Back to Journals » Journal of Hepatocellular Carcinoma » Volume 12
Treatment Outcomes of Systemic Therapies for Infiltrative Hepatocellular Carcinoma
Authors Chen PY , Chang CK, Chen BB, Hsu CH, Cheng AL, Shao YY
Received 18 March 2025
Accepted for publication 19 June 2025
Published 23 June 2025 Volume 2025:12 Pages 1221—1229
DOI https://doi.org/10.2147/JHC.S528897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Mohamed Shaker
Po-Yi Chen,1,2 Chih-Kai Chang,3 Bang-Bin Chen,3 Chih-Hung Hsu,1,2,4 Ann-Lii Cheng,1,2,4 Yu-Yun Shao1,2,4
1Department of Medical Oncology, National Taiwan University Cancer Center, Taipei, Taiwan; 2Department of Oncology, National Taiwan University Hospital, Taipei, Taiwan; 3Department of Medical Imaging, National Taiwan University Hospital, Taipei, Taiwan; 4Graduate Institute of Oncology, College of Medicine, National Taiwan University, Taipei, Taiwan
Correspondence: Yu-Yun Shao, Department of Oncology, National Taiwan University Hospital, 7 Chung-Shan South Road, Taipei, 10002, Taiwan, Tel +886 2 23123456 ext. 266008, Fax +886 2 23711174, Email [email protected]
Purpose: Outcomes in the treatment of unresectable infiltrative hepatocellular carcinoma (HCC) are poorly understood, and infiltrative HCC is generally underrepresented in clinical trials. The present study explored outcomes associated with the treatment of infiltrative HCC with various systemic therapies.
Patients and Methods: We enrolled all patients with Barcelona Clinic Liver Cancer stage C infiltrative or multinodular HCC who received first-line systemic therapy between January 2015 and December 2021 at a single center. We compared baseline characteristics and treatment outcomes for the two HCC subtypes.
Results: In total, 260 patients were enrolled, 128 (49.2%) of whom had infiltrative HCC. Patients with infiltrative HCC were more likely to have macrovascular invasion (91.4% vs 68.2%, p < 0.001) but less likely to have extrahepatic spread (32.0% vs 54.5%, p < 0.001) than patients with multinodular HCC. In patients who received multikinase inhibitors alone, the time to treatment failure (TTF) and overall survival (OS) were similar for the 2 HCC subtypes. In patients who received immune checkpoint inhibitor (ICI)-based therapy, multivariate analyses revealed that infiltrative HCC was associated with shorter TTF (HR: 4.07, 95% CI: 2.13– 7.79, p < 0.001) and poorer OS (HR: 3.27, 95% CI: 1.76– 6.11, p < 0.001).
Conclusion: In patients receiving ICI-based therapy for HCC, infiltrative HCC was associated with poorer outcomes.
Keywords: hepatocellular carcinoma, HCC, infiltrative, systemic therapy, multikinase inhibitor, immune checkpoint-inhibitor
Introduction
Liver cancer is the sixth most common cancer and the third leading cause of cancer-related deaths worldwide. Hepatocellular carcinoma (HCC) accounts for 75% to 85% of liver cancer cases.1 Patients with HCC present with single nodular, multinodular, or infiltrative patterns.2 Infiltrative type of HCC, which accounts for 8% to 18% of HCC cases and is notable for its microscopic spread across the liver parenchyma and blood vessels, often presents in imaging with characteristics such as an incomplete or absent capsule and indistinct demarcation and is frequently associated with portal vein tumor thrombus.3 Few studies have compared the characteristics of infiltrative HCC with those of the more common nodular HCC.4,5
Infiltrative HCC is difficult to detect from the background of cirrhosis using ultrasound because of its borderless and infiltrative appearance. Consequently, the diagnosis of infiltrative HCC tends to be delayed until the tumor has progressed to an advanced stage. Accordingly, compared with patients with nodular HCC, those with infiltrative HCC are less likely to receive curative treatment, which typically involves surgical resection, liver transplantation, or local ablation.6,7 The overall survival (OS) rate for infiltrative HCC is worse than that for other HCC subtypes; at advanced stages, OS without treatment is only 1.5 to 3 months.8,9
The treatment options for advanced HCC include sorafenib, lenvatinib, and combination immunotherapies such as bevacizumab plus atezolizumab and durvalumab plus tremelimumab.10–15 Patients with infiltrative HCC are usually underrepresented in clinical trials because they do not have measurable lesions. Historically, the multikinase inhibitor (MKI) sorafenib had been the standard first-line therapy for advanced HCC.10,16–18 Unfortunately, MKIs have limited efficacy against infiltrative HCC. A retrospective study (n = 40) reported a median OS of only 4 months among patients with infiltrative HCC receiving an MKI.19 Data regarding the effectiveness of combination immunotherapies for infiltrative HCC are lacking. This study examined the efficacy of systemic therapies for the treatment of infiltrative HCC. Patients with multinodular HCC were also included for comparison.
