Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 20
Withholding of Life-Sustaining Treatment and Mortality in ICU Patients with Severe Acute COPD Exacerbations: A Retrospective French Cohort
Authors Puechoultres P, Jamme M, Abi-Abdallah G, Diop S, Legriel S, Ferré A
Received 27 December 2024
Accepted for publication 20 May 2025
Published 18 June 2025 Volume 2025:20 Pages 1995—2009
DOI https://doi.org/10.2147/COPD.S502019
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Pauline Puechoultres,1 Matthieu Jamme,2,3 Georges Abi-Abdallah,4 Sylvain Diop,5 Stéphane Legriel,1,6 Alexis Ferré1
1Intensive Care Unit, Versailles Hospital, Le Chesnay, France; 2Intensive Care Unit, West Parisian Private Hospital, Ramsay-Générale de Santé, Trappes, France; 3Department for Research, Studies, Assessment and Statistics (DREES), French Ministry of Health, Paris, France; 4Department of Anesthesiology and Critical Care, APHP, Hôpital Européen Georges Pompidou, Paris, France; Université de Paris, INSERM, IThEM, Paris, France; 5Department of Anesthesiology and Intensive care, Marie Lannelongue Hospital, Le Plessis Robinson, France; 6University Paris-Saclay, UVSQ, INSERM, CESP, Villejuif, France
Correspondence: Alexis Ferré, Intensive Care Unit, Versailles Hospital, 177 Rue de Versailles, Le Chesnay, 78150, France, Email [email protected]
Background: Data on withholding life-support (WLS) decisions during acute exacerbations of chronic obstructive pulmonary disease (COPD) in the intensive care unit (ICU) are scarce. This study aimed to identify factors associated with these decisions and their impact on mortality.
Methods: We conducted a monocentric retrospective cohort study on all patients admitted to our ICU between 2015 and 2021 for a severe acute exacerbation of COPD. Logistic multivariable regression analysis was performed.
Results: We included 463 patients of whom 128 (27.6%) had a decision of withholding of care. The 3-months mortality was 49.2% and 4.8% in the WLS group and in the no WLS group, respectively. Forty-eight patients (10.4%) had advanced healthcare directives. In multivariable analysis, factors associated with a decision of WLS were higher age (odds ratio [+10 years] = 1.93, p < 0.001), immunodeficiency (OR = 3.07, p < 0.001), higher Performance Status (PS) score (OR [+1 point] = 2.10, p < 0.001), long-term oxygen therapy (OR = 4.11, p < 0.001) and shock after ICU admission (OR = 2.43, p = 0.01). In multivariate analysis, factors significantly associated with 3-month mortality included decision of WLS during ICU (OR = 22.98, p < 0.001) and invasive mechanical ventilation (OR = 2.72, p < 0.001).
Conclusion: Approximately 30% of COPD patients underwent a decision to withhold life-sustaining treatment. Higher age, immunosuppression, increased PS score, and long-term oxygen therapy were significantly associated with this decision. Nearly half of the patients died within three months following a withholding of care decision.
Keywords: COPD, exacerbation, mortality, withholding, life-support
Background
Chronic obstructive pulmonary disease (COPD) exacerbation presents as a transient increase in respiratory symptoms,1 with acute severe exacerbations requiring intensive care unit (ICU) ventilatory assistance in 2% to 4% of the cases.2 Exacerbations play a crucial role in the disease impairment by increasing bronchial inflammation and accelerating the decline of the lung function.1 Despite advances in ICU management over the past decades, mortality rates following exacerbations remain high,3 ranging from 15% in the ICU to 30% at day 904 and 30% at 1 year.5 Many ICU deaths occur after a decision to withhold or withdraw life-sustaining therapies, with previous studies reporting that 90% of COPD patients who died in the ICU had a prior “do not intubate” decision.6,7 Identifying COPD patients for whom ICU care may be of limited benefit and establishing an early care plan remains a major challenge. There is general agreement that specific palliative care should be integrated early in the healthcare pathway for patients with the most severe stages of COPD. However, no standardized recommendations exist regarding the individualized intensity of care during an ICU stay.8 Nevertheless and in comparison with cancer patients, COPD patients are more likely to die in ICU, without having had access to palliative care before ICU admission.9,10 Recent literature provides very limited information on the decisions of withholding of life-sustaining treatment, their characteristics, and the consequences on COPD patients outcomes. Integrating decisions of withhold and withdrawal life-sustaining treatment play a major role in the care process of COPD patients admitted to ICU for a severe acute exacerbation. The decision-making process is further complicated due to the lack of identified prognostic factors,11 the difficulty for patients in critical condition to express their will,12 and the difficulty for physicians to address these topics.13 Indeed, fewer than 50% of COPD patients had been informed by their primary physician about the possibility of intubation during a life-threatening exacerbation.12,13
Unlike non-invasive ventilation (NIV), invasive mechanical ventilation (MV) is associated with high morbidity and mortality.14 Therefore, the ethical question of its use is crucial. The advance care planning process facilitates the writing of advanced healthcare directives and seems to reduce the gap between the patient’s will and the subsequent delivery of care.15 There is substantial variability and no formal recommendations in the withhold or withdrawal life-sustaining treatment process between world regions, countries and individual ICUs within a country.16,17 In France, the concept grows from preventing the unreasonable obstinacy. Described in the Claeys-Leonetti law in 2016, it lies in the principle of withholding or not engaging in medical therapies that [appears to be useless, disproportionate or having no other effect than the sole artificial maintenance of life].18 An observational European study conducted in 67 ICUs in 2020 reported that in most of cases, multidisciplinary meeting following consensus among all participating physicians was preferred.19 The medical literature on this topic for COPD patients admitted to the ICU is limited and does not provide physicians with a clear understanding of the factors influencing withholding life-support (WLS) decisions or their impact on patients’ mid-term prognosis.
