Back to Journals » Advances in Medical Education and Practice » Volume 16
Understanding Barriers and Motivations: Enhancing Support for UK Medical Students’ Participation in Foreign Medical Electives
Authors Sarela S, Asim N, Atapaka S, Sheriff V, Barzyk-Sheriff GA
Received 4 November 2024
Accepted for publication 27 March 2025
Published 19 April 2025 Volume 2025:16 Pages 637—649
DOI https://doi.org/10.2147/AMEP.S499581
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Shazia Sarela,1 Naireen Asim,2,* Shruthi Atapaka,2,* Vafie Sheriff,3 Gabriela Anna Barzyk-Sheriff3
1UCL Medical School, University College London, London, UK; 2St George’s University of London Medical School, St George’s University of London, London, UK; 3Royal Wolverhampton NHS Trust, Wolverhampton, UK
*These authors contributed equally to this work
Correspondence: Shazia Sarela, University College London, Gower Street, London, WC13 6BT, United Kingdom, Email [email protected]
Purpose: This study aimed to explore UK medical students’ preferences, motivations, and barriers regarding international electives and to evaluate the impact of an online planning event designed to address these. Additionally, this study examined trends in UK medical students completing foreign electives over the past decade.
Methods: Freedom of Information requests were sent to 46 UK medical universities requesting data on the number of students undertaking foreign electives over the past 10 years. Attendees at a peer-led event regarding electives completed a survey on their motivations and challenges in doing a foreign elective, followed by a post-event feedback form. Results were analysed using the Python Scipy package.
Results: Of the 103 respondents, 76.7% preferred to undertake an international elective, while 21.36% preferred a combination of the UK and international locations. Non-academic reasons were significant motivators for undertaking a foreign elective, while safety and financial concerns were major deterrents. The online event received positive feedback, with participants appreciating the utility of the event in aiding their understanding of the elective planning process.
Conclusion: UK medical students show a strong preference for international electives, despite significant barriers, particularly related to safety and finances. The peer-led event proved to be effective in supporting students’ planning of electives.
Keywords: undergraduate medical education, medical student elective, COVID-19 pandemic, cultural competencies, international medical education
Introduction
Medical electives are short-term placements that medical students undertake, typically in their final years of study, to gain hands-on experience in a clinical setting of their interest, either locally or internationally. The key motivations behind medical students’ participation in international electives are cultural immersion, exposure to diverse healthcare practices, opportunities for personal and professional growth.1 Multiple studies conclude such experiences also foster an increased interest in academic medicine and enhance cultural competence.2–5 Additionally, foreign electives offer opportunities for enhancement of problem solving and critical and innovative thinking, as students may be exposed to limited resource settings where they must still provide effective patient care.5 However, existing studies are limited by their poorly specified scope of participating medical schools, dearth of comparative data between medical schools, and narrow participation criteria.5 Also, factors such as destination choice and support structures remain underexplored.3
UK medical students face several obstacles in participating in international medical electives. Safety concerns, politically unstable regions, or areas with inadequate healthcare infrastructure, frequently discourage participation,6 and the high costs of international travel and living can be prohibitively expensive.7 Visa requirements and language barriers further limit equitable access and available experiences, as do integration into foreign clinical environments.6,7 Furthermore, the ethical considerations and dilemmas associated with international electives significantly influence students’ choice of destination,7 especially when there is limited availability of support structures necessary for effective participation.
The COVID-19 pandemic has significantly affected medical students’ perceptions of their careers and their engagement in electives.8 The pandemic is likely to have influenced their destination choices as they navigate career planning amid uncertainty. However, the influence of the pandemic on international electives, including barriers to participation and the level of support provided by medical schools has not been directly evaluated.8 Whilst the pandemic’s effects on medical education have been studied, these efforts have focussed on shifts in clinical practice, telehealth adoption, and disruptions in clinical rotations.9 Research on medical students’ involvement in clinical research during the pandemic has highlighted various challenges10 but motivations, expectations and challenges in relation to international electives as well as destination choices of foreign electives have not been investigated.
