 pandemic. PLoS One. 2022;17(11):e0267530. doi:10.1371/journal.pone.0267530
6. Kosendiak AA, Adamczak B, Bania J, Kontek S. Stress levels, attitude toward vaccination and personal protective equipment of students at Wroclaw medical university during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(21):13860. doi:10.3390/ijerph192113860
7. Norton EJ, Georgiou I, Fung A, Nazari A, Bandyopadhyay S, Saunders KEA. Personal protective equipment and infection prevention and control: a national survey of UK medical students and interim foundation doctors during the COVID-19 pandemic. J Public Health. 2021;43(1):67–75. doi:10.1093/pubmed/fdaa187
8. Arima M, Takamiya Y, Furuta A, Siriratsivawong K, Tsuchiya S, Izumi M. Factors associated with the mental health status of medical students during the COVID-19 pandemic: a cross-sectional study in Japan. BMJ open. 2020;10(12):e043728. doi:10.1136/bmjopen-2020-043728
9. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):
10. Simegn W, Yohannes L, Seid AM, et al. Perceived stress and associated factors among university students in Ethiopia during the late stage of the COVID-19 pandemic: a cross-sectional study. Front Psychol. 2022;13:978510. doi:10.3389/fpsyg.2022.978510
11. Fernandes ACA, Padilha DMM, de Moura A, de Aquino CEF, Lima IBA, Mota-Rolim SA. COVID-19 pandemic decreased sleep quality of medical students. Sleep Sci. 2022;15(4):436–440. doi:10.5935/1984-0063.20220075
12. D’Eon MF, Waller J, Stacey A, et al. Medical student stress, burnout, and workplace factors. Can Med Edu J. 2022;13(5):116–117. doi:10.36834/cmej.75327
13. Vaz M, Sumithra S, Ravindra R, Chandran S, Ramachandra S, Timms O. The Covid-19 effect on medical students’ perceptions of their profession: a mixed methods study from South India. Indian J Med Ethics. 2023;VIII(3):184–195. doi:10.20529/IJME.2022.070
14. Wielewska MK, Godzwon JM, Gargul K, et al. Comparing students of medical and social sciences in terms of self-assessment of perceived stress, quality of life, and personal characteristics. Front Psychol. 2022;13:815369. doi:10.3389/fpsyg.2022.815369
15. Peng P, Hao Y, Liu Y, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2023;21:167–181. doi:10.1016/j.jad.2022.10.040
16. Büssing A, Lindeberg A, Stock-Schröer B, Martin D, Scheffer C, Bachmann HS. Motivations and experiences of volunteering medical students in the COVID-19 pandemic-results of a survey in Germany. Front Psychiatry. 2021;12:768341. doi:10.3389/fpsyt.2021.768341
17. Kang K, Lee M, Cho H. Interpersonal skills mediate the relationship between communicative and clinical competencies among nursing students: a descriptive study. Nurse Educ Today. 2021;99:104793. doi:10.1016/j.nedt.2021.104793
18. Zhou E, Ma S, Kang L, et al. Psychosocial factors associated with anxious depression. J Affect Disord. 2022;322:39–45. doi:10.1016/j.jad.2022.11.028
19. Huang ZH, Wang N. Empirical analysis based on the related factors of college students’ mental health problems. Front Psychol. 2022;13:997910. doi:10.3389/fpsyg.2022.997910
20. Wei M, Zhao D, Wang WQ, Ni JL. International skills of undergraduate in medical university. China J Health Psychol. 2013;21(09):1416–1418. doi:10.13342/j.cnki.cjhp.2013.09.032
21. Egnew TR, Wilson HJ. Faculty and medical students’ perceptions of teaching and learning about the doctor-patient relationship. Patient Edu Couns. 2010;79(2):199–206. doi:10.1016/j.pec.2009.08.012
22. Gupta A, Jagzape A, Kumar M. Social media effects among freshman medical students during COVID-19 lock-down: an online mixed research. J Educ Health Promot. 2021;10:55. doi:10.4103/jehp.jehp_749_20
23. Li H, Lin CD, Bray MA, Kehle TJ. The measurement of stressful events in Chinese college students. Psychol Sch. 2005;42(3):315–323. doi:10.1002/pits.20082
24. Zheng R. Psychological Diagnosis of College Students. Shandong, China: Shandong Education Press; 1999:339–345.
25. Fried EI, Cramer AOJ. Moving forward: challenges and directions for psychopathological network theory and methodology. Perspect Psychol Sci. 2017;12(6):999–1020. doi:10.1177/1745691617705892
26. Peng J, Ren L, Yang N, Zhao L, Fang P, Shao Y. The network structure of decision-making competence in Chinese adults. Front Psychol. 2020;11:563023. doi:10.3389/fpsyg.2020.563023
27. Wei Z, Ren L, Liu C, Cao M, Yang Q, Deng Y. The concept map of felt stigma in patient with epilepsy. Seizure. 2020;80:138–142. doi:10.1016/j.seizure.2020.06.019
28. Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. 2018;23(4):617–634. doi:10.1037/met0000167
29. Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2021;56(2):353–367. doi:10.1080/00273171.2019.1614898
30. Stochl J, Soneson E, Wagner AP, Khandaker GM, Goodyer I, Jones PB. Identifying key targets for interventions to improve psychological wellbeing: replicable results from four UK cohorts. Psychol Med. 2019;49(14):2389–2396. doi:10.1017/S0033291718003288