Methods and Patients
Patients
We enrolled all patients with Barcelona Center Liver Cancer (BCLC) stage C infiltrative or multinodular HCC who received first-line systemic therapies, between January 2015 and December 2021 at National Taiwan University Hospital (NTUH) in Taipei, Taiwan. HCC diagnoses were based on the American Association for the Study of Liver Disease criteria.20 Infiltrative HCC was defined as HCC involving nonnodular and nonencapsulated lesions with a margin poorly demarcated on computed tomography or magnetic resonance imaging (Figure S1). One radiologist and one medical oncologist independently reviewed all imaging results to determine whether tumors were infiltrative. Disagreement was resolved through consultation with another radiologist not informed of the initial determinations. All investigators were blinded to clinical outcomes. Systemic therapies included MKIs (sorafenib or lenvatinib) alone, immune checkpoint inhibitor (ICI) monotherapy, and combination immunotherapies (atezolizumab plus bevacizumab, MKI plus ICI, or dual ICIs).
Patients who completed at least 3 clinical visits after the initiation of systemic treatment were included for analysis. Patients were excluded if they received simultaneous locoregional therapy or an early-phase investigational agent or if they had a diagnosis of HCC harboring sarcomatoid differentiation, combined cholangiocarcinoma, or double cancer.
Data Collection
We reviewed the medical records of the enrolled patients to obtain demographic information, clinical history, laboratory data, and imaging results. This study was approved by the Institutional Review Board of NTUH. The last follow-up date was December 31, 2022.
Statistical Analysis
Frequency tables were generated for categorical variables. Continuous variables are presented as means and standard deviations. The chi-square test or Fisher’s exact test was used to analyze between-group differences in nominal variables, and the independent t test or Mann–Whitney U-test was used to analyze continuous variables. For univariate survival analysis, the Kaplan–Meier method with the Log rank test was employed. A Cox proportional hazards model was used for multivariate analysis. All statistical analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC, USA). A two-sided p value of ≤ 0.05 was considered statistically significant.
Time to treatment failure (TTF) was defined as the interval between treatment initiation and discontinuation due to disease progression, an adverse event, or death. OS was defined as the interval between treatment initiation and the time of death.
Results
Patient Characteristics
A total of 899 patients who received first-line therapy for BCLC stage C HCC were initially identified. After screening, 260 patients were included in our analysis (Figure S2). Most of the patients had hepatitis B virus–induced HCC (65%), Child-Pugh class A (61.9%) liver reserve, tumor involvement of more than 50% of the liver parenchyma (62.7%), and a serum alpha-fetoprotein level of ≥ 400 ng/mL (60.0%; Table 1). These findings reflect the hepatitis B virus–predominant nature of HCC in Taiwan and the advanced tumor stage with impaired liver reserve of this patient cohort.
 |
Table 1 Patient Characteristics |
Interobserver disagreement regarding imaging interpretation was achieved for 39 (15%) patients. Regarding HCC morphology, HCC was infiltrative in 128 (49.2%) patients, and multinodular in 132 (50.8%) patients. Patients with infiltrative HCC, were more likely to be male (86.7% vs 74.2%, p = 0.011), and have macrovascular invasion (91.4% vs 68.2%, p < 0.001), main portal vein thrombosis (52.3% vs 22.0%, p < 0.001), and a shorter time from diagnosis to first systemic treatment (7.3 weeks vs 10.7 weeks, p = 0.040). Extrahepatic spread was less common in patients with infiltrative HCC than in patients with multinodular HCC (32.0% vs 54.5%, p < 0.001). Patients with infiltrative HCC also had a lower mean platelet level than did patients with multinodular HCC (203.6 vs 253.6 K/µL, p = 0.001; Table 1).
