Back to Journals » Advances in Medical Education and Practice » Volume 16
Impact of an Extracurricular Research Course on Medical Students: A Quasi-Experimental Study
Authors Alnajjar JS , Alabdulqader RA, Alhithlool AW, Almarzooq MA, Alshakhs AA , Al-Omair AM, Ali SI, Almaqhawi A
Received 15 December 2024
Accepted for publication 16 March 2025
Published 25 March 2025 Volume 2025:16 Pages 461—470
DOI https://doi.org/10.2147/AMEP.S509323
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Md Anwarul Azim Majumder
Jawad S Alnajjar,1 Razan Anwar Alabdulqader,1 Abdulmalek W Alhithlool,1 Mohammed A Almarzooq,1 Abdullah Afif Alshakhs,1 Abdullah Mohammed Al-Omair,1 Sayed Ibrahim Ali,2 Abdullah Almaqhawi2
1College of Medicine, King Faisal University, Alahsa, Saudi Arabia; 2Department of Family and Community Medicine, College of Medicine, King Faisal University, Al Hofuf, Saudi Arabia
Correspondence: Jawad S Alnajjar, College of Medicine, King Faisal University, Alahsa, Saudi Arabia, Email [email protected]
Introduction: Research is a fundamental component for advancing healthcare and medical knowledge. It enhances students’ ability to practice evidence-based care in clinical practice. Despite the recognized benefits, barriers such as lack of time, skills, funding, and guidance impede students’ involvement in research. This study aims to evaluate the effectiveness and impact of conducting a specialised extracurricular research course designed for medical students at King Faisal University.
Patients and Methods: A quasi-experimental study utilized a pretest-posttest design, including a control group. Participants were second-to-sixth-year medical students, divided into an intervention group and a control group. The intervention group participated in a comprehensive research course over eight months. A pretest-posttest self-administered questionnaire was given at the beginning and end of the course to assess research knowledge and attitudes. The control group completed the same at equivalent time points.
Results: The paired sample t-test demonstrated significant improvements in pre- and post-test scores for research knowledge among students who attended more than 50% of the course (p = 0.009). Similarly, students who attended less than or equal to 50% of the course content also showed significant gains in research knowledge (p = 0.005). However, the comparison between the intervention and control groups did not show a significant difference (p = 0.160).
Conclusion: This study highlights the effectiveness of a structured research training program in enhancing medical students’ research knowledge and attitudes. The findings advocate for integrating formal research training into medical curricula to prepare future healthcare professionals for evidence-based practice and sustained research engagement. Despite limitations such as non-randomized assignments and a single-institution focus, the study underscores the transformative impact of systematic research education on medical students’ professional development.
Keywords: academic development, extracurricular, medical education, medical students, pretest-posttest, quasi-experimental study, research
Introduction
Research is a very important aspect of enhancing medical services and medical development.1 It is defined as a systematic process to achieve new knowledge, science, or invention by the use of standard methods.2 It plays a crucial role in acquiring knowledge in biological and medical sciences.3 Acquiring research knowledge about performing research enables students to decide based on evidence-based medicine in healthcare practice.4 Furthermore, active engagement in research activities contributes to the continuous improvement of healthcare standards.5
Every healthcare student is expected to have the ability to execute research in order to attain professional accomplishments and gain crucial understanding.5 Participation in research has been found to have a positive impact on students’ critical thinking and communication skills.6 Similarly, engaging in research courses has been proven to enhance students’ beliefs regarding science in the short term.7 A previous study indicated that medical students with research experience outside the curriculum tend to conduct further papers post-graduation compared to those without such experience.8 However, for the purpose of publishing medical research, possessing a comprehensive understanding of research ethics, applicable techniques, and constrictive views is mandatory.9–11 In addition, several barriers hinder research engagement, including insufficient time, limited skills and expertise, inadequate access to funding and resources, lack of proper guidance from teaching staff, restricted access to medical journals and relevant databases, and insufficient motivation to pursue research activities.5,12,13 Several prior studies have emphasized the benefits and advantages of research training specifically tailored for medical students.14,15 Goto et al established a research program across various universities in Vietnam and concluded that learning and practicing research is a valuable and reliable strategy.16 A subsequent study done by the University of Calgary found a substantial rise in medical student research draft submissions from 11% to 59% following the implementation of a structured research program.17
At King Faisal University, medical students already follow a research curriculum that includes quarterly sessions and lectures on medical research. However, an exclusive course has been proposed to enhance their education, provide hands-on research experience, and support publishing efforts. This course aims to bridge the gap between theoretical knowledge and real-world application through a structured research program. Therefore, this study evaluates the effectiveness of an extracurricular research course designed specifically for medical students. Therefore, this research is both exclusive and crucial, as it provides valuable insights into how structured research programs can bridge the gap between theoretical knowledge and real-world application. This research aims to evaluate the effectiveness of an extracurricular research course specially designed for medical students.
