Back to Journals » Advances in Medical Education and Practice » Volume 16
Paramedics Satisfaction with Simulation Experience for Career Development and Skills Maintenance
Authors Alshibani A , Alburaidi AS, Alsukait MA, Albadr R, Alsubaie BK, Almutairi A, Almutairi S, AlHussaini Z
Received 31 May 2024
Accepted for publication 7 February 2025
Published 19 February 2025 Volume 2025:16 Pages 245—253
DOI https://doi.org/10.2147/AMEP.S480813
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Abdullah Alshibani,1– 3 Abdulhakim Saad Alburaidi,2,3 Munirah Ali Alsukait,2,4 Reema Albadr,2,3 Bader Khalid Alsubaie,2,3 Ahmed Almutairi,2,3 Shujaa Almutairi,2,3 Zainab AlHussaini1,2,5
1Emergency Medical Services Department, College of Applied Medical Services, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 2King Abdullah International Medical Research Center (KAIMRC), Riyadh, Saudi Arabia; 3Department of Emergency Medical Services, King Abdulaziz Medical City, Riyadh, Saudi Arabia; 4College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 5Emergency Medicine Department, King Abdulaziz Medical City, Riyadh, Saudi Arabia
Correspondence: Abdullah Alshibani, Emergency Medical Services Department, College of Applied medical Services, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia, Email [email protected]
Introduction: Due to the importance of medical simulation as part of continuous professional development, we developed a specialized 12-month simulation program for Emergency Medical Services (EMS) personnel working at King Abdulaziz Medical City (KAMC), aiming to develop and maintain their clinical practice skills for various trauma/medical emergencies. This study, therefore, aimed to assess the level of satisfaction and experience with the developed simulation program to guide current and future simulation programs designed for EMS personnel.
Methods: A descriptive cross-sectional design was employed where an online survey was distributed to all EMS personnel at KAMC. Demographics, professional information, and satisfaction with simulation experience using the validated Satisfaction with Simulation Experience Scale (SSES) were collected from all participants. Descriptive and correlation analyses were performed to assess the effectiveness of the implemented simulation program.
Results: Of the 71 invited EMS personnel, 63 (88.7%) completed the survey. Most participants were males (88.9%) with less than 5-year experience (54%). The results showed high mean scores for all scale items, ranging from 4.44 to 4.63 on a scale of 1 to 5, with standard deviations ranging from 0.58 to 0.86. The correlation analyses showed no significant associations between demographics and professional information with simulation experience and satisfaction level.
Conclusion: These findings suggested that the simulation-based continuing professional development program at KAMC is effective in contributing to the professional development and skill enhancement of EMS personnel. Further, larger scale studies are needed to assess the effectiveness of simulation programs for EMS personnel.
Keywords: education, training, simulation, prehospital, emergency, ambulance
Introduction
Simulation is considered a broad term used to describe an instructional technique in a variety of disciplines, though its definition is up for controversy among educational theorists. As mentioned, there is a wide range of disciplines that use simulation as an educational pedagogy.1 Lopreiato et al defined simulation as “an array of structured activities that represent actual or potential situations in education and practice”. Indeed, such activities would allow the chance for the development and enhancement of knowledge, skills, attitudes and also provide a realistic representation of actual situations in a simulated environment.2 Using simulation in medical education has several advantages. First, rather than using actual patients, simulation learning expedites the teaching and learning process by using mannequins and artificial environments that resemble reality.3 It also eliminates patient risk, enhances teaching and learning experiences, and provides an engaging, learner-centered environment.4 The use of simulation is known to improve student confidence while enabling them to acquire skills. For these reasons, using simulation in medical education and continuous professional development is considered as an effective educational strategy and, therefore, should be implemented in all fields of medicine and healthcare, including emergency medicine and emergency medical care.5