Most patients in both the morphology subtype groups received a MKI alone as their first-line systemic treatment (68.5%). The type of systemic therapy used was similar between patients with multinodular versus infiltrative HCC (Table 1). Subsequent treatments were administered to 111 patients (42.7%).
Clinical Outcomes of Systemic Treatments
Patients with infiltrative HCC had significantly shorter TTF (median 1.6 vs 2.3 months, p = 0.018; Figure 1A) than did patients with multinodular HCC but had similar OS (median 3.4 vs 4.6 months, p = 0.184; Figure 1B). In multivariate analysis, infiltrative HCC was an independent predictor of shorter TTF (HR: 1.34; 95% CI: 1.00–1.78; p = 0.049; Table 2) and was borderline significant in predicting a shorter OS (HR: 1.30; 95% CI: 0.96–1.75; p = 0.092; Table 2). These results suggest that infiltrative HCC has poor response to treatment even after controlling other potential factors.
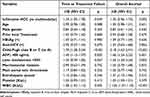 |
Table 2 Multivariate Analysis for Predictors of Time to Treatment Failure and Overall Survival for All Patients |
In patients receiving an MKI alone as a first-line therapy, median TTF (2.0 vs 2.2 months, p = 0.895) and OS (4.5 vs 3.8 months, p = 0.326) were similar in the infiltrative and multinodular HCC groups (Figure 2A and B). By contrast, in patients who received ICI-based treatment as first-line therapy, those with infiltrative HCC had a significantly shorter median TTF (1.3 vs 4.9 months, p < 0.001; Figure 2C) and OS (2.0 vs 10.9 months, p < 0.001; Figure 2D) than did those with multinodular HCC. In multivariate analysis of the outcomes for these patients, infiltrative HCC remained an independent predictor of a shorter TTF (HR: 4.07; 95% CI: 2.13–7.79; p < 0.001) and OS (HR: 3.27; 95% CI: 1.76–6.11, p < 0.001; Table 3).
 |
Table 3 Multivariate Analysis for Predictors of Time to Treatment Failure and Overall Survival for Patients Receiving Immune-Checkpoint-Inhibitor-Based Treatments |
Clinical Outcomes of ICI Monotherapy versus Combination Immunotherapies
ICIs may be used alone or in combination with bevacizumab, an MKI, or another ICI. In the current study, when combination immunotherapies were used, the median TTF (1.6 vs 6.4 months, p < 0.001) and OS (4.8 vs 15.1 months, p < 0.001) were shorter for patients with infiltrative HCC than for patients with multinodular HCC. By contrast, when ICI monotherapy was used, the median TTF (0.5 vs 1.4 months, p = 0.276) and OS (1.0 vs 1.7 months, p = 0.473) were similar in the two groups. However, patients with infiltrative HCC who received combination immunotherapy still had a longer median TTF (1.6 vs 0.5 months, p = 0.013) and longer OS (4.8 vs 1.0 months, p = 0.051) than did patients who received ICI monotherapy (Figure 3A and B). In 46 patients with Child-Pugh class A liver function who received combination immunotherapy, the differences remained in median TTF (1.7 vs 8.0 months, p < 0.001) and OS (3.9 vs 15.6 months, p < 0.001) between the HCC subtype groups (Figure S3).
Discussion
This study discovered treatment outcomes differences based on HCC morphology subtype (infiltrative vs multinodular HCC). Patients who received ICI-based therapies had different TTF and OS, depending on their tumor’s morphology, whereas patients who received a MKI did not. Moreover, this difference was more pronounced in patients who received combination immunotherapies. These findings indicate that the 2 morphology subtypes have distinct tumor biology and microenvironments that affect the efficacy of immunotherapies. To our knowledge, this is the first study to report such findings.