Methods and Materials
Study Design
This is a quasi-experimental study that utilised a pretest-posttest design including a control group. The study used a self-administered questionnaire tailored to medical students to assess the impact of the extracurricular research course announced by the College of Medicine Research Club. The course consists of 20 educational hours and lasts for 4 days; Institutional Review Board approval was obtained, and the study spanned from September 2023 to April 2024.
Participants
The study sample comprised students from the Bachelor of Medicine and Surgery Program at King Faisal University, Saudi Arabia, specifically those in their second to sixth year out of a seven-year program. A total of 91 students participated in the study, divided into two main groups: the intervention group and the control group. The intervention group included students who voluntarily registered for the extracurricular research course announced by the College of Medicine Research Club. From a pool of 345 students, 145 were selected based on mentor availability and registration priority. Among these, 71 students (71/145; 49%) completed both the pretest and posttest questionnaires and were deemed eligible to participate in the study. The distribution of students by academic year was as follows:
- Second-year students: 8/71 (11.2%)
- Third-year students: 10/71 (14%)
- Fourth-year students: 16/71 (22.5%)
- Fifth-year students: 18/71 (25.3%)
- Sixth-year students: 19/71 (26.7%)
The 71 students in the intervention group were further subdivided based on their attendance and participation in the course:
- Group A: Forty-one students (41/71; 58%) attended Only one or two days, covering 50% or less of the course content.
- Group B: Thirty students (30/71; 42%) attended three or four days, covering more than 50% of the course content.
The control group consisted of 20 students (20/91; 22%) who neither registered for nor participated in the course. The participants were chosen through a convenience sampling method. Both the intervention group (71/91; 78%) and the control group (20/91; 22%) were included in the study’s analyses.
Data Collection
A self-designed questionnaire [supplementary file] was developed for this study after an extensive literature search,1,12,17,18 tailored to align with the course content. The relevance of the questionnaire was verified by expert faculty members. To ensure understandability, a pilot questionnaire was administered to a group of undergraduate students, resulting in modifications based on feedback from both the students and the experts. The reliability of the questionnaire was evaluated using Cronbach’s alpha, which produced a coefficient of (0.805), indicating good internal consistency. The questionnaire was divided into three sections: the first section comprised 9 items, gathering demographic information such as gender, age, and educational level. The second section consisted of 27 multiple-choice questions, designed to assess participants’ knowledge of the medical research in areas such as literature review, critical appraisal, research proposal development, research methodologies, research components, statistical analysis, and ethical considerations. The third section consisted of 12 items aimed at understanding participants’ attitudes towards medical research, with responses measured using a five-point Likert scale, ranging from strongly disagree (score-1) to strongly agree (score-5). In the pre-test, we distributed the questionnaire before the exposure to the first course lecture, and we distributed the post-test questionnaire after the last lecture. The data was collected through a Google Form, which was distributed to participants via WhatsApp. The collected data was securely stored in an Excel file, ensuring confidentiality and integrity throughout the process. Regarding the control group, they filled out the pre and post-questionnaire with the same interval without exposure to the course content.
Intervention
The study intervention group participated in a series of comprehensive lectures delivered by residents and consultants, spanning four days (Figure 1). These lectures were conducted at a rate of one day every two months, covering a total of six months during the academic year. Each instructional day lasted three to five hours of in person lectures, accumulating approximately 20 hours of instructional time. The first day highlights an overview of research steps, how to choose research ideas, how to read scientific papers, and a literature review. The second day highlights the research proposal, introduction section, research method, and IRB approval. The third day highlights the writing discussion, the SPSS program, and the results. The last day highlights writing abstracts and journal submissions. The concept behind the time intervals between each day of the course was to allow participants enough time to complete the tasks required of them before proceeding to the next day. Participants were randomly allocated into groups of 5–6 students, with each group assigned a mentor from the faculty who provided guidance and reviewed their work throughout the six months. By the end of the period, each group was required to complete a research paper.
 |
Figure 1 Overview of the Course Structure and Flow. |
Ethical Considerations
The study was reviewed and approved by the Institutional Review Board at King Faisal University, Al-Ahsa, Saudi Arabia (Ethics Approval No. KFU-REC-2023-SEP-ETHICS1517). Prior to participating, informed consent was obtained from all participants.