Considering the multitude of challenges that are faced by students, medical schools could play a vital role in supporting international elective participation. Comprehensive support, including financial aid and mentorship, can boost students’ confidence and experience during international electives.11 The UK Medical Schools Council recommends enhancing support through early exposure, safety protocols, and psychological assistance across all elective phases.12,13 Despite this, levels of support that are received by medical students in planning international electives have not been studied.
There are substantial advantages in pursuing electives. However, a significant gap in the literature persists regarding the perceptions, motivations, and obstacles faced by UK medical students, and the support that is available to them, when considering foreign electives. This study aims to examine the experiences of UK medical students with planning and considering international electives. The objectives of our study are to a) understand trends and accessibility of a foreign elective for medical students in the UK by assessing the number of students who have undertaken a foreign elective in the past 10 years; b) explore the motivations and expectations of UK medical students considering a foreign elective; c) identify any barriers or concerns that may discourage UK medical students from pursuing international electives; d) understand current students’ knowledge and understanding of planning foreign electives; and e) understand the level of support students perceive they have received from their institutions.
Addressing the identified barriers and enhancing support structures will empower students to fully engage in and benefit from international electives, ultimately shaping well-rounded healthcare professionals ready for the complexities of global health.
Methods
A Freedom of Information (FOI) Request was sent to all 46 British Medical Schools requesting the percentage of students completing an elective in any part for any duration outside of the UK in each cohort 2013–2023 to understand trends in foreign electives and assess the pandemic’s impact on accessibility. Additionally, institutions were requested to provide the reason why they were unable to provide the requested data in any part.
A survey to collect data related to medical student preferences, understanding, motivating and deterring factors surrounding international electives was designed using the AMEE guide for educational research, including pilot testing on 10 individuals and feedback from medical educators.
The survey consisted of 26 close-ended questions, including demographics; preference of elective location and the impact of the Covid pandemic on elective choices. Factors related to students’ knowledge, understanding, motivations and barriers to foreign electives were assessed using a 5-point Likert Scale, with 1 being the least and 5 the most (Table 1). Students were given the option to provide additional details for the reasons the Covid pandemic impacted their choice of elective destination. Students’ eligibility for Widening Participation Programmes (WPP) and students’ number of years before undertaking their elective were collected as control variables.
 |
Table 1 Aspects Regarding Undertaking a Foreign Elective Students Were Asked to Rate Using a Likert Scale |
Survey participants were recruited using convenience sampling through an online event titled “How to plan your elective”, targeting UK medical students. This sampling technique was selected due to the ease of participant recruitment and to avoid recruiter bias. This event consisted of current medical students and doctors talking about their experiences while undertaking an international elective and providing advice on how to plan and benefit from an international elective. The survey was administered to attendees prior to the event. A separate feedback form, composed of 3 Likert scale-based questions and one open-ended question, was administered after the event (Table 2). By nature of the survey, only current medical students in the UK could complete the survey and feedback form. This study received exemption from ethics approval by UCL as it collected completely anonymous, non-sensitive data from students using an educational survey. All students attending the event were provided with a Participation Information Leaflet, which detailed how their data would be used for research and their right to withdraw from the study at any time. All students who completed the survey and feedback form consented to their anonymous data being used for research purposes.
 |
Table 2 Aspects Regarding the “How to Plan Your Elective” Event Students Were Asked to Rate Using a Likert Scale |
Statistical analysis was conducted using Python’s ScipyStats package and included a chi-squared test to demonstrate association between categorical variables; a Wilcoxon Signed Rank Test or The Friedman Test to compare paired data; a Mann Whitney U-test for unpaired data; and a Spearman Rank Test to demonstrate correlation.