The main objectives of this study were to identify the factors associated with decisions of withholding of life-sustaining therapies, to describe the different types of organ support withholding decisions during ICU, and to evaluate the association with outcome for patients admitted to the ICU for severe acute exacerbation of COPD.
Study Design and Methods
This is an observational, retrospective, and monocentric study. The ethics committee of the French Intensive Care Society (N°#21-66, 2021) approved the study and the protocol was registered at the French National Institute for Health Data (#MR2516271119). All procedures were carried out in accordance with current legislation and regulations (Institutional ethical standards of the responsible committee, and the Helsinki Declaration of 1975). Upon recovery, informed consent was sought from the patients.
Patients
All consecutive ICU COPD patients admitted between 2015 and 2021 were screened. Only patients over 40 years of age admitted for a severe acute exacerbation of COPD were included in the study. A severe acute exacerbation was defined by the presence of acute respiratory failure and/or hypercapnic acidosis. Exclusion criteria were admission to the ICU for reasons other than acute exacerbation of COPD, known asthma according to international definition, patient refusal to participate and early readmission in ICU for a relapse. We excluded patients with a withdrawing care decision during the first 24 hours after ICU admission.
We compared patients with a decision of withholding life-support during their ICU stay (named “WLS group”) to patients without these type decisions (named “no-WLS” group).
Patients management in ICU and ventilatory support according to good clinical practices and guidelines has been described in a previous publication related to this cohort.20
Data Collection
As previously described,20 the retrospective data obtained from medical records included: demographics, COPD characteristics, coexisting conditions, immunodeficiency, triggering factor for COPD exacerbation, usual performance status (PS), Simplified Acute Physiology Score II (SAPS II), vital parameters, laboratory tests, type and duration of ventilatory support, type of care of organ failure, patients self-decision of advance care planning prior to ICU admission, collegial decision of withholding of care during ICU stay and their type if specified (no cardio-pulmonary resuscitation, no orotracheal intubation, no reintubation after successful weaning of invasive mechanical ventilation, no vasopressor use, no renal replacement therapy, no future admission in ICU after discharge), ICU and hospital lengths of stay, and mortality rates at different endpoints.
Withholding/Withdrawing of Life-Support and Decision Process
In France, the SRLF (French Intensive Care Society) proposed guidelines in 2008 summarized in Figure S1, which are based on the French law of April the 22th 2005.21 In the ICU at Versailles hospital, the life-sustaining decision process is based on these good practice recommendations and requires a consensus of all participants (medical and paramedical) as well as the opinion of a physician from outside the ICU before the decision is made. Withholding of life-support decisions have been taken during dedicated ethical collegial meetings.
Statistical Analysis
Descriptive data are presented as absolute values (%) for categorical data and as medians with interquartile ranges (IQR) for continuous variables.
We performed a comparison according to the occurrence of the decision of withholding intensive care. We used the χ2 test or Fisher’s exact test for categorical variables and Student’s t-test or the Wilcoxon t-test for continuous variables (according to their distribution).
To identify the risk factors associated with a decision of limitation of care, we performed a multivariate analysis with a logistic regression model. The set of variables with a p-value < 0.20 in the univariate analysis was then included in the initial model and submitted to an automated process of variable selection known as stepwise. All of them could not be included in the multivariable model because of a strong collinearity. Once the final model was in place, residuals analysis was assessed graphically and interactions were sought. We used the Hosmer-Lemeshow test to assess the model goodness-of-fit.