Statistical Analysis
Data were analysed using SPSS version 26.0 (IBM Corporation, Armonk, NY, US). Descriptive and inferential statistics were employed to analyze the data. Frequencies and percentages were calculated to summarize categorical variables such as gender, academic year, and obstacles faced in research engagement. For continuous variables, mean scores and standard deviations were computed to assess participants’ research knowledge and attitudes before and after the intervention.
Paired sample t-tests were conducted to evaluate changes in research knowledge and attitudes within each group (intervention and control) pre- and post-intervention. Independent sample t-tests were used to compare post-intervention scores between the experimental and control groups. Effect sizes were calculated to assess the magnitude of observed differences. The level of statistical significance was set at p < 0.05 for all tests.
Results
Table 1 presents the demographic characteristics of the study participants (N = 91), highlighting their distribution by gender, academic year, and the obstacles faced in research engagement. The gender distribution is nearly balanced, with 49.5% male and 50.5% female participants, ensuring diverse perspectives in the study. Participants were drawn from various academic years, with the largest group from Year 4 (30.7%), followed by Year 6 (23%) and Year 5 (21%). The smallest groups were from Year 3 (16.5%) and Year 2 (8.8%), indicating broad representation across the medical curriculum.
 |
Table 1 Participant Demographics (N = 91) |
A significant portion of students (41.8%) identified a lack of research training as a major obstacle to research engagement, highlighting a critical area for curricular improvement. Additionally, 35.2% of participants cited limited time due to academic commitments, underscoring the challenge of balancing research with rigorous medical studies. Inadequate mentorship (27.5%) and lack of funding/resources (20.9%) were also notable barriers.
Analysis of paired sample tests (Table 2) reveals changes in pre- and post-test scores among participants. For Group B, those attending more than 50% of the course, pre-intervention scores averaged 13.63 and increased to 16.00 post-intervention, reflecting a mean difference of −2.37 (p = 0.009). Group A, with an attendance of 50% or less, exhibited an increase in mean score from 12.78 to 15.51, resulting in a mean difference of −2.73 (p = 0.005). In contrast, the post-intervention comparison between the experimental group and the control group did not yield a statistically significant difference, with a mean difference of 2.75 (p = 0.160). Comprehensive statistics (Table 3) elucidate these findings, presenting standard deviations and error means that contextualise the variability and dependability of these measurements. For example, Group B (Pre) had a standard deviation of 6.61 and a standard error mean of 1.21, while Group B (Post) recorded a standard deviation of 5.51 and a standard error mean of 1.01.
 |
Table 2 Paired Sample Test for Intervention and Control Groups |
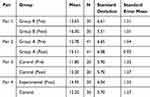 |
Table 3 Means Before and After for Interventional and Control Groups |
Before the intervention (Table 4), the attitudes toward medical research were generally positive among students. The highest mean score was 4.51 for the anticipation of participating in future research, while the statement regarding the enjoyment of research hours yielded a lower mean score of 3.32, indicating less enthusiasm for the process itself. The least agreement was noted for the statement that research could increase heat between classmates, with a mean score of 3.07. Following the intervention, there was a noticeable improvement in attitudes toward medical research. The statement about future participation in research achieved a mean score of 4.85, suggesting increased enthusiasm. The endorsement for mandatory research education also saw an increase, achieving a mean score of 4.46 post-intervention. Despite improvements, the enjoyment of research hours remained modest with a post-intervention mean score of 3.58, and concerns about research fostering discord among classmates marginally improved, with a post-intervention score of 2.86.
 |
Table 4 Participants’ Attitude Toward Medical Research Before the Intervention |
Discussion
The crucial importance of scientific research for advancing medical practice is widely recognized.1 To ensure appropriate collaboration in creating new literature and implementing optimal evidence-based care, all healthcare providers must be competent in every research element.4 Incorporating comprehensive medical research education into undergraduate programs has become a cornerstone of modern medical training. This approach aims to equip future healthcare professionals with critical research skills and a robust foundation of knowledge essential for navigating the complexities of evidence-based medicine.5 Our study aimed to analyze the effectiveness of establishing a dedicated healthcare student research school.