Simulated training is an integral part of paramedic education, regardless of the pathway to registration.6 It aims to assess participants’ cognitive abilities by adjusting mannequins settings based on their assessment and management of the mannequins they are working with.7 Moreover, simulation is used to build basic psycho-motor abilities at a lower cognitive level so that one can become proficient with a process or technique.8 Simulation-based refresher training was shown to actively address and improve the lack of exposure to important clinical scenarios, according to a 2017 survey of ten Australian and New Zealand ambulance service employers.9 High-quality simulation experiences can help improve training and evaluation skills for scenarios that are rarely encountered in clinical practice.9 A clear checklist for evaluation, recognizable simulation tools, well-defined learning objectives, and a debriefing session should all be included in such experiences.10 The findings of a survey of 389 paramedic programs showed all programs have access to simulation tools (often a wide variety of them), meaning that Emergency Medical Services (EMS) education is widely accessible to simulation.9
The EMS department at King Abdulaziz Medical City (KAMC) in Riyadh, Saudi Arabia, has developed and implemented a structured simulation program in January 2023 for its EMS personnel as part of their continuous professional development and education. Monthly sessions with clear topics and objectives were set for various trauma and medical emergencies. The simulation sessions were conducted using high-fidelity mannequins followed by a debriefing session at the end to reflect and discuss the cases. All EMS personnel working at KAMC were invited to these simulation sessions and were expected to attend them monthly. The program was scheduled to be over 12 months and consisted of 5 domains using case-based curriculum. These domains were airway, breathing, circulation, trauma, and mega codes/trouble shooting. This study, therefore, aimed to assess the level of satisfaction with simulation experience for EMS personnel working at KAMC post one year of continuous professional development and education through formal simulation training.
Methods
This study employed a descriptive cross-sectional design to explore the effectiveness of simulation for EMS personnel through assessing their level of satisfaction with the simulation experience as part of their continuous education and career development. The study was conducted at the EMS department at KAMC in Riyadh, Saudi Arabia. KAMC has its own EMS system that responds to both emergency and low equity cases in and outside of the hospital along with critical care transfers. Consisting of approximately 120 employees, it has a large coverage area that includes housing, military bases, university campus, and two remote clinics. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) of King Abdullah International Medical Research Center (KAIMRC) (IRB approval no.: IRB/0232/24).
All EMS personnel working at the EMS department at KAMC who attended the simulation sessions were invited to participate in this study. Students and interns who attended these sessions were excluded. A total of 71 certified prehospital care personnel (paramedics and emergency medical technicians) attended the simulation sessions over a 12-month period. They were all invited through Email to complete the online survey. No sampling technique was applied as all prehospital care personnel were invited to participate in this study. A Consent form was obtained from all participants prior to completing the survey. Participants’ privacy and confidentiality were protected at all stages of the study as no personal information was collected from any participant, all responses were kept secured on a university desktop with a private network, and only the principal investigator had access to the collected data.
A structured simulation program was conducted over a 12-month period using a manikin-based training. The program consisted of several medical and trauma emergency cases where high- and low-fidelity simulation was applied based on the objectives of each simulation session. Every month, a single day event with general theme, for example cardiac emergencies, and clear objectives was conducted. An invitation letter with the name of the theme and its objectives was distributed early every month to all prehospital care personnel to attend. On the day of the simulation session, a pre-briefing was performed explaining the theme and objectives, discussion about the expectations, providing information about how the simulation will be conducted in that day, and highlighting that simulation is a safe learning environment. After each simulation case in the day, a debriefing was conducted to reflect on the performance of the participants, identify potential gaps, explore the rationale of the participants’ behaviors, and seek solutions to improve the assessment and management of the cases in the prehospital care settings. The participants in this study assessed their satisfaction with simulation experience as this is the first initiative in Saudi Arabia, to our knowledge, that include the use of structured simulation program as part of continuous education for prehospital care personnel.