Then, we performed survival analyses to identify the risk factors associated with 90-days mortality. As “Death at day 90” is a date in point and known for all the patients, we used a Cox model. Nevertheless, as some variables can change during the ICU stay, the latter were considered as time-dependent covariates. All the covariates presenting a p-value < 0.20 in a univariate manner were used, for the construction of the multivariate model. The same method was used to obtain a final logistic regression model. In addition to assuming proportionality of risk, log linearity hypothesis was tested for all survival analyses. As the withholding status changed over time in the cohort, we plotted survival curves by landmark time (Day 0, Day 1, Day 2, and Day 3). Only patients whose withholding status was defined before or at the respective landmark time were included in the corresponding survival curve.22
We performed a complete case analysis for variables with less than 5% of missing data. For variables with 5% to 30% missing data, we performed a multiple imputation by chained equation.23 No variable with more than 30% missing data was imputed; these variables were excluded from the multivariable analysis.
We conducted all tests with an alpha risk of 0.05 in a 2-tailed fashion. We performed analyses with the statistical software R4.3.1© (R foundation© for Statistical Computing Vienna, Austria).
Results
Patient Characteristics
Figure 1 is the patient flowchart and Table 1 reports patients characteristics at ICU admission. We included 463 patients, of whom 299 (64.6%) were men with a median age of 69 (IQR, 62–77) years. The GOLD stage (1 to 4, according to 2024 GOLD Report) was known for 375 (80.1%) patients and was ≥3 for 260 (56.2%) patients. The Performance Status (PS) score at admission was very altered (stage 4) or altered (stages 3 and 2) for 2 patients out of 3. Sixty-six (14.3%) patients had already been intubated for an exacerbation of COPD and only forty-eight (10.4%) reported advanced directives of care. Finally, 107 (23.1%) patients were considered as immunosuppressed in a significantly higher proportion in the group with WLS decision (36.7% vs 17.9%, p < 0.001). One hundred and twenty-eight (27.6%) patients had a decision of withhold life-sustaining treatment. Patients were significantly older in the WLS decision group (p < 0.001). There were significantly more patients treated with long-term oxygen therapy and systemic corticosteroids in the WLS decision group (p < 0.001 for both variables). The serum albumin was significantly lower in the WLS decision group (29 vs 32 g/L, p = 0.001). The median SAPS II was 38 (IQR, 31–49) and significantly higher in the WLS decision group (p < 0.001).
 |
Table 1 Baseline and Intensive Care Unit (ICU) Characteristics in Patients Admitted for a Severe Acute Exacerbation of COPD |
 |
Figure 1 Flow chart. Abbreviations: COPD, Chronic obstructive pulmonary disease; ICU, Intensive care unit. |
ICU Management and Outcomes
Table 2 reports ICU management and outcomes. NIV was initiated in 409 (88.3%) patients, with 101 (26%) failures with statistically more failure in the decision of limitation group (35.7% vs 21.9%, p = 0.001). One hundred and thirty-seven (29.6%) patients were intubated. Median duration of NIV was 3 days (IQR = 2–5) and invasive MV was 6 days (IQR = 3–13). Median length of stay in ICU was 6 days (IQR, 4–9) and was similar between the two groups. Thirty-six (7.8%) patients died in the ICU and 56 (12.1%) died in the hospital. At 3 months, 79 (17.1%) patients were deceased, 63 of which were in the withholding of care decision group (p < 0.001). The temporal distribution of mortality according to the Kaplan–Meier survival analysis at landmark day 0 is illustrated in the Figure 2.
 |
Table 2 ICU Management and Outcomes in Patients Admitted for a Severe Acute Exacerbation of COPD |
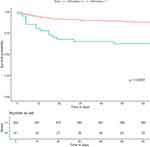 |
Figure 2 Kaplan–Meier 3-month survival curves for patients with and without a decision to withhold care at landmark time day 0. |
Data Concerning the Withholding of Life-Support-Decisions
The median delay of collegial meetings for withholding decisions was 1 [0–3] day. Table S1 shows the various types of WLS decided during ICU stay and their distribution. The most relevant decision is related to intubation, the main topic for COPD patients. This specific decision concerns 83 (64.8%) out of the 128 patients with a decision of withholding of care and 83 (100%) of the 127 patients who were not intubated in the WLS group. For the 45 intubated patients, 44 (97.8%) had a decision to not being re-intubate after successful weaning. All withholding of care decision during ICU stay match with patient’s self-advanced directive when noticed. Only twenty-six patients had a second ethical meeting leading to 22 decisions of withdrawing of care and 100% hospital mortality. Figure S2 shows the different end-point mortality for patients with and without WLS according to the ventilator support during ICU. Figure S3 illustrates the Kaplan–Meier survival at landmark day 1, day 2, and day 3 to consider the decision-making time of withhold care.