The main findings of this study indicate that the intervention group demonstrated a statistically significant improvement in research knowledge following the training course compared to their baseline scores. This improvement, as evidenced by the analysis of post-test knowledge scores, reflects an enhanced understanding of research principles among the course participants. However, when compared to the control group, the difference in post-test scores was not statistically significant. Previous studies have repeatedly shown that structured research training greatly improves medical students’ research knowledge and skills.1,14 Astonishingly, the study found no substantial difference in knowledge comparing the experimental group with the control group. This unexpected result aligns with findings by Eby et al, which suggest that the effectiveness of mentorship may vary based on factors such as the mentor’s expertise, the quality of the mentor-mentee relationship, and the duration of the mentoring program.19 These variables are critical in determining the success of mentorship interventions, as mismatches in expertise or poor mentor-mentee dynamics may reduce their impact. Additionally, one limitation of our study is the use of a non-randomized sampling method, which may have contributed to this finding. Non-randomized designs can introduce selection bias, as participants may possess inherent differences that influence outcome measures independently of the intervention.20
Our findings indicate that Group B had a higher pre-test mean knowledge score of approximately 13.63, compared to Group A and the control group, which had lower means of 12.78 and 12.20, respectively. This suggests that participants in Group B may have entered the study with a stronger foundation in research knowledge. The discrepancy in baseline knowledge between the groups could reflect differences in prior exposure to research concepts, educational backgrounds, or motivation levels. These factors might have influenced their initial readiness and ability to engage with the research course content effectively. Sabzwari et al highlighted a strong association between prior research involvement and current engagement, particularly among male participants and those working in the public sector.1 Additionally, doctors engaged in research were more likely to report positive attitudes toward it, while 83.5% of those not involved found it challenging.1 However, it remains unclear whether early research experiences in medical school stimulated later involvement or if pre-existing motivation drove both early and later participation.21
The intervention group demonstrated improved attitudes toward research, showing increased motivation and a more positive perspective on its importance in medical practice, aligning with the findings of Vujaklija et al.7 Additionally, other studies indicate that medical students would welcome training in academic writing.17 However, previous research has highlighted that despite generally positive attitudes toward research, there was a noticeable deficiency in practical skills, particularly in reading and writing academic literature.22 One of the most notable outcomes was the increased motivation to engage in research activities. The highest-rated post-intervention statement, “I will participate in researching in the future”, achieved a mean score of 4.85, showing a statistically significant improvement from pre-intervention levels and a significant difference between the control and intervention groups. This highlights the course’s effectiveness in encouraging and motivating participants to continue and pursue research in the future. Regrettably, there was noticeable ambivalence regarding the obligatory aspect of research, as indicated by the statement, “Research work should be made optional”, which received a mean score of 3.69. Although students acknowledged the importance of research, they exhibited reluctance to engage in it. For instance, a study by Burgoyne et al discovered that while many healthcare students appreciated the educational value of research, a significant proportion expressed discomfort with the mandatory nature of research projects, citing time constraints and the added pressure it placed on their already demanding schedules.23 Similarly, Amgad et al reported that students often viewed compulsory research as an additional burden, leading to mixed feelings about its inclusion in the medical curriculum.24
The study identifies lack of research training and limited time due to academic commitments as major barriers to research involvement, consistent with findings from previous studies by Alsaleem et al and Giri et al12,13 Additionally, prior studies have found a lack of time, disruption of normal studies, and the belief that student papers are rarely cited to be a barrier to medical students engaging in research.23 Notably, a previous study highlighted that interest in research among healthcare students declines as they advance in their academic years, further emphasizing time as a critical barrier.24 For participants who had not yet published, the primary obstacle was the lack of opportunity to initiate research projects, which consequently led to the perception that they had no work to submit for publication.17 Furthermore, when analyzing graduates as a whole, it was evident that those who had research opportunities during medical school were significantly more likely to pursue research in their postgraduate careers.21 These enduring difficulties highlight the necessity of comprehensive support networks to encourage student participation in research projects. Finally, these findings highlight how important it is to include formal research training in healthcare education and demonstrate how it improves students’ research knowledge, attitudes, and future involvement in research.