Using online surveys generated by Google Forms, demographic information including age, gender, level of education, area of specialization, place of graduation, professional classification, primary role, work experience, years of experience, and prior simulation experiences were collected. Data regarding level of satisfaction with the simulation experience was collected using the Satisfaction with Simulation Experience Scale (SSES) which is a validated, multidimensional, 18-item scale that rated the employee’s agreement with each item on a 5-point Likert scale. Despite that it was originally developed by nursing researchers at the University of Newcastle in the United Kingdom, the SSES can be implemented in healthcare specialties and different cultural backgrounds. The survey went under face validity where seven paramedics (two senior paramedics holding a Ph.D. degree, one paramedic holding a master’s degree, and four paramedics holding a bachelor’s degree) assessed the question flow, clarity, and logical reasoning of the questions to support the study aim. No major changes were made after the face validity of the survey. Clear and unified instructions were given to all data collectors about the targeted population, the study’s aim, and the collection methods to reduce the risk of bias.
Data was collected using EXCEL sheets and then converted to the Statistical Package for the Social Sciences (SPSS) for analysis. Descriptive analysis including mean and Standard Deviation (SD) for continuous variables, and frequency and proportions for categorical variables was used to summarize demographics and professional information and SSES data. Along with Cronbach’s Alpha, percentages and frequencies were utilized for reliability analysis and factor loadings for factor analysis. Mean scores were calculated to assess the overall satisfaction rate of participants. Additionally, Pearson correlation was performed to examine the association between demographics/professional information and overall satisfaction/experience level with simulation and when stratified by sections including debriefing and reflection, clinical reasoning, and clinical learning.
Results
Demographics and Professional Information
A total of 71 prehospital care personnel were invited to complete the survey, 63 (88.7%) of them completed the survey. Most participants were males (88.9%) and aged 26–30 years (39.7%). The majority of participants hold bachelor’s degree and are specialized in EMS (63.5% and 95.2% respectively). Seventy-three percent of the participants were paramedics and more commonly (68.3%) work as Advanced Life Support (ALS) ground crew. The most common place of graduation was Saudi governmental universities (61.9%). A summary of the participants’ demographics is presented in Table 1.
 |
Table 1 Demographic Information |
With regards to professional information, most participants had less than five years of experience in a medical setting (54.0%) (Table 2). More than 71% of the participants had prior work experience before joining the EMS service at KAMC (Table 2). Similarly, most had received formal training before joining the EMS service at KAMC (58.7%) (Table 2).
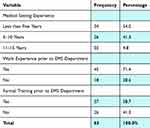 |
Table 2 Work Experience and Training |
Reliability Analysis and Factor Loadings for Factor Analysis
The Cronbach’s alpha value of the instrument is 0.962, which indicates a high level of internal consistency of the measuring instrument. Similarly, the factorability of the 18 items was examined using the Principal Component Analysis (PCA) extraction method. All items had factor loading values above the accepted value of 0.7. Only four items had scores between 0.5 and 0.7, which is also acceptable Given the Cronbach’s alpha and the item loadings, factor analysis of the scale was considered appropriate for this study (See Supplementary File 1).
Satisfaction With Simulation Experience
The participants reported high level of satisfaction with simulation experience, ranging from 4.44 to 4.63 on a 5-point Likert scale of 1 to 5, with Standard Deviations (SD) ranging from 0.58 to 0.86 (Table 3). Paramedics rated their experience and learning highly and positively in terms of debriefing and reflection (4.55), clinical reasoning (4.48), learning (4.53), and overall satisfaction and learning experience with simulation (4.53) (Table 3).
 |
Table 3 Mean (SD) of Satisfaction Level With Simulation Experience Based on 5-Point Likert Scale |
Correlation Between Demographics/Professional Information and Satisfaction Level With Simulation Experience
The correlation coefficients between Demographics and professional information including gender, education, place of graduation, professional classification, primary role, previous work experience, years working in a medical environment, previous formal training, and experience/satisfaction with simulation learning were assessed for statistical significance at assessed using Pearson correlation. The findings showed no significance of the 0.01 or 0.05 level (2-tailed). The findings showed no significant associations between demographics and professional information with overall simulation experience and when stratified by sections (debrief and reflection, clinical reasoning, and clinical learning) (see Supplementary File 1).