Table 3 reports patient characteristics at ICU admission according to a “do not intubate” decision. The characteristics between the two groups are similar when comparing WLS decision groups, excepted for age, long-term steroids use, long-term oxygen therapy, the GOLD stage, the PS, and immunodeficiency that all appear significantly higher in the “do not intubate” group (p < 0.05).
 |
Table 3 Baseline and ICU Characteristics in Patients According to the “Do Not Intubate” Decision |
Factors Associated with the Withholding of Life-Support Decision
In multivariable analysis, five variables were independently associated with the decisions of withholding of care: higher age (CI 95% = 1.49–2.52, OR = 1.93/+10 years, p < 0.001), immunodeficiency (CI 95% = 1.79–5.32, OR = 3.07, p < 0.001), higher PS score (CI 95% = 1.56–2.87, OR = 2.10/+1 point, p < 0.001), long-term oxygen therapy (CI 95% = 2.45–7.00, OR = 4.11, p < 0.001) and presence of shock during the first 48-hours after ICU admission (CI 95% = 1.25–4.74, OR = 2.43, p = 0.009) (Table 4). The odds ratio of advanced healthcare directives is not filled as all patients with advanced directives (n = 48) have had a decision of WLS, whatever the type.
 |
Table 4 Logistic Regression Analysis of Predictive Factors Associated Decision of Withholding of Care in ICU |
Factors Associated with 3 Months Mortality
Table S2 reports factors independently associated with 3 months mortality: a decision of WLS during ICU (CI 95% = 11.19–47.17, CSH = 22.98, p < 0.001) and the use of invasive mechanical ventilation (CI 95% = 1.58–4.70, CSH = 2.72, p > 0.001). Age, immunodeficiency, long-term steroids, and long-term oxygen therapy were not significantly associated with 3 months mortality in this multivariable model. An increasing serum albumin level was inversely associated with mortality at day-90 (CI 95% = 0.92–0.98, CSH = 0.95, p < 0.008).
Discussion
To the best of our knowledge, this is the first study to provide detailed information on predictive factors of decision-making of withhold life-support in patients admitted to the ICU for a severe acute exacerbation of COPD.
The baseline characteristics of our patients are similar to the literature on age (60 to 70 years old), majority of male gender,15–17 severe COPD stage, and high PS score attesting to severe chronic pulmonary diseases.5,18,19 Almost 30% of our patients experienced a decision of withholding of care, 65% of which on the orotracheal intubation as compared to a do not intubate decision for 22% of a previous study on critically ill COPD patients.24 Despite the lack of data and inter-studies variability, our results are consistent with the literature.5,16 Ten and a half percent of our patients reported self-advanced directives prior to their admission, a similar number to the actual French Regional Health Agency data25 and to another cohort in 2015.26
In severe exacerbations of COPD, non-invasive ventilation is a cornerstone of critical care management. The results showed that 88.2% of patients had NIV with a failure rate of 26.9% as previously reported.27–29 Heterogeneity of NIV failure between cohorts may be related to patients’ demographics but it may also vary according to the ethical decisions about ICU admissions, or the definition of NIV failure in case of withhold/withdrawal care. These crucial decisions are rarely described in the literature, making the comparison between the different studies difficult. In our cohort, invasive MV was necessary for 29.4% of patients with a median duration of invasive MV, length of stay in ICU and in hospital of 6, 5.5, and 11 days respectively, similar to previous studies.5,27,28,30
In the group of patients with WLS decisions, the withholding of organ life-support decisions were no-CPR, and no renal replacement therapy in 100%, and 76% of cases respectively. Most of studies mainly describe withholding of therapies decisions concerning CPR or intubation. This seems understandable, given that these decisions are the most relevant for critically ill COPD patients. The factors associated with decision of WLS treatment were higher age, immunodeficiency, higher PS score, long-term oxygen therapy, and presence of shock during the first 48h after ICU admission. However, the COPD GOLD stage did not significantly impact the decision. This results can be explained by collinearity effect between COPD stage and a long-term oxygen therapy or its impact on the PS score, all related to frailty.31 We brought out a PS ≥ 2 in 65% of the patients and GOLD stage ≥3 in 69% of the patients. It is likely these two variables jointly evolve and participate in the decision-making process of WLS.
All the patients with self-advanced directives in our study have had a decision of withhold therapies, making it impossible to realize a logistic regression analysis. This is partly explainable by the low percentage of patients having written such directives in our cohort, result supported by previous studies.26,32,33 This study being retrospective, we do not have a systematic collection of patients’ self-anticipated directives. Some could have written them without the medical team’s knowledge because this question did not seem relevant to the physicians in the absence of scheduled ethical meeting. These results reinforce the importance of advanced healthcare directives, general information to the public, their invaluable help for physicians and the imperative need to pursue studies. It is even more important considering growing vulnerable populations in ICU, with chronic severe respiratory diseases reporting high mortality rate.34
In medical literature, few studies have described factors correlated to a decision-making of withholding of treatment within specific groups of ICU patients, such as post-operative, neurological, trauma or end-stage renal disease patients.32–35 The associated factors are most often higher age, severe comorbidities and high severity scores during the first 48 hours.36 The relevance of our ICU cohort is the lack of data on factors associated with decision-making in a COPD population.