Other retrospective studies have indicated that infiltrative HCC accounts for only 8% to 18% of all HCC cases.4,5 In the present study, among advanced HCC cases in particular, the infiltrative and multinodular HCC subtypes were represented nearly equally (49.2% vs 50.8%). The higher prevalence of infiltrative HCC in patients with advanced HCC than in non-advanced HCC reflects the greater difficulty of obtaining an early diagnosis and the associated lower likelihood that curative therapy will be initiated in cases of infiltrative HCC than in cases of nodular HCC. Moreover, this disparity in patient composition also disclosed the difference between real-world practice and clinical trials.
Several mechanisms may account for the prognostic differences observed between infiltrative and multinodular HCC treated with ICIs. First, the immunosuppressive tumor microenvironment may hinder antitumor immunity through the accumulation of regulatory T cells, inhibitory B cells, myeloid-derived suppressor cells, and M2-polarized tumor-associated macrophages.21 Second, HCC cells harboring β-catenin mutations may exhibit reduced lymphocyte infiltration and resistance to PD-1 blockade.22 Other tumor cell–intrinsic mechanisms have also been implicated in ICI resistance, examples include insufficient expression of tumor-specific neoantigens23 and compromised antigen processing and presentation due to loss of heterozygosity in human leukocyte antigen alleles.24 These potential mechanisms have all been tested in patients with HCC. Nevertheless, studies focused specifically on infiltrative HCC are lacking.
In the current study, ICI monotherapy was not superior to MKIs in terms of improving OS. Adding bevacizumab or a MKI to a ICI or employing dual ICI therapy may counteract the immunosuppressive tumor microenvironment25 and increase the likelihood of a tumor response, thereby improving survival.12,15,26 Our study revealed that although patients with infiltrative HCC and those with multinodular HCC both derived benefits from combination immunotherapy, patients with infiltrative HCC exhibited less improvement (in terms of both TTF and OS). This may be attributable to diminished T cell infiltration, T cell exhaustion, an increase in regulatory T cells, and downregulation of natural killer cell activators.27 Further research is required to elucidate the distinct microenvironmental differences between these HCC subtypes to develop innovative combination therapies that enhance immune responsiveness.
Our study has several limitations. First, this was a retrospective study conducted at a single center without a validation cohort. Further validation through multicenter prospective studies is needed. Second, a substantial proportion of the included patients received MKI monotherapy, which is now considered merely an alternative first-line therapy. Third, multiple regimens of combination immunotherapy were used. Nevertheless, this study obtained an interesting finding that has not been reported in the literature on this often-ignored disease subtype.
Conclusion
Among patients receiving ICI-based therapy for HCC, those with infiltrative HCC have poorer treatment outcomes than those with multinodular HCC. This association may be limited to combination immunotherapy. The underlying mechanism warrants further exploration.
Data Sharing Statement
All data generated or analyzed during this study are included in this article and its online supplementary material files. Further enquiries can be directed to the corresponding author.
Ethics Approval Statement
The study protocol conformed to the ethical guidelines of the 2013 Declaration of Helsinki and the 2018 edition of the Declaration of Istanbul; it was approved by the Institutional Review Board of National Taiwan University Hospital (202211099RINB). Formal consent by written signature was not required for this type of study due to the retrospective nature of anonymous clinical data use, based on the Ethical Guidelines for Medical and Biological Research Involving Human Subjects in Taiwan. No transplant patients were included in this study.
Funding
This study was supported by grants from the Ministry of Science and Technology, Taiwan (MOST-105-2314-B-002-194, MOST 106-2314-B-002-213, MOST-108-2314-B-002-072-MY3, and MOST-111-2314-B-002-120), National Science and Technology Council, Taiwan (NSC-112-2314-B-002-267, NSC 113-2314-B-002 −001, and NSC-113-2923-B-002-001-MY3), Ministry of Health and Welfare (MOHW112-TDU-B-211-144002), National Taiwan University Hospital (NTUH. 105-S2954, and NTUH. 108-S4150) and National Taiwan University Cancer Center (NTUCCS-113-26).