31. Kendall M. Multivariate Analysis. Charles Griffin and Company Limited; 1975.
32. Ni P, Chen L, Liu N. The sample size estimation in quantitative nursing research. Chin J Nurs. 2010;45:378–380. doi:10.3761/j.issn.0254-1769.2010.04.037
33. Li H, Mei JR. Development of stress scale for college student. Chin J Applied Psychol. 2002;23(8):27–32. doi:10.3969/j.issn.1006-6020.2002.01.005
34. Yang Q, Shi M, Zeng L, Xu P. University freshmen’s excessive smartphone use and psychological safety during the COVID-19 pandemic. Front Psychiatry. 2022;13:993555. doi:10.3389/fpsyt.2022.993555
35. Epskamp S, Cramer A, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;48:367–371. doi:10.1037/met0000167
36. Epskamp S, Waldorp L, Mõttus R, Borsboom D. The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behav Res. 2018;53(4):453–480. doi:10.1080/00273171.2018.1454823
37. Bhushan N, Mohnert F, Sloot D, Jans L, Albers C, Steg L. Using a Gaussian graphical model to explore relationships between items and variables in environmental psychology research. Front Psychol. 2019;10:1050. doi:10.3389/fpsyg.2019.01050
38. Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9(3):432–441. doi:10.1093/biostatistics/kxm045
39. Foygel R, Drton M. Extended Bayesian information criteria for Gaussian graphical models. Adv Neural Inf Process Syst. 2010;23:2020–2028. doi:10.48550/arXiv.1011.6640
40. Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Software Pract Exper. 1991;21:1129–1164. doi:10.1002/spe.4380211102
41. Guo Z, He Y, Yang T, et al. The roles of behavioral inhibition/activation systems and impulsivity in problematic smartphone use: a network analysis. Front Public Health. 2022;10:1014548. doi:10.3389/fpubh.2022.1014548
42. Hoffman M, Steinley D, Gates KM, Prinstein MJ, Brusco MJ. Detecting clusters/communities in social networks. Multivariate Behav Res. 2018;53(1):57–73. doi:10.1080/00273171.2017.1391682
43. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50(1):195–212. doi:10.3758/s13428-017-0862-1
44. Mullarkey MC, Marchetti I, Beevers CG. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. 2019;48(4):656–668. doi:10.1080/15374416.2018.1437735
45. Totenhagen CJ, Serido J, Curran MA, Butler EA. Daily hassles and uplifts: a diary study on understanding relationship quality. J Fam Psychol. 2012;26(5):719–728. doi:10.1037/a0029628
46. Hur Y, Cho AR, Huh S, Kim S. How do medical students differ in their interpersonal needs? BMC Med Educ. 2017;17(1):42. doi:10.1186/s12909-017-0870-y
47. Davis BP, Clevenger C, Dillard R, Moulia D, Ander DS. “Disbelief and sadness”: first-year health profession students’ perspectives on medical errors. J Patient Saf. 2021;17(8):e1901–e1905. doi:10.1097/PTS.0000000000000691
48. Cheng T, Lin Q, Fu H. A comparative study of subjective well-being, interpersonal relationship and love forgiveness among Chinese college students before and after the COVID-19 epidemic. Front Psychol. 2023;14:1229451. doi:10.3389/fpsyg.2023.1229451
49. Deinzer R, Kiupel S, Weik U. Endocrine and psychological stress response in simulated doctor‒patient interactions in medical education. Psychoneuroendocrinology. 2019;105:172–177. doi:10.1016/j.psyneuen.2018.09.028
50. Dyrbye LN, Thomas MR, Huntington JL, et al. Personal life events and medical student burnout: a multicenter study. Acad Med. 2006;81(4):374–384. doi:10.1097/00001888-200604000-00010
51. Tang W, Kang Y, Xu J, Li T. Associations of suicidality with adverse life events, psychological distress and somatic complaints in a Chinese medical student sample. Community Ment Health J. 2020;56(4):635–644. doi:10.1007/s10597-019-00523-4
52. Ford MB. Social distancing during the COVID-19 pandemic as a predictor of daily psychological, social, and health-related outcomes. J Gen Psychol. 2021;148(3):249–271. doi:10.1080/00221309.2020.1860890
53. Bashir MBA, Mohamed SOA, Nkfusai CN, et al. Assessment of minor psychiatric morbidity, stressors, and barriers of seeking help among medical students at the University of Khartoum, Khartoum, Sudan. Pan Afr Med J. 2020;35:87. doi:10.11604/pamj.2020.35.87.17512
54. Ooi PB, Khor KS, Tan CC, Ong DLT. Depression, anxiety, stress, and satisfaction with life: moderating role of interpersonal needs among university students. Front Public Health. 2022;10:958884. doi:10.3389/fpubh.2022.958884
55. Ruiz-Moral R, Gracia de Leonardo C, Caballero Martínez F, Monge Martín D. Medical students’ perceptions towards learning communication skills: a qualitative study following the 2-year training programme. Int J Med Educ. 2019;10:90–97. doi:10.5116/ijme.5cbd.7e96
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