Results
Figure 1 demonstrates the average Percentage of Students Undertaking a Foreign Elective (PSUFE) from 2013 to 2023 from the FOI data. Tables 3, 4 and Table S1 outline the number of universities able to provide data for each year and includes yearly statistics including the mean, maximum, minimum, inter-university variance and percentage changes from pre-pandemic levels. This achieved our aim to understand trends and accessibility of a foreign elective for medical students in the UK by assessing the number of students who have undertaken a foreign elective in the past 10 years.
 |
Table 4 Values Related to the Average Percentage of Students Undertaking a Foreign Elective in 33 British Universities from 2013 to 2023 |
 |
Figure 1 Box plot representing mean percentage of students undertaking a foreign elective in part or full across British universities in the period 2013–2023. |
One hundred and three out of the 149 (69%) attendees at the online event completed the questionnaire and consented for their data to be used for research. The demographic data from the questionnaire is outlined in Table 5, with responses from students of 10 different British universities. Over 90% of all respondents were scheduled to undertake their elective in the next 2 years, with 70% in just over 1 year. 76.7% of students preferred an entirely international elective, followed by 21.36% in the UK and Abroad, and 1.94% in the UK only. The respondents’ preferences for elective location by country is outlined in Figure 2.
 |
Table 5 Demographics of Students Responding to Pre-Event Questionnaire |
 |
Figure 2 Bar chart representing students’ self-reported preference for elective destinations. |
Students identifying themselves as eligible for Widening Participation Programmes (WPP) were found to be 3-fold more likely to prefer a UK-based elective than those who were ineligible (Chi-squared test p-value = 0.002).
Table 6a and b outlines the students’ responses for five-point Likert scale questions assessing their understanding and knowledge; motivating aspects and deterring factors related to foreign electives and are further detailed below.
Students’ rating for their levels of understanding and knowledge of the requirements from their university regarding their electives received the highest mean score (2.29/5) out of the 4 aspects measured. There was no significant difference found amongst the rating of understanding for the 3 lowest scoring aspects (travel planning; logistics; and financial support) (Friedman Test p value = 0.959). This achieved our aim to understand current students’ knowledge and understanding of planning foreign electives.
Student scores for the importance of non-academic reasons (4.13/5) were significantly greater than the scores for the importance of academic factors (3.86/5) (Wilcoxon signed-rank test p value = 0.026). This achieved our aim to explore the motivations and expectations of UK medical students considering a foreign elective.
There were no significant differences amongst student scores for the importance of financial (3.95/5) and safety-related aspects while undertaking a foreign elective (3.99/5) (Wilcoxon signed-rank test p value = 0.656). The overall score across all deterring factors was significantly higher amongst students preferring UK-based electives (5/5) than a foreign elective (3.93/5) (Mann Whitney U-test p value = 0.046). Additionally, the rating of the importance of financial barriers was significantly higher amongst students eligible for WPP (4.47/5) than those who were not (3.79/5) (Mann Whitney U-Test p-value = 0.009). A significant negative correlation was found between student levels of understanding and knowledge of planning electives and the level of importance given to deterring factors (Spearman Rank Test p-value = 0.009) (Figure 3). This achieved our aim to identify any barriers or concerns that may discourage UK medical students from pursuing international electives, 78.65% of students reported no impact of the pandemic on their elective choices. 16.5% were more likely to choose a foreign elective, citing reasons such as missed travel opportunities and wanting to explore alternative medical settings after the pandemic. 4.85% were more likely to remain in the UK due to concerns about illness or a desire to contribute to the NHS.
 |
Figure 3 Regression plot demonstrating correlation between rating for understanding and knowledge related to foreign electives and importance of deterring factors. |
Table 7 shows the self-perceived level of support students received from their university regarding electives using a five-point Likert scale, with a mean score of 1.94/5. There was no significant difference in the scores of students greater or less than 2 years away from undertaking their elective (Mann Whitney U-test p-value = 0.79). Students preferring foreign electives rated university support significantly higher (1.95/5) than those preferring UK-based electives (1.5/5) (Mann Whitney U-test p-value = 0.056). A significant positive correlation was found between the student levels of understanding and knowledge of planning electives and the level of support received from their university (Spearman Rank Test p-value = 0.0001) (Figure 4). This achieved our aim to understand the level of support students perceive they have received from their institutions.