Discussion
The findings of this study revealed that the integration of simulation as part of continuous professional development for EMS personnel has resulted in a positive experience and high level of satisfaction among the participants. This positive simulation experience spanned across various sections of the program, including debriefing and reflection, clinical reasoning, and clinical learning. Furthermore, the satisfaction levels were not significantly associated with demographic and professional information variables, indicating a broad acceptance and appreciation of the simulation program despite professional levels. The high mean scores for all scale items, ranging from 4.44 to 4.63 on a 5-point Likert scale, emphasize the effectiveness of the simulation program in meeting the educational needs and expectations of EMS personnel. These findings suggested that the simulation-based training provided an engaging and effective learning environment conducive to enhancing EMS personnel skills and competencies. Participants felt that the facilitators provided constructive criticism and feedback during the debriefing sessions, which helped to develop their clinical reasoning skills, and identified any strengths or weaknesses.
This study employed an exploratory research design since it seeks to understand both the simulation and satisfaction experiences of EMS practitioners working in KAMC after a year of continuous education through simulation. This type of research design has been shown to be effective in the identification of correlations and patterns in fields with low previous studies.11 Moreover, this study is a quantitative descriptive paper relying on a survey to collect data from EMS personnel appropriate for assessing their experience and satisfaction level with regards to debriefing and reflection, clinical reasoning, and clinical learning after one year of continuous simulation. The data collection method is thought to be a suitable technique since according to Babbie,12 surveys are an affordable way to gather data that can be used to reach a large number of individuals, which makes them an ideal tool for researching the preferences and behaviour of people. Furthermore, Babbie12 emphasized the use of questionnaires in gathering data since they provide an organized approach that guarantees comparability and consistency in responses.
EMS personnel must respond quickly and accurately to a variety of critical scenarios due to the dynamic and high-stakes nature of the field. Therefore, they are frequently exposed to a variety of unforeseen risks and stressors leading them to make quick decisions and carry out procedures in complicated situations.13 Emergency response training provided by simulation holds the potential to improve and revolutionize EMS practice and education for EMS personnel. In fact, an essential and effective method for raising patient safety is simulation.14 Longitudinal simulation training has been shown to improve learner competency,15 while frequent simulation among EMS personnel has been effective in improving the prehospital accuracy in disaster triage field.16
In our simulation program, a manikin-based simulation was applied using both high and low fidelity simulation to create a virtual environment for the participants to practice how to assess and manage common medical and trauma emergencies. A study conducted by Leszczyński et al17 tested virtual environments (computer-based training) as a recent interactive practice of resuscitation assessments. They declared that technology-enhanced learning had the potential to provide novel solutions to alleviate the shortages in simulation-based rescue training.17 Another recent study showed that the integration and utilization of Artificial Intelligence (AI) in the emergency healthcare education including medical simulation could offer transformative potential in emergency care education and provide innovative solutions.18 Other studies assessed the use of cadavers in simulation training for prehospital care personnel.19,20 One study by Leszczyński et al showed that cadaver-based training had the potential to greatly improve the abilities of prehospital care personnel by offering a tactile and realistic learning environment that complements conventional simulation techniques.19 In addition, the usefulness of employing cadavers to teach auscultation techniques was demonstrated by Bakalarski et al,20 highlighting the significance of a variety of simulation tools in all-encompassing EMS education. The overall findings from the studies assessing medical simulation for prehospital care personnel showed that different techniques are applied (manikin-based education, computer-based training, AI-based education, and cadaver-based training). All of which were shown to have the potential to improve education and enhance training and experience for prehospital care personnel.
The significance of this study lies in its contribution to the existing body of knowledge on the effectiveness of simulation training in EMS education. By demonstrating high levels of satisfaction among paramedics with the simulation experience, this study supports the continued use and development of simulation programs for EMS personnel. This is crucial for ensuring that EMS personnel are well-prepared to meet the demands of their roles, ultimately leading to improved patient-centred care and outcomes.