We observed 7.8% ICU mortality, 12.1% hospital mortality, 17.1% 90-days mortality and 27.9% 1-year mortality. In the literature, we can observe a certain degree of variability. Berenyi et al and Brown et al reported ICU mortality rates of 13.6% and 11.5% but hospital mortality rates of 26% and 18.7%, respectively.28,37 Nevertheless, our results seem homogeneous with a meta-analysis displaying ICU mortality rates from 7% to 25% and hospital mortality rates from 11% to 40%.30 Concerning COPD patients long-term survival, the amount of date is more limited.38 In most studies, 30 days-mortality ranges from 15% to 20% and 1 year-mortality varies from 30% to 45%.39–41
In this study, the mortality rate at day 90 was 17.1% but almost 50% in the withholding of care group and close to 5% in the group without such decision. Although patients over 80 years old are supposed to be non-frail and well selected for ICU admission, this high mortality rate can be partly explained by the high proportion of patients over 75 years old in the withholding of care group. Seneff et al reported a doubled mortality at 1 year for patients over 65 years.42 In a prospective study on 832 patients, Wildman et al reported 52% of mortality at 6-months for patients with a “do no intubate” decision versus 18% in the “not intubated and not limited patients” group and 45% for intubated patients. Their patients with a withholding of treatment decision, were significantly older (70 versus 66 years old).24
The variables significantly associated with 3-months mortality were WLS decision during ICU and the use of invasive mechanical ventilation. Age, immunodeficiency, long-term steroids, and long-term oxygen therapy (related to COPD severity) were not independently correlated to 3-months mortality in this multivariate model. The major role of “withholding of care decision” eventually induced a bias in our statistic model because age, immunodeficiency, and higher COPD severity are positively associated with the decision-making process of WLS. Once the WLS decision has been taken, these variables do not influence anymore mortality in multivariate analysis whereas these variables influence mortality in other studies.27,43,44 However, Messer et al review did not report age, functional status or long-term oxygen therapy as independent factors associated with 6-months mortality in critically ill COPD patients.30 Invasive MV exposes patients to an increased risk of complications and longer hospital stay.14 It is therefore reasonable to expect that intubation is associated with excess mortality. Wildman et al described invasive MV as an independent risk factor of mortality.24 Other studies did not report such an association.30,42,45 Improvements in the management of patients under invasive MV in recent decades have led to a reduction in mortality and could explain divergent results in the literature. Galerneau et al in a retrospective study on 1816 COPD patients in ICU described a major decrease of the 3-months mortality from 41% in 1997 to 22% in 2018, including intubated patients.4
Firstly, this article raises awareness of this issue in COPD patients, which is an original contribution. Secondly, it provides an overview of this ethical challenge, highlighting that the frailest patients subject to a withholding care decision have a very poor short- and medium-term prognosis. This raises important questions about how these patients should be managed in the ICU and underscores the need to anticipate such decisions as much as possible before hospitalization.
At present, it remains difficult to provide clinicians with a simple set of criteria or a scoring system to guide these complex decisions. However, the long-term goal is to move in that direction. While this article does not claim to achieve that, it addresses a crucial issue and offers valuable preliminary data.
Besides its strength, our study has several limitations. First, as a French monocentric and retrospective study, the interpretation, and extrapolation of our results are limited. French health care procedures could not be interpreted as it nor be implemented in other countries on a routine basis. Second, the “decision of withholding of care” is a time-dependent variable, considering it can appear during the time in ICU. It can induce an immortality bias on the survival analyses but we supposed that the decision-making depended mostly on factors already known at the admission, which is partly incorrect. However, the median period for this decision since ICU admission was 1 day, and we performed survival curves at different landmark time (from day 0 to day 3) with similar significant results supporting our analysis. Third, we did not analyse factors associated with each type of withholding of organ-life-support decision. Samples of subgroups were too small to allow a relevant analysis and focusing about “do not intubate” decision seems the more accurate in a COPD population. Fourth, we studied the mid- and long-term mortality but, as the study is retrospective, we could not collect information on quality of life for surviving patients. Finally, the last limit is the potential subjectivity in its interpretation and application. It seems difficult to be exhaustive in the collection of data that have led the caregivers to decide limitations of life-sustaining treatment. Moreover, we cannot exclude mortality biases related to self-fulfilling prophecy after withholding of care decision. This study is part of an evidence-based approach and help to the caregivers when he takes such important decisions, but it cannot replace the ethic dimension of collegial meetings and the liberty of the medical team in the decision-making process.