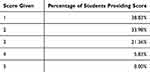 |
Table 7 Percentage of Students Rating Each Score for Their Perceived Level of Support Received from Their University Regarding Their Elective Using a Likert Scale |
 |
Figure 4 Regression plot demonstrating correlation between student understanding and knowledge related to foreign electives and level of support received from their universities. |
The post event feedback survey was answered by 70/149 students (46.9%), with the results shown in Table 8 and Figure 5. The reduction in response rate from the pre-event questionnaire was primarily due to non-response bias as participants had already filled out the initial survey and benefited from attending the event, as well as logistical challenges, including scheduling conflicts, time constraints, and participants’ inability to attend the full event. Students described hearing from students with foreign elective experience and learning about the logistics of foreign electives as the most valuable aspects of the event in the open-ended question asked in the feedback form.
 |
Table 8 Percentage of Students Rating Each Score for Different Aspects of the “How to Plan Your Elective” Event Feedback Form Using a Likert Scale |
 |
Figure 5 Box plot demonstrating mean score out of 5 for questions asked to students after the “How to Plan Your Elective” event. |
Discussion
The FOI request data reveal significant trends in UK medical students’ participation in international electives. The pre-pandemic proportion of students undertaking foreign electives was 75.1% from 2013 to 2019, with minimal annual variation. This consistency suggests a sustained interest in international experiences, aligning with previous studies that highlight the importance of global health exposure in medical education.14 The considerable variation between universities (see Table S1) could be attributed to differing institutional support, financial resources, and the availability of established partnerships with foreign institutions.
The pandemic resulted in a 63.1% decrease in foreign elective participation in 2019–2020, consistent with previous studies that reported a substantial decline in medical student mobility during the pandemic due to travel restrictions and safety concerns.15 The lowest participation rate of 1.6% was recorded in 2020/2021. In contrast, 53.9% of students completed a foreign elective in 2022/2023. Yet, this was significantly lower than the pre-pandemic average, despite the easing of travel restrictions. The slow recovery in foreign elective participation may be due to increased reliance on virtual learning and telemedicine, post-pandemic.16 Nonetheless, the numerous and clear benefits of international electives provide a compelling argument for efforts to ensure that hesitancy to travel owing to lack of confidence or experience does not lead to students opting out of foreign electives.
Previous studies corroborate our findings that UK medical students are primarily motivated to undertake foreign electives by opportunities for personal growth, cultural immersion, and professional development.17 The highest scores of importance given to non-academic reasons emphasise the value students place on the holistic experience of living and working in a different cultural setting.
The high scores given to financial and safety-related factors by students as aspects deterring them from completing a foreign elective emphasises the importance of financial support being made available to students. Also, concerns regarding safety require to be discussed and mitigated to facilitate more students to complete a foreign elective. The significantly higher average score to deterrent factors by students preferring UK-based electives highlights the importance that safety, finance, logistics and personal aspects play in discouraging students from undertaking foreign electives. Targeted talks, materials and mentorship can serve to quell unrequited worries.
Students eligible for WPP are typically from lower socio-economic backgrounds, giving rise to concerns regarding the specific barriers for these students. Students eligible for WPP were found to be 3-fold more likely to complete a UK-based foreign elective. This can be largely attributed to financial constraints as the average score given to the importance of financial barriers was significantly higher amongst WPP eligible students than others. WPP students often lack the resources to cover the costs of travel, accommodation, and living expenses abroad.18 Additionally, the complexity of organising international placements and scarcity of institutional support19 could further deter these students from pursuing international electives. Unequal access to international electives could exacerbate existing disparities in medical education, through missing out opportunities for holistic growth. However, despite the recognised benefits, there is insufficient support available specifically for financially constrained students.20 Potential solutions include the provision of targeted financial aid for international electives, comprehensive guidance and planning resources, and establishment of partnerships with international institutions to create more affordable opportunities.