While the study provides valuable insights, it also acknowledges certain limitations. One of the strengths of this study is that no study has been explicitly conducted to investigate the level of satisfaction of Saudi Arabian EMS workers with simulation training. This postulates that there is a significant gap in the research, which our study is attempting to fill. To the best of our knowledge, this is the first study to examine how satisfied EMS staff are with simulation training in this setting. However, the findings of our study showed that there were lack of significant associations between paramedics’ experience and satisfaction levels with demographic and professional information variables suggests the need for further research to explore other potential factors that may influence satisfaction with simulation training.
Additionally, the study’s context and sample size conducted within a single medical city in Saudi Arabia, which may limit the generalizability of the findings. Future research could involve multiple sites and diverse EMS settings to enhance the applicability of the results. Given the positive outcomes observed, future research could include longitudinal studies to examine the long-term impact of simulation training on paramedics’ career progression and patient care practices. Exploring the integration of simulation training with other educational strategies could also offer insights into the most effective approaches for EMS education. Additionally, qualitative studies could provide a deeper understanding of paramedics’ experiences with simulation training, shedding light on areas for further improvement.
Conclusion
In conclusion, the study underscores the value of simulation-based training in the EMS field. The findings of the study supported the strategic use of simulation programs to enhance and maintain the skills of EMS personnel, as participants in this study reported positive feedback and high level of satisfaction with research experience. Demographics and professional information of the participants were not significantly associated with the satisfaction level with simulation experience, indicating a broad acceptance and appreciation of the simulation program despite professional levels. By continuing to explore and refine simulation training, EMS education can evolve to meet the challenges of the modern healthcare, ultimately leading to better patient care and outcomes.
Acknowledgment
We extend our heartfelt appreciation to the dedicated EMS personnel who generously devoted their time to participate in our simulation program and kindly completed our survey. Moreover, we express gratitude to both the KAMC Emergency Medical Services and Pediatric simulation departments, with whom we collaborated to successfully execute our simulation program.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research is funded by King Abdullah International Medical Research Center. The role of this funding is to cover publication fees for open access.
Disclosure
The Authors declare that there is no conflicts of interest.
References
1. Wheeler B, Dippenaar E. The use of simulation as a teaching modality for paramedic education: a scoping review. British Paramedic J. 2020;5(3):31–43. doi:10.29045/14784726.2020.12.5.3.31
2. Lioce L. Healthcare Simulation Dictionary. Rockville: Agency for Healthcare Research and Quality; 2020.
3. Strachan H, Campbell P, Hoskins G. Emergency care practitioner students’ satisfaction with simulation across two universities in South Africa. Inter J Nurs Stud. 2019;104. doi:10.1016/j.ijnurstu.2019.103443
4. Jeffries PR. A framework for designing, implementing, and evaluating: simulations used as teaching strategies in nursing. Nurse Educ Pers. 2005;26(2):96–103.
5. Dreifuerst KT. The essentials of debriefing in simulation learning: a concept analysis. Nurse Educ Pers. 2009;30(2):109–114.
6. National Highway Traffic Safety Administration (NHTSA). EMS education standards. 2021. Available from: https://www.ems.gov/assets/EMS_Education-Standards_2021_FNL.pdf.