Conclusion
Acute severe exacerbations are a leading cause of morbidity and mortality in COPD patients following ICU admission. Factors associated with decisions to withhold life-sustaining treatment include advanced age, immunodeficiency, higher PS scores, and long-term oxygen therapy. Nearly half of the patients died within three months after a decision to withhold care. This study highlights the potential role of advanced healthcare directives in guiding a withholding of care decision. Given the substantial burden of severe acute exacerbations of COPD, early identification of factors, which can help the decision to withhold life-support care and associated to mortality is crucial. Such an approach could facilitate proactive care planning project before or during hospitalization. Larger prospective studies are warranted to further explore and validate these findings.
Data Sharing Statement
The investigators will make the documents and individual data strictly required for monitoring, quality control, and audit of the study available to dedicated persons, in accordance with laws and regulations in force (Articles L.1121-3 and R.5121-13 of the Code de Santé Publique – CSP, French Public Health Code).
The datasets used and/or analysed during the study will be available from the coordinating investigator (Alexis Ferré) on reasonable request. The procedures carried out under the French data privacy authority (Commission Nationale de l’Informatique et des Libertés) do not permit the transmission of the database, nor do the informed consent documents signed by the patients. Consultation by the editorial board or interested researchers of individual participant data that underlie the results reported in the article after deidentification may nevertheless be considered, subject to prior determination of the terms and conditions of such consultation and in respect of compliance with the applicable regulations.
Ethics Approval and Consent to Participate
This single-centre, observational, retrospective study was approved by the ethics committee of the French Intensive Care Society (N° #21-66) and registered at the French National Institute for Health Data (#MR 2516271119). Informed consent was sought from the patients upon recovery, in compliance with French law.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas. All authors took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for this study.
Disclosure
Matthieu Jamme reports honoraria by Sanofi for a lecture during JAMIR Congress 2022, outside the submitted work. Stéphane Legriel reports consulting fees from Becton Dickinson and meeting invitation from UCB, outside the submitted work. Alexis Ferré reports honoraria by Fisher & Paykel for a lecture during SFMU Congress 2022, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Agusti A. Global Initiative for Chronic Obstructive Lung Disease. About GOLD. 2023;2023:1.
2. Davidson AC, Staab D. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax. 2016;71(2):1–35. doi:10.1136/thoraxjnl-2015-208209
3. Halpin DM, Miravitlles M, Metzdorf N, Celli B. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J Chron Obstruct Pulmon Dis. 2017;12:2891–2908. doi:10.2147/COPD.S139470
4. Galerneau L-M, Bailly S, Terzi N. Management of Acute Exacerbations of Chronic Obstructive Pulmonary Disease in the ICU: an Observational Study From the OUTCOMEREA Database, 1997–2018. Crit Care Med. 2023;51(6):753–764. doi:10.1097/CCM.0000000000005807
5. Warwick M, Fernando SM, Aaron SD. Outcomes and Resource Utilization Among Patients Admitted to the Intensive Care Unit Following Acute Exacerbation of Chronic Obstructive Pulmonary Disease. J Intensive Care Med. 2021;36(9):1091–1097. doi:10.1177/0885066620944865
6. Schmidt M. Intensive care unit admission in chronic obstructive pulmonary disease: patient information and the physician’s decision-making process. Crit Care Lond Engl. 2014;18(3):R115. doi:10.1186/cc13906
7. Fu P-K. Early Do-Not-Resuscitate Directives Decrease Invasive Procedures and Health Care Expenses During the Final Hospitalization of Life of COPD Patients. J Pain Symptom Manage. 2019;58(6):968–976. doi:10.1016/j.jpainsymman.2019.07.031
8. Iyer AS, Sullivan DR, Lindell KO, Reinke LF. The Role of Palliative Care in COPD. Chest. 2022 ;161(5): 1250–1262. doi:10.1016/j.chest.2021.10.032
9. Beernaert K, Cohen J, Deliens L. Referral to palliative care in COPD and other chronic diseases: a population-based study. Respir Med. 2013;107(11):1731–1739. doi:10.1016/j.rmed.2013.06.003
10. Rush B, hertz P, Bond A, McDermid RC, Celi LA. Use of Palliative Care in Patients With End-Stage COPD and Receiving Home Oxygen: national Trends and Barriers to Care in the United States. Chest. 2017;151(1):41–46. doi:10.1016/j.chest.2016.06.023
11. Casanova C, de Torres JP, Aguirre-Jaíme A. The progression of chronic obstructive pulmonary disease is heterogeneous: the experience of the BODE cohort. Am J Respir Crit Care Med. 2011;184(9):1015–1021. doi:10.1164/rccm.201105-0831OC
12. Vidal AC, Pandiella A. COPD. A model for using advanced directives and care planning. Arch Bronconeumol. 2010;46(6):325–331. doi:10.1016/j.arbres.2009.12.001
13. Mulcahy P, Buetow S, Osman L. GPs’ attitudes to discussing prognosis in severe COPD: an Auckland (NZ) to London (UK) comparison. Fam Pract. 2005;22(5):538–540. doi:10.1093/fampra/cmi052
14. Burns KEA. Non-invasive ventilation versus invasive weaning in critically ill adults: a systematic review and meta-analysis. Thorax. 2022;77(8):752–761. doi:10.1136/thoraxjnl-2021-216993
15. Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(7):477–489. doi:10.1016/j.jamda.2014.01.008
16. Mark NM, Rayner SG, Lee NJ, Curtis JR. Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Intensive Care Med. 2015;41(9):1572–1585. doi:10.1007/s00134-015-3810-5
17. Morgan J. How do you decide when to withdraw life support? Lancet Respir Med. 2015;3(6):430–431. doi:10.1016/S2213-2600(15)00189-7