A significant majority (76.7%) of respondents expressed a preference for completing their elective abroad, with East Asia (20%) and Oceania (18%) emerging as the most popular destinations. East Asia’s rapidly advancing healthcare infrastructure and technology may be attractive to students as an opportunity to gain exposure to cutting-edge medical practices and innovations.21 Furthermore, the cultural immersion and vastly different healthcare system can provide valuable learning experiences, particularly in areas like infectious diseases and public health.22 Oceania appeals to students interested in environmental health and indigenous health care, as well as those seeking experience in rural and remote medicine.23 Students who completed electives in Oceania reported significant gains in their understanding of global health issues and a greater appreciation for the social determinants of health.24,25
The Middle East remains the least popular destination, chosen by only 4% of students. Concerns regarding safety may be the underlying cause. In our study, safety has emerged as the most important factor deterring students from undertaking a foreign elective, receiving an average score of 3.99/5, and being scored 5/5 for importance by 38.8% of respondents. Perceptions of political instability, regional conflicts, and cultural differences, alongside limited awareness of healthcare systems and institutional partnerships may contribute to the low appeal of the Middle East.26 Addressing these concerns through improved communication, safety assurances, and fostering collaborations could enhance its attractiveness as an elective destination.
The feedback from our elective planning event highlights the value students place on practical knowledge and peer support, with most respondents reporting excellent confidence in planning their elective and a good understanding of the logistical and cultural aspects involved post the event. The present feedback is consistent with previously reported evidence that structured preparation (including cultural competency training, language courses, and logistical planning) significantly enhances the educational outcomes of international electives.27 Students who receive comprehensive pre-departure training are more likely to have positive experiences and report higher levels of satisfaction with their electives. Additionally, such training mitigates the risks of cultural misunderstandings and logistical challenges, allowing adequate focus on clinical and professional development. In this context, access to experienced mentors helps students to navigate foreign healthcare systems and to enhance the learning experience. Furthermore, mentorship contributes to students’ personal growth by providing them with role models who embody professionalism and ethical practice in diverse cultural settings.27
The average rating for institutional support by students was 1.95/5, with over 70% of students rating the support as 1 or 2 out of 5. This indicates a concerning lack of resources, support and guidance provided to students in planning international electives. Also, students’ knowledge and understanding of factors related to planning their electives such as support available, university mandated requirements and travel essentials, was low across all domains. We found a significant positive correlation between the scores for available support and levels of student understanding and knowledge. This finding strongly indicates that improving support, resources and mentorship at the university level can enhance students’ confidence in planning foreign electives. Furthermore, the significantly negative correlation between students’ understanding and knowledge of elective related factors and their scoring of the importance of deterring factors suggests that many of the issues students regard as adverse could be mitigated by greater support from their medical schools.
In making decisions about allocating resources to supporting international electives, medical schools should consider that the integration of global health curricula and cultural competency training into medical education is crucial for preparing students for the challenges and opportunities of medical practice. Students who receive such training are better equipped to adapt to different cultural contexts and are more likely to have successful and meaningful elective experiences.28,29 Medical schools should prioritise these elements in their educational policies to ensure that all students, regardless of background, can access and benefit from international electives.
We accept that the present study is limited by the small sample size of 103 respondents, and FOI data only up to 2023, which limited our ability to assess post-COVID-19 trends. The event for recruiting participants was primarily aimed at helping students to plan foreign electives, which may have attracted a participant pool that was biased to foreign electives, leading to overestimation of the importance of motivating factors. We opted to primarily use close-ended questions and limited the number of controlling variables collected, such as WPP eligibility and the timeframe until students would undertake their elective, to maximise survey participation and minimise respondent burden. However, this approach restricted the opportunity for deeper exploration of other perceived barriers or motivations related to undertaking a foreign elective, such as ethical considerations or more specific, individualised concerns. Collecting additional data—such as individual students’ financial status, visa requirements, and specific connections to countries or hospitals—could provide a more comprehensive understanding of the factors that motivate or hinder participation in foreign electives.