Limitation
This study has several limitations that should be considered when interpreting the findings. The quasi-experimental design with non-randomized group assignments may introduce selection bias and limit generalizability, and the single-institution setting at King Faisal University further restricts applicability to other populations. The low response rate may introduce non-response bias, potentially stemming from time constraints or survey fatigue. The reliance on self-reported questionnaires introduces the possibility of response bias, and while reliability was assessed using Cronbach’s alpha, further validation of the tool is needed. Additionally, the study’s pretest-posttest design does not capture long-term retention of knowledge or sustained changes in attitudes. Future research should include randomized designs, larger and more diverse samples, and longer follow-up periods to enhance the validity and applicability of the findings.
Conclusion
This research emphasises the efficacy of a structured research course at King Faisal University in substantially improving the research knowledge and attitudes of medical students. Nevertheless, there was no discernible distinction in the knowledge outcomes of the control and intervention groups. The results emphasise the significance of formal research training in preparing students for lifelong research engagement and evidence-based practice. Although the course demonstrated positive effects, such as the intervention group showing improved attitudes toward research, with increased motivation and a more positive perspective on its importance in medical practice, there are opportunities for improvement, such as overcoming participation barriers and enhancing engagement through curriculum refinement. Future research should investigate the long-term retention of research skills and attitudes and expand to multiple institutions.
Data Sharing Statement
Data is provided within the manuscript.
Ethics Approval and Consent to Participate
The study protocol was evaluated and approved by the Institutional Review Board at King Faisal University, Al-Ahsa, Saudi Arabia (Ethics Consent No. KFU-REC-2023-SEP-ETHICS1517), and informed consent was obtained from each participant before enrolment in the study.
Consent for Publication
Not applicable. No individual person’s data in any form (including individual details, images, or videos) are included in this manuscript.
Acknowledgments
We would like to thank the participants for their time and commitment to this study. We also extend our gratitude to King Faisal University for supporting this research project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia (Grant No. KFU242695).
Disclosure
The authors declare that they have no competing interests.
References
1. Sabzwari S, Kauser S, Khuwaja AK. Experiences, attitudes, and barriers towards research amongst junior faculty of Pakistani medical universities. BMC Med Educ. 2009;9:68. doi:10.1186/1472-6920-9-68
2. Memarpour M, Fard AP, Ghasemi R. Evaluation of attitude to, knowledge of and barriers toward research among medical science students. Asia Pac Fam Med. 2015;14(1):1. doi:10.1186/s12930-015-0019-2
3. Ávila MJ, Rodríguez-Restrepo A. The importance of research in undergraduate medical education. Medwave. 2014;14(10):e6032. doi:10.5867/medwave.2014.10.6032
4. Mahmoud Wahdan M. Medical students’ knowledge and attitude towards research in Ain Shams University: a cross-sectional study. Egypt Family Med J. 2019;3(1):1–16. doi:10.21608/efmj.2019.67519
5. AlSayegh AS, Enayah SK, Khoja WN, Enayah RK, Sendi NS. Assessment of the current knowledge and willingness to conduct medical research work of future healthcare providers: a cross-sectional study in Jeddah, Saudi Arabia. J Family Med Prim Care. 2020;9(3):1522–1527. doi:10.4103/jfmpc.jfmpc_1047_19
6. Lopatto D. Undergraduate research experiences support science career decisions and active learning. CBE Life Sci Educ. 2007;6(4):297–306. doi:10.1187/cbe.07-06-0039
7. Vujaklija A, Hren D, Sambunjak D, et al. Can teaching research methodology influence students’ attitude toward science? Cohort study and nonrandomized trial in a single medical school. J Investig Med. 2010;58(2):282–286. doi:10.2310/JIM.0b013e3181cb42d9
8. Reinders JJ, Kropmans TJ, Cohen-Schotanus J. Extracurricular research experience of medical students and their scientific output after graduation. Med Educ. 2005;39(2):237. doi:10.1111/j.1365-2929.2004.02078.x
9. Hicks C. A study of nurses’ attitudes towards research: a factor analytic approach. J Adv Nurs. 1996;23(2):373–379. doi:10.1111/j.1365-2648.1996.tb02681.x