7. Cannon-Bowers JA. Recent advances in scenario-based training for medical education. Curr Opin Anesthesiol. 2008;21(6):784–789. doi:10.1097/ACO.0b013e3283184435
8. Al-Elq AH. Simulation-based medical teaching and learning. J Family Commun Med. 2010;17(1):35–40. doi:10.4103/1319-1683.68787
9. Green A, Hug M. Simulation training and skill assessment in EMS. 2022.
10. Cicero MX, Brown L, Overly F, et al. Creation and Delphi-method refinement of pediatric disaster triage simulations. Prehosl Emerg Care. 2014;18(2):282–289. doi:10.3109/10903127.2013.856505
11. Vogt WP. Quantitative versus qualitative is a distraction: variations on a theme by Brewer and Hunter (2006). Method Innov Online. 2008;3(1):18–24. doi:10.4256/mio.2008.0007
12. Babbie ER. The Practice of Social Research. Cengage AU; 2020.
13. Sterud T, Ekeberg Ø, Hem E. Health status in the ambulance services: a systematic review. BMC Health Serv Res. 2006;6(1):1–10. doi:10.1186/1472-6963-6-82
14. Kothari K, Zuger C, Desai N, et al. Effect of repetitive simulation training on emergency medical services team performance in simulated pediatric medical emergencies. AEM Educ Tra. 2021;5(3):e10537. doi:10.1002/aet2.10537
15. Pusic MV, Kessler D, Szyld D, Kalet A, Pecaric M, Boutis K. Experience curves as an organizing framework for deliberate practice in emergency medicine learning. Acad Emergency Med. 2012;19(12):1476–1480. doi:10.1111/acem.12043
16. Cicero MX, Whitfill T, Overly F, et al. Pediatric disaster triage: multiple simulation curriculum improves prehospital care providers’ assessment skills. Prehos Emerg Care. 2017;21(2):201–208. doi:10.1080/10903127.2016.1235239
17. Leszczyński P, Charuta A, Kołodziejczak B, Roszak M. Evaluation of virtual environment as a form of interactive resuscitation exam. New Revi Hypermed Multimed. 2017;23(4):265–276. doi:10.1080/13614568.2017.1421717
18. Furey P, Town A, Sumera K, Webster CA. Approaches for integrating generative artificial intelligence in emergency healthcare education within higher education: a scoping review. Criti Care Innov. 2024;7(2):34–54.
19. Leszczyński P, Muraczyńska B, Wejnarski A, Baczewska B, Malm M, Drop B. Improving the quality of training paramedics by means of cadavers–a pilot study. BMC Med Edu. 2021;21(1):1–8. doi:10.1186/s12909-021-02498-x
20. Bakalarski P, Klepacka M, Sówka K, et al. Cadaver as a didactic tool for auscultating lung sounds. Criti Care Innov. 2019;2(3):11–18.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Just-in-Time, Just-in-Place Virtual Training in the Pediatric Emergency Department: A Novel Approach to Impact the Perfusion Exam

Shah AS, Sobolewski B, Chon S, Cruse B, Glisson MD, Zackoff MW, Davis D, Zhang Y, Schumacher DJ, Geis GL
Advances in Medical Education and Practice 2023, 14:901-911
Published Date: 18 August 2023
Exploring Endoscopic Competence in Gastroenterology Training: A Simulation-Based Comparative Analysis of GAGES, DOPS, and ACE Assessment Tools
Ismail FW, Afzal A, Durrani R, Qureshi R, Awan S, Brown MR
Advances in Medical Education and Practice 2024, 15:75-84
Published Date: 31 January 2024
Factors Influencing Occupational Stress Perceived by Emergency Nurses During Prehospital Care: A Systematic Review
Montero-Tejero DJ, Jiménez-Picón N, Gómez-Salgado J, Vidal-Tejero E, Fagundo-Rivera J
Psychology Research and Behavior Management 2024, 17:501-528
Published Date: 13 February 2024
A Modular Cataract Surgery Training Model Incorporating Human Factors and a Pedagogical Theory
Mansoor Q, Qurashi N, Chen Y
Clinical Ophthalmology 2024, 18:1171-1180
Published Date: 1 May 2024
Impact of Simulation-Based Surgical Training in Laparoscopy on Satisfaction Level and Proficiency in Surgical Skills
Mukhtar F, Shaheen MF, Alhabeeb AY, Zafar M, Alkattan K
Advances in Medical Education and Practice 2025, 16:357-366
Published Date: 27 February 2025