We are now contemplating further research, using data beyond 2023, to assess the long-term impacts of the pandemic on medical student mobility. A mixed-methods approach with surveys and interviews may provide deeper insights into students’ experiences. Additional research on the effectiveness of specific support methods about planning foreign electives and the long-term career impacts of international electives, especially for WPP students, would be valuable. Our understanding of the value and long-term benefits of international electives may also be advanced by retrospective survey of the experiences of qualified doctors with specialist interests, including research and extra-clinical activities. Such studies may incentivise medical schools to strengthen support structures and provide direction on successful support structures.
Conclusion
Our study highlights the motivations, preferences, and challenges of UK medical students pursuing international electives and was able to fulfil all its objectives initially stated. To promote global engagement and equip students with essential skills, medical schools should align elective planning with students’ goals for clinical and personal growth while directly engaging them in the process to ensure diverse clinical exposure and personal development. Addressing declining participation and support gaps worsened by COVID-19 is critical, as is applying innovative models to overcome financial, logistical, and institutional barriers that hinder access to international electives. By leveraging data to create inclusive policies, medical schools can expand participation in foreign electives in the post-pandemic context. Additionally, strengthening institutional support—through financial aid, logistical guidance, and mentorship—will ensure equitable access, particularly for underrepresented students. These efforts will not only enhance the impact of international electives but also foster a more inclusive and globally competent generation of medical professionals.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Holmes D, Zayas LE, Koyfman A. Student objectives and learning experiences in a global health elective. J Community Health. 2012;37(5):927–934. doi:10.1007/s10900-012-9547-y
2. Arps S, Noviski KM, Tucker L, Tutwiler A. Medical students’ motivations for participating in an elective focused on social inequalities and health disparities. Adv Health Sci Educ. 2024;29(1):1–26. doi:10.1007/s10459-024-10320-8
3. Hayashi M, Son D, Nanishi K, Eto M. Long-term contribution of international electives for medical students to professional identity formation: a qualitative study. BMJ Open. 2020;10(8):e039944. doi:10.1136/bmjopen-2020-039944
4. Harmer A, Lee K, Petty N. Global health education in the United Kingdom: a review of university undergraduate and postgraduate programmes and courses. Public Health. 2015;129(6):797–809. doi:10.1016/j.puhe.2014.12.015
5. Arja SB, Arja SB, Ponnusamy K, Kottath Veetil P, Paramban S, Laungani YC. Medical education electives can promote teaching and research interests among medical students. Adv Med Educ Pract. 2024;Volume 15:173–180. doi:10.2147/AMEP.S453964
6. Liljedahl M, Björck E, Ponzer S, Bolander Laksov K. Navigating without a map: how medical students interact with clinical learning environments. Stud Higher Educ. 2019;44(2):275–286. doi:10.1080/03075079.2017.1359822
7. Rahim A, Knights F, Fyfe M, Alagarajah J, Baraitser P. Preparing students for the ethical challenges on international health electives: a systematic review of the literature on educational interventions. Med Teach. 2016;38(9):911–920. doi:10.3109/0142159X.2015.1132832
8. Byrnes YM, Civantos AM, Go BC, McWilliams TL, Rajasekaran K. Effect of the COVID-19 pandemic on medical student career perceptions: a national survey study. Med Educ Online. 2020;25(1):1798088. doi:10.1080/10872981.2020.1798088
9. Storz MA. International medical electives during and after the COVID-19 pandemic-current state and future scenarios: a narrative review. Globalization Health. 2022;18(1):44. doi:10.1186/s12992-022-00838-0
10. Hall L, Binks S, Heal C. The effect of COVID-19 on medical student clinical skill practice and self-perceived proficiency. MedEdPublish. 2023;13:10. doi:10.12688/mep.19478.2
11. McKinnon T, Watson A, Richards L, Sears J, Brookes MJ, Green CA. The volunteers in research programme: supporting COVID-19 research and improving medical training in parallel. Clin Med. 2021;21(3):182. doi:10.7861/clinmed.2020-1072
12. Cherniak WA, Drain PK, Brewer TF. Educational objectives for international medical electives: a literature review. Acad Med. 2013;88(11):1778–1781. doi:10.1097/ACM.0b013e3182a6a7ce
13. Wiskin C, Barrett M, Fruhstorfer B, Schmid ML. compiled on behalf of the MSC UK Electives Committee. Recommendations for undergraduate medical electives: a UK consensus statement. Medical Education. 2018;52(1):14–23. doi:10.1111/medu.13445
14. Collaborative IU. Global health education in medical schools (GHEMS): a national, collaborative study of medical curricula. BMC Med Educ. 2020;20:389.