10. Ajay S, Bhatt A. Training needs of clinical research associates. Perspect Clin Res. 2010;1(4):134–138. doi:10.4103/2229-3485.71771
11. Rajadhyaksha V. Training for clinical research professionals: focusing on effectiveness and utility. Perspect Clin Res. 2010;1(4):117–119. doi:10.4103/2229-3485.71767
12. Alsaleem SA, Alkhairi MAY, Alzahrani MAA, et al. Challenges and barriers toward medical research among medical and dental students at King Khalid University, Abha, Kingdom of Saudi Arabia. Front Public Health. 2021;9:706778. doi:10.3389/fpubh.2021.706778
13. Giri PA, Bangal VB, Phalke DB. Knowledge, attitude and practices towards medical research amongst the postgraduate students of pravara institute of medical sciences university of Central India. J Family Med Prim Care. 2014;3(1):22–24. doi:10.4103/2249-4863.130263
14. Al-Tannir M, Abu-Shaheen A, AlSumaih S, et al. Research knowledge and skills among medical and allied health students attending a summer research course: a pretest and posttest analysis. Cureus. 2018;10(8):e3132. doi:10.7759/cureus.3132
15. Ramjiawan B, Pierce GN, Iffat M, et al. How we teach: an international basic science and clinical research summer program for medical students. Adv Physiol Educ. 2012;36:27–33. doi:10.1152/advan.00056.2011
16. Goto A, Nguyen TN, Nguyen TM, Hughes J. Building postgraduate capacity in medical and public health research in Vietnam: an in-service training model. Public Health. 2005;119(3):174–183. doi:10.1016/j.puhe.2004.05.005
17. Griffin MF, Hindocha S. Publication practices of medical students at British medical schools: experience, attitudes and barriers to publish. Med Teach. 2011;33(1):e1–e8. doi:10.3109/0142159X.2011.530320
18. Ibrahim NK, Fetyani DM, Bashwari J. Assessment of research-oriented knowledge, attitude & practice of medical students and interns about research with implementation of educational intervention program, King Abdulaziz University, Jeddah. RMJ. 2013;38(4):432–439.
19. Eby LT, Allen TD, Evans SC, Ng T, Dubois D. Does mentoring matter? A multidisciplinary meta-analysis comparing mentored and non-mentored individuals. J Vocat Behav. 2008;72(2):254–267. doi:10.1016/j.jvb.2007.04.005
20. Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002.
21. Segal S, Lloyd T, Houts PS, Stillman PL, Jungas RL, Greer RB. The association between students’ research involvement in medical school and their postgraduate medical activities. Acad Med. 1990;65(8):530–533. doi:10.1097/00001888-199008000-00010
22. Aslam F, Qayyum MA, Mahmud H, Qasim R, Haque IU. Attitudes and practices of postgraduate medical trainees towards research--a snapshot from Faisalabad [published correction appears in J Pak Med Assoc. 2005 Jan;55(1):50. Qayyum, MA [corrected to Qayyum, MA]]. J Pak Med Assoc. 2004;54(10):534–536.
23. Burgoyne LN, O’Flynn S, Boylan GB. Undergraduate medical research: the student perspective. Med Educ Online. 2010;15:5212. doi:10.3402/meo.v15i0.5212
24. Amgad M, Man Kin Tsui M, Liptrott SJ, Shash E. Medical student research: an integrated mixed-methods systematic review and meta-analysis. PLoS One. 2015;10(6):e0127470. doi:10.1371/journal.pone.0127470
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Faculty and Students’ Perceptions About Online Teaching Styles of Faculty in Large Group Lectures
Malay J, Kassab SE, Merghani TH, Rathan R, Sreejith A
Advances in Medical Education and Practice 2022, 13:1261-1266
Published Date: 6 October 2022
Impact of a Preclinical Medical Student Anesthesiology Elective on the Attitudes and Perceptions of Medical Students Regarding Anesthesiology
Walsh KL, Yadav A, Cradeur M, Huang H, Lee D, Owusu-Dapaah H, Ji C, Kendall MC, Asher S
Advances in Medical Education and Practice 2023, 14:1347-1355
Published Date: 29 November 2023
What Matters Most: Determinants Associated with the Selection of Medical Residencies in Qatar
Kane T, Ford J, Al Saady RM, Vranic S, Musa OAH, Suliman S
Advances in Medical Education and Practice 2024, 15:141-151
Published Date: 28 February 2024
Crafting Tomorrow’s Medical Leaders: Insights from Medical Students and Interns in Saudi Arabia
Albednah FA, Albishri SB, Alnader RY, Alwazzan L
Journal of Healthcare Leadership 2024, 16:141-156
Published Date: 13 March 2024
Integrating Psychological Care Training in Trauma Care for Medical Students: the Need and the Strategies
Shrivastava SR, Shrivastava PS, Joshi A
Advances in Medical Education and Practice 2024, 15:447-450
Published Date: 27 May 2024