18. Article L 1110-5 du Code de Santé Publique. 2005.
19. van Veen E. End-of-life practices in traumatic brain injury patients: report of a questionnaire from the CENTER-TBI study. J Crit Care. 2020;58:78–88. doi:10.1016/j.jcrc.2020.04.001
20. Abdallah GA, Diop S, Jamme M, Legriel S, Ferré A. Respiratory Infection Triggering Severe Acute Exacerbations of Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2024;19:555–565. doi:10.2147/COPD.S447162
21. Villers D, Renault A, Le Gall G, Boles J-M. SRLF. Witholding and withdrawing of life support in Intensive Care Unit: How evaluate our pratices. Reanimation. 2010;19:706–717. In French.
22. Putter H, van Houwelingen HC. Understanding Landmarking and Its Relation with Time-Dependent Cox Regression. Stat Biosci. 2017;9(2):489–503. doi:10.1007/s12561-016-9157-9
23. Little R, Rubin D. Statistical Analysis with Missing Data. In: Wiley Series in Probability and Statistics.
24. Wildman MJ, Sanderson CFB, Groves J. Survival and quality of life for patients with COPD or asthma admitted to intensive care in a UK multicentre cohort: the COPD and Asthma Outcome Study (CAOS. Thorax. 2009;64(2):128–132. doi:10.1136/thx.2007.091249
25. ARS. Directives anticipées. 2019. Available from: https://www.ars.sante.fr/les-directives-anticipees-faites-savoir-vos-volontes.
26. Stefan MS, Nathanson BH, Higgins TL. Comparative Effectiveness of Noninvasive and Invasive Ventilation in Critically Ill Patients With Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Crit Care Med. 2015;43(7):1386–1394. doi:10.1097/CCM.0000000000000945
27. Gadre SK, Duggal A, Mireles-Cabodevila E. Acute respiratory failure requiring mechanical ventilation in severe chronic obstructive pulmonary disease (COPD. Medicine. 2018;97(17):e0487. doi:10.1097/MD.0000000000010487
28. Berenyi F, Steinfort DP, Abdelhamid YA. Characteristics and Outcomes of Critically Ill Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease in Australia and New Zealand. Ann Am Thorac Soc. 2020;17(6):736–745. doi:10.1513/AnnalsATS.201911-821OC
29. Ongel EA, Karakurt Z, Salturk C. How do COPD comorbidities affect ICU outcomes? Int J Chron Obstruct Pulmon Dis. 2014;9:1187–1196. doi:10.2147/COPD.S70257
30. Messer B, Griffiths J, Baudouin SV. The prognostic variables predictive of mortality in patients with an exacerbation of COPD admitted to the ICU: an integrative review. QJM Mon J Assoc Physicians. 2012;105(2):115–126. doi:10.1093/qjmed/hcr210
31. Oken MM, Creech RH, Tormey DC. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655. doi:10.1097/00000421-198212000-00014
32. Kirschner KL. When Written Advance Directives are not Enough. Clin Geriatr Med. 2005;21(1):193–209. doi:10.1016/j.cger.2004.08.006
33. Hartog CS, Peschel I, Schwarzkopf D. Are written advance directives helpful to guide end-of-life therapy in the intensive care unit? A retrospective matched-cohort study. J Crit Care. 2014;29(1):128–133. doi:10.1016/j.jcrc.2013.08.024
34. Gamertsfelder EM, Seaman JB, Tate J, Buddadhumaruk P, Happ MB. Prevalence of Advance Directives Among Older Adults Admitted to Intensive Care Units and Requiring Mechanical Ventilation. J Gerontol Nurs. 2016;42(4):34–41. doi:10.3928/00989134-20151124-02
35. Nathens AB, Rivara FP, Wang J, Mackenzie EJ, Jurkovich GJ. Variation in the rates of do not resuscitate orders after major trauma and the impact of intensive care unit environment. J Trauma. 2008;64(1):81–88. doi:10.1097/TA.0b013e31815dd4d7
36. Skjaker SA, Hoel H, Dahl V, Stavem K. Factors associated with life-sustaining treatment restriction in a general intensive care unit. PLoS One. 2017;12(7):e0181312. doi:10.1371/journal.pone.0181312