Disclosure
Dr Chih-Hung Hsu reports grants and/or personal fees for (1) institutional grants for sponsor-initiated clinical trials; (2) honoraria for lectures; (3) participating in advisory boards from Roche, AstraZeneca, Merck Sharp & Dohme, Eisai, and Surface Oncology, outside the submitted work. Dr Ann-Lii Cheng reports personal fees for advisory/ consultancy, speaker bureau and/or travel from AstraZeneca, Bayer, Bristol Myers Squibb, Genentech/Roche, Ipsen Innovation, Eisai, Ono Pharmaceutical, Sanofi, Omega Therapeutics, MSD, Amgen Taiwan, and Pilatus Biosciences Inc.; independent director of TTY Biopharma; participation on a data safety monitoring board for Abbisko, outside the submitted work. The authors declare no other conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Trevisani F, Caraceni P, Bernardi M, et al. Gross pathologic types of hepatocellular carcinoma in Italian patients. Relationship with demographic, environmental, and clinical factors. Cancer. 1993;72(5):1557–1563. doi:10.1002/1097-0142(19930901)72:5<1557::AID-CNCR2820720512>3.0.CO;2-5
3. Reynolds AR, Furlan A, Fetzer DT, et al. Infiltrative hepatocellular carcinoma: what radiologists need to know. Radiographics. 2015;35(2):371–386 doi:10.1148/rg.352140114
4. Benvegnù L, Noventa F, Bernardinello E, Pontisso P, Gatta A, Alberti A. Evidence for an association between the aetiology of cirrhosis and pattern of hepatocellular carcinoma development. Gut. 2001;48(1):110–115 doi:10.1136/gut.48.1.110
5. Lopez RR, Pan SH, Hoffman AL, et al. Comparison of transarterial chemoembolization in patients with unresectable, diffuse vs focal hepatocellular carcinoma. Arch Surg. 2002;137(6):653–657 doi:10.1001/archsurg.137.6.653
6. Demirjian A, Peng P, Geschwind JF, et al. Infiltrating hepatocellular carcinoma: seeing the tree through the forest. J Gastrointest Surg. 2011;15(11):2089–2097 doi:10.1007/s11605-011-1614-7
7. Sereni CP, Rodgers SK, Kirby CL, Goykhman I. Portal vein thrombus and infiltrative HCC: a pictoral review. Abdom Radiol. 2017;42(1):159–170 doi:10.1007/s00261-016-0855-z
8. Kneuertz PJ, Demirjian A, Firoozmand A, et al. Diffuse infiltrative hepatocellular carcinoma: assessment of presentation, treatment, and outcomes. Ann Surg Oncol. 2012;19(9):2897–2907 doi:10.1245/s10434-012-2336-0
9. Yopp AC, Mokdad A, Zhu H, et al. Infiltrative hepatocellular carcinoma: natural history and comparison with multifocal, nodular hepatocellular carcinoma. Ann Surg Oncol. 2015;22 Suppl 3:S1075–1082 doi:10.1245/s10434-015-4786-7
10. Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi:10.1056/NEJMoa0708857
11. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised Phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–1173. doi:10.1016/S0140-6736(18)30207-1
12. Cheng AL, Qin S, Ikeda M, et al. Updated efficacy and safety data from IMbrave150: atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J Hepatol. 2022;76(4):862–873. doi:10.1016/j.jhep.2021.11.030
13. Shao YY, Feng YH, Yen CJ, et al. Bevacizumab and atezolizumab as first-line therapy for advanced hepatocellular carcinoma: a Taiwanese subgroup analysis on efficacy and safety. J Formos Med Assoc. 2022;121(12):2430–2437. doi:10.1016/j.jfma.2022.09.005
14. Chen CT, Feng YH, Yen CJ, et al. Prognosis and treatment pattern of advanced hepatocellular carcinoma after failure of first-line atezolizumab and bevacizumab treatment. Hepatol Int. 2022;16(5):1199–1207. doi:10.1007/s12072-022-10392-x
15. Abou-Alfa GK, Lau G, Kudo M, et al. Tremelimumab plus durvalumab in unresectable hepatocellular carcinoma. NEJM Evid. 2022;1(8):EVIDoa2100070. doi:10.1056/EVIDoa2100070