15. Yıldırım S, Bostancı SH, Yıldırım DÇ, Erdoğan F. Rethinking mobility of international university students during COVID-19 pandemic. Higher Educ Evaluation Develop. 2021;15(2):98–113. doi:10.1108/HEED-01-2021-0014
16. Walters M, Alonge T, Zeller M. Impact of COVID-19 on medical education: perspectives from students. Acad Med. 2022;97(3S):S40–8. doi:10.1097/ACM.0000000000004525
17. Watson DA, Cooling N, Woolley IJ. Healthy, safe and effective international medical student electives: a systematic review and recommendations for program coordinators. Tropical Dis Travel Med Vaccines. 2019;5(1):1–4. doi:10.1186/s40794-019-0081-0
18. Sartania N, Alldridge L, Ray C. Barriers to access, transition and progression of Widening Participation students in UK Medical Schools: the students’ perspective. MedEdPublish. 2021;10(1). doi:10.15694/mep.2021.000132.1
19. Harrison N, Davies S, Harris R, Waller R. Access, participation and capabilities: theorising the contribution of university bursaries to students’ well-being, flourishing and success. Cambridge J Educat. 2018;48(6):677–695.
20. Krstić C, Krstić L, Tulloch A, Agius S, Warren A, Doody GA. The experience of widening participation students in undergraduate medical education in the UK: a qualitative systematic review. Med Teach. 2021;43(9):1044–1053. doi:10.1080/0142159X.2021.1908976
21. Hasebe K, Tamai A, Yamada S, Maskarinec GG. Trends of international electives in medical education undergraduates in Japan. Hawaii J Health Soc Welfare. 2022;81(10):279.
22. Peluso MJ, Rodman A, Mata DA, Kellett AT, van Schalkwyk S, Rohrbaugh RM. A comparison of the expectations and experiences of medical students from high-, middle-, and low-income countries participating in global health clinical electives. Teaching Learning Med. 2018;30(1):45–56. doi:10.1080/10401334.2017.1347510
23. Liu Y, Zhang Y, Liu Z, Wang J. Gaps in studies of global health education: an empirical literature review. Global Health Action. 2015;8(1):25709. doi:10.3402/gha.v8.25709
24. James Imperato P. A third world international health elective for US medical students: the 25-year experience of the state university of New York, Downstate Medical Center. J Community Health. 2004;29(5):337–373. doi:10.1023/B:JOHE.0000038652.65641.0d
25. Withers M, Press D, Wipfli H, et al. Training the next generation of global health experts: experiences and recommendations from pacific rim universities. Globalization Health. 2016;12(1):1–7. doi:10.1186/s12992-016-0162-z
26. St Clair NE, Pitt MB, Bakeera-Kitaka S, et al. Global health: preparation for working in resource-limited settings. Pediatrics. 2017;140(5):e20163783. doi:10.1542/peds.2016-3783
27. Smith JK, Weaver DB. Capturing medical students’ idealism. Anna Family Med. 2006;4(suppl 1):S32–7. doi:10.1370/afm.543
28. Battat R, Seidman G, Chadi N, et al. Global health competencies and approaches in medical education: a literature review. BMC Med Educ. 2010;10(1):1–7. doi:10.1186/1472-6920-10-94
29. Mews C, Schuster S, Vajda C, et al. Cultural competence and global health: perspectives for medical education–Position paper of the GMA committee on cultural competence and global health. GMS J Med Educ. 2018;35(3). doi:10.3205/zma001174
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