37. Brown H, Dodic S, Goh SS. Factors associated with hospital mortality in critically ill patients with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:2361–2366. doi:10.2147/COPD.S168983
38. Prediletto I, Giancotti G, Nava S. COPD Exacerbation: why It Is Important to Avoid ICU Admission. J Clin Med. 2023;12(10):3369. doi:10.3390/jcm12103369
39. Teixeira C. Patients admitted to the ICU for acute exacerbation of COPD: two-year mortality and functional status. J Bras Pneumol Publicacao of Soc Bras Pneumol E Tisilogia. 2011;37(3):334–340. doi:10.1590/s1806-37132011000300009
40. Portier F, Defouilloy C, Muir J-F. Determinants of Immediate Survival among Chronic Respiratory Insufficiency Patients Admitted to an Intensive Care Unit for Acute Respiratory Failure. Chest. 1992;101(1):204–210. doi:10.1378/chest.101.1.204
41. Gungor S, Mocin OY, Tuncay E. Risk factors of unfavorable outcomes in chronic obstructive pulmonary disease patients treated with noninvasive ventilation for acute hypercapnic respiratory failure. Clin Respir J. 2020;14(11):1083–1089. doi:10.1111/crj.13245
42. Seneff MG. Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274(23):1852–1857. doi:10.1001/jama.1995.03530230038027
43. Ranieri P, Bianchetti A, Margiotta A, Virgillo A, Clini EM, Trabucchi M. Predictors of 6-Month Mortality in Elderly Patients with Mild Chronic Obstructive Pulmonary Disease Discharged from a Medical Ward After Acute Nonacidotic Exacerbation: COPD EXACERBATION AND MORTALITY IN ELDERLY PATIENTS. J Am Geriatr Soc. 2008;56(5):909–913. doi:10.1111/j.1532-5415.2008.01683.x
44. Bustamante-Fermosel A, De Miguel-Yanes JM, Duffort-Falcó M, Muñoz J. Mortality-related factors after hospitalization for acute exacerbation of chronic obstructive pulmonary disease: the burden of clinical features. Am J Emerg Med. 2007;25(5):515–522. doi:10.1016/j.ajem.2006.09.014
45. Ucgun I, Metintas M, Moral H, Alatas F, Yildirim H, Erginel S. Predictors of hospital outcome and intubation in COPD patients admitted to the respiratory ICU for acute hypercapnic respiratory failure. Respir Med. 2006;100(1):66–74. doi:10.1016/j.rmed.2005.04.005
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Lack of COPD-Related Follow-Up Visits and Pharmacological Treatment in Swedish Primary and Secondary Care
Sandelowsky H, Janson C, Wiklund F, Telg G, de Fine Licht S, Ställberg B
International Journal of Chronic Obstructive Pulmonary Disease 2022, 17:1769-1780
Published Date: 9 August 2022
The Effect of Maintenance Treatment with Erdosteine on Exacerbation Treatment and Health Status in Patients with COPD: A Post-Hoc Analysis of the RESTORE Dataset

Calverley PMA, Papi A, Page C, Rogliani P, Dal Negro RW, Cazzola M, Cicero AF, Wedzicha JA
International Journal of Chronic Obstructive Pulmonary Disease 2022, 17:1909-1920
Published Date: 22 August 2022
Six-Minute Walking Test and 30 Seconds Chair-Stand-Test as Predictors of Mortality in COPD – A Cohort Study
Höglund J, Boström C, Sundh J
International Journal of Chronic Obstructive Pulmonary Disease 2022, 17:2461-2469
Published Date: 4 October 2022
Clinical Characteristics and Outcomes of Eosinophilic Exacerbations of COPD
Donnan M, Liu TL, Gvalda M, Chen X, Foo CT, MacDonald MI, Thien F
International Journal of Chronic Obstructive Pulmonary Disease 2025, 20:1061-1070
Published Date: 13 April 2025
Characteristics and Outcomes of People With COPD Who Experience Exacerbations While on Inhaled Triple Therapy: Results of the SIRIUS I Cohort Study in the US (2015–2019)
Nordon C, Carstens D, Fagerås M, Müllerová H, Veeranki PS, Alves JA, Germack HD, Barnes TL, McCormack MC
International Journal of Chronic Obstructive Pulmonary Disease 2025, 20:1851-1864
Published Date: 11 June 2025