16. Cheng AL, Kang YK, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a Phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34. doi:10.1016/S1470-2045(08)70285-7
17. Shao YY, Wang SY, Lin SM. Management consensus guideline for hepatocellular carcinoma: 2020 update on surveillance, diagnosis, and systemic treatment by the Taiwan liver cancer association and the gastroenterological society of Taiwan. J Formos Med Assoc. 2021;120(4):1051–1060. doi:10.1016/j.jfma.2020.10.031
18. Chen CT, Hsu CH, Cheng AL, Shao YY. Expanding sorafenib treatment for hepatocellular carcinoma beyond Barcelona clinic liver cancer stage C patients: a national study. Anticancer Res. 2022;42(9):4461–4470. doi:10.21873/anticanres.15946
19. Koulakian H, Allaham W, Vilgrain V, Ronot M. Non-measurable infiltrative HCC: is post-contrast attenuation on CT a sign of tumor response? Eur Radiol. 2019;29(8):4389–4399. doi:10.1007/s00330-018-5805-4
20. Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–380. doi:10.1002/hep.29086
21. Velcheti V, Schalper K. Basic overview of current immunotherapy approaches in cancer. Am Soc Clin Oncol Educ Book. 2016;35(36):298–308. doi:10.1200/EDBK_156572
22. Harding JJ, Nandakumar S, Armenia J, et al. Prospective genotyping of hepatocellular carcinoma: clinical implications of next-generation sequencing for matching patients to targeted and immune therapies. Clin Cancer Res. 2019;25(7):2116–2126. doi:10.1158/1078-0432.CCR-18-2293
23. Dong LQ, Peng LH, Ma LJ, et al. Heterogeneous immunogenomic features and distinct escape mechanisms in multifocal hepatocellular carcinoma. J Hepatol. 2020;72(5):896–908. doi:10.1016/j.jhep.2019.12.014
24. Hazini A, Fisher K, Seymour L. Deregulation of HLA-I in cancer and its central importance for immunotherapy. J Immunother Cancer. 2021;9(8):e002899. doi:10.1136/jitc-2021-002899
25. Kudo M. Limited impact of Anti-PD-1/PD-L1 monotherapy for hepatocellular carcinoma. Liver Cancer. 2020;9(6):629–639. doi:10.1159/000512170
26. Qin S, Chan SL, Gu S, et al. Camrelizumab plus rivoceranib versus sorafenib as first-line therapy for unresectable hepatocellular carcinoma (CARES-310): a randomised, open-label, international phase 3 study. Lancet. 2023;402(10408):1133–1146. doi:10.1016/S0140-6736(23)00961-3
27. Donne R, Lujambio A. The liver cancer immune microenvironment: therapeutic implications for hepatocellular carcinoma. Hepatology. 2023;77(5):1773–1796. doi:10.1002/hep.32740
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Simultaneous and Sequential Use of Molecular Targeted Agents Plus Immune Checkpoint Inhibitors for Advanced Hepatocellular Carcinoma: A Real-World Practice in China
Li J, Huang L, Ge C, Zhu X, Qiu M, Chen C, Wei S, Yan Y
Journal of Hepatocellular Carcinoma 2023, 10:949-958
Published Date: 20 June 2023
Immunotherapy Efficacy in Advanced Hepatocellular Carcinoma in a Diverse and Underserved Population in the United States
Bteich F, Desai K, Zhang C, Kaur A, Levy RA, Bioh L, Wang A, Sultana S, Kaubisch A, Kinkhabwala M, Bellemare S, Fidvi S, Kanmaniraja D, Berkenblit R, Moon JY, Adedimeji A, Tow CY, Saenger Y
Journal of Hepatocellular Carcinoma 2024, 11:257-269
Published Date: 3 February 2024
Systemic Drugs for Hepatocellular Carcinoma: What Do Recent Clinical Trials Reveal About Sequencing and the Emerging Complexities of Clinical Decisions?
Himmelsbach V, Koch C, Trojan J, Finkelmeier F
Journal of Hepatocellular Carcinoma 2024, 11:363-372
Published Date: 19 February 2024
Prediction of Pathologic Response in Unresectable Hepatocellular Carcinoma After Downstaging with Locoregional and Systemic Combination Therapy

Yang C, Chen Y, Sheng L, Wang Y, Zhang X, Yang Y, Ronot M, Jiang H, Song B
Journal of Hepatocellular Carcinoma 2025, 12:43-58
Published Date: 16 January 2025




